Monday Poster Session
Category: Esophagus
P2854 - A Rare Case of Synchronous Esophageal Squamous Cell Carcinoma: Implications of Molecular Testing for Prognosis, Clonality, and Targeted Therapy
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FL
Felicia Lee, MD
Boston Medical Center
Boston, MA
Presenting Author(s)
Felicia Lee, MD1, Vanessa Avalone, MD1, Marya Pulaski, MD1, Michael Waisberg, MD, PhD2, Horst C. Weber, MD3
1Boston Medical Center, Boston, MA; 2VA Providence Health Care System, Providence, RI; 3VA Boston Healthcare System, Jamaica Plain, MA
Introduction: Esophageal squamous cell carcinoma (ESCC) is far more common in Asia, while esophageal adenocarcinoma is more common in the U.S. Synchronous SCC (SSCC) is a rare subtype involving multiple primary tumors, separated by normal mucosa, arising simultaneously in the esophagus. It is particularly infrequent in Western countries and may be associated with different risk factors and worse long-term survival than solitary SCC. We present a rare case of double SSCC whereby molecular profiles of both tumors were analyzed using next generation sequencing (NGS), highlighting the growing importance of precision oncology.
Case Description/
Methods: A 72-year-old male with history of alcohol, opioid, and chronic tobacco use disorder presented with worsening dysphagia. A diagnostic EGD showed a circumferential friable mass lesion in the mid-esophagus and a distinctly separate semi-circumferential ulcerated lesion in the distal esophagus (Fig.1). Biopsies confirmed both lesions as moderately to poorly differentiated SCC and illustrate the positive immunohistochemistry (IHC) analyses of these lesions for PD-L1 (Fig 1). NGS revealed a combined positive score of 1 and 20 for the proximal and distal lesions, respectively, in addition to stable microsatellite status, suggestive of poor response to immunotherapy. Both tumors shared typical driver mutations in TP53, CDKN2A/B, and TET2 genes, whereas some non-driver mutations (ASXL1, NFKB1A, NSD3) were only detected in the proximal but not the distal tumor (Table 1). The patient was diagnosed with T3N2M0 disease and underwent neoadjuvant chemoradiation. However, he developed significant complications and was not a candidate for further active therapy.
Discussion: NGS provided important insight into characterizing the intra-tumor heterogeneity in this very rare case of SSCC. Common driver mutations were found in both tumors, supporting the “field cancerization” theory in which widespread epithelial injury from carcinogens like chronic tobacco and alcohol use can lead to a pre-malignant field with genetic instability. However, the presence of additional mutations in the proximal lesion supports the idea of a branched common progenitor clone. Evidence of these two models suggest that while the tumors are not metastatic, they are also not completely independent. Therefore, NGS offers a more comprehensive understanding of tumor clonality with a particularly critical impact on the actionability and development of targeted therapies in esophageal SCC.
