Monday Poster Session
Category: Esophagus
P2850 - Oral and Esophageal Blisters: Unusual Cause of Dysphagia
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DK
Diksha Kajal, MD
Florida State University
Cape Coral, FL
Presenting Author(s)
Diksha Kajal, MD1, Khrystyna Babenko, DMD2, Marilin Rosa, MD3, Iryna S. Hepburn, MD, FACG1
1Florida State University, Cape Coral, FL; 2Temple University Kornberg School of Dentistry, Philadelphia, PA; 3NeoGenomics Laboratories, Fort Myers, FL
Introduction: Bullous pemphigoid (BP) is an autoimmune disease that often affects the elderly, presenting with mucocutaneous bullae. We describe a patient with an unusual case of dysphagia after developing oral and esophageal bullae despite taking steroid therapy
Case Description/
Methods: 89y male presented to the ED with dysphagia and inability to manage secretions after he felt a blister in his throat. On exam, he was drooling and had painful oral bullae. He was hospitalized six weeks prior for diffuse skin blistering. Skin biopsy showed subepidermal bullae, spongiosis, and eosinophilic infiltration, confirming BP. Serum BP180 Abs were >180. He was treated with IV steroids and discharged on prednisone 50 mg/d and doxycycline 100mg/d. GI was consulted for suspected esophageal obstruction. Due to concerns of airway compromise, the patient was intubated; EGD revealed multiple hemorrhagic bullae and ulcerations in the oropharynx and esophagus. Multispecialty teams(GI, ID, ENT) were involved. Transfer to a tertiary center was attempted but declined multiple times due to lack of inpatient dermatology expertise. After prolonged hospitalization, the patient was discharged and was ultimately started on IVIG.
Discussion: BP is a rare autoimmune disorder associated with medication, skin infection or injury, or malignancy. Formation of antibodies to basal membrane proteins BP180&BP230 leads to T cell and complement activation, proteolytic enzymes release and blistering. Patients have itchy tense fluid-filled bullae that form erosions on rupture. Mucosal involvement with large sanguinous bullae and erosion is rare. Mucosal BP leads to serious morbidity and mortality in steroid resistant cases due to infectious complications. Skin biopsy shows a split under the epidermis and dermal neutrophilic infiltrate with eosinophils. Patients are initially treated with high potency topical steroids, doxycycline, and oral steroids; extensive disease requires IV steroids. Steroid sparing agents include mycophenolate, dapsone, azathioprine, and methotrexate. Refractory disease may require rituximab, dupilumab, omalizumab, and IVIG. IVIG was used successfully in our patient. Patients with mucosal BP are at risk of morbidity and mortality and require significant resources. There are few proven treatment options which are often associated with complications. Absence of inpatient dermatology expertise hinders care of these patients. Higher awareness of BP and its treatment among gastroenterologists would potentially improve outcomes.