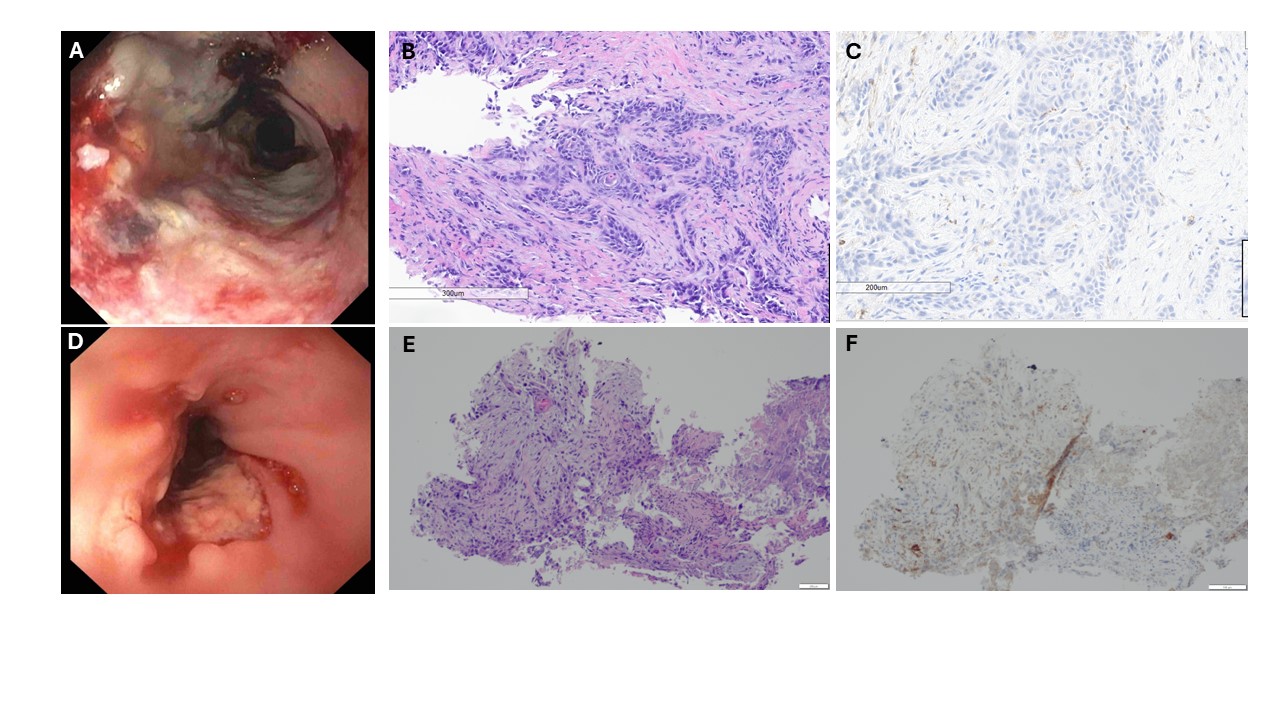
Figure: Figure 1. (Top Row, A-C) Proximal tumor seen at 25 cm in the mid-esophagus: A) Endoscopic image. B) H&E staining. C) Immunohistochemistry staining for PD-L1. (Bottom Row, D-F) Distal tumor of the esophagus: D) Endoscopic image. E) H&E staining. F) Immunohistochemistry staining for PD-L1.

Figure: Table 1: Columns 1-2: Frequently reported genetic mutations in ESCC and in this case with their respective functions. Columns 3-6: Molecular profiles of the patient’s proximal and distal esophageal tumors using FoundationMedicineR next generation sequencing.
Disclosures:
Felicia Lee indicated no relevant financial relationships.
Vanessa Avalone indicated no relevant financial relationships.
Marya Pulaski indicated no relevant financial relationships.
Michael Waisberg indicated no relevant financial relationships.
Horst Weber indicated no relevant financial relationships.
Felicia Lee, MD1, Vanessa Avalone, MD1, Marya Pulaski, MD1, Michael Waisberg, MD, PhD2, Horst C. Weber, MD3. P2854 - A Rare Case of Synchronous Esophageal Squamous Cell Carcinoma: Implications of Molecular Testing for Prognosis, Clonality, and Targeted Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Boston Medical Center, Boston, MA; 2VA Providence Health Care System, Providence, RI; 3VA Boston Healthcare System, Jamaica Plain, MA
Introduction: Esophageal squamous cell carcinoma (ESCC) is far more common in Asia, while esophageal adenocarcinoma is more common in the U.S. Synchronous SCC (SSCC) is a rare subtype involving multiple primary tumors, separated by normal mucosa, arising simultaneously in the esophagus. It is particularly infrequent in Western countries and may be associated with different risk factors and worse long-term survival than solitary SCC. We present a rare case of double SSCC whereby molecular profiles of both tumors were analyzed using next generation sequencing (NGS), highlighting the growing importance of precision oncology.
Case Description/
Methods: A 72-year-old male with history of alcohol, opioid, and chronic tobacco use disorder presented with worsening dysphagia. A diagnostic EGD showed a circumferential friable mass lesion in the mid-esophagus and a distinctly separate semi-circumferential ulcerated lesion in the distal esophagus (Fig.1). Biopsies confirmed both lesions as moderately to poorly differentiated SCC and illustrate the positive immunohistochemistry (IHC) analyses of these lesions for PD-L1 (Fig 1). NGS revealed a combined positive score of 1 and 20 for the proximal and distal lesions, respectively, in addition to stable microsatellite status, suggestive of poor response to immunotherapy. Both tumors shared typical driver mutations in TP53, CDKN2A/B, and TET2 genes, whereas some non-driver mutations (ASXL1, NFKB1A, NSD3) were only detected in the proximal but not the distal tumor (Table 1). The patient was diagnosed with T3N2M0 disease and underwent neoadjuvant chemoradiation. However, he developed significant complications and was not a candidate for further active therapy.
Discussion: NGS provided important insight into characterizing the intra-tumor heterogeneity in this very rare case of SSCC. Common driver mutations were found in both tumors, supporting the “field cancerization” theory in which widespread epithelial injury from carcinogens like chronic tobacco and alcohol use can lead to a pre-malignant field with genetic instability. However, the presence of additional mutations in the proximal lesion supports the idea of a branched common progenitor clone. Evidence of these two models suggest that while the tumors are not metastatic, they are also not completely independent. Therefore, NGS offers a more comprehensive understanding of tumor clonality with a particularly critical impact on the actionability and development of targeted therapies in esophageal SCC.
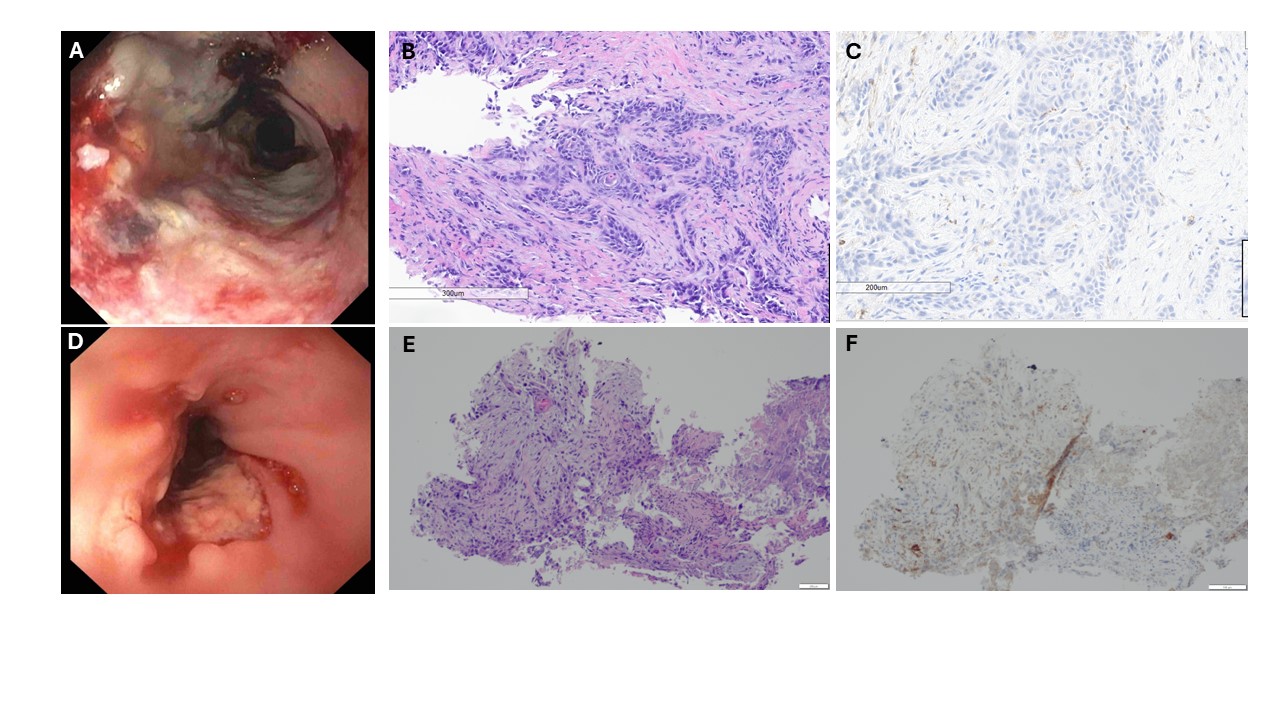
Figure: Figure 1. (Top Row, A-C) Proximal tumor seen at 25 cm in the mid-esophagus: A) Endoscopic image. B) H&E staining. C) Immunohistochemistry staining for PD-L1. (Bottom Row, D-F) Distal tumor of the esophagus: D) Endoscopic image. E) H&E staining. F) Immunohistochemistry staining for PD-L1.

Figure: Table 1: Columns 1-2: Frequently reported genetic mutations in ESCC and in this case with their respective functions. Columns 3-6: Molecular profiles of the patient’s proximal and distal esophageal tumors using FoundationMedicineR next generation sequencing.
Disclosures:
Felicia Lee indicated no relevant financial relationships.
Vanessa Avalone indicated no relevant financial relationships.
Marya Pulaski indicated no relevant financial relationships.
Michael Waisberg indicated no relevant financial relationships.
Horst Weber indicated no relevant financial relationships.
Felicia Lee, MD1, Vanessa Avalone, MD1, Marya Pulaski, MD1, Michael Waisberg, MD, PhD2, Horst C. Weber, MD3. P2854 - A Rare Case of Synchronous Esophageal Squamous Cell Carcinoma: Implications of Molecular Testing for Prognosis, Clonality, and Targeted Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
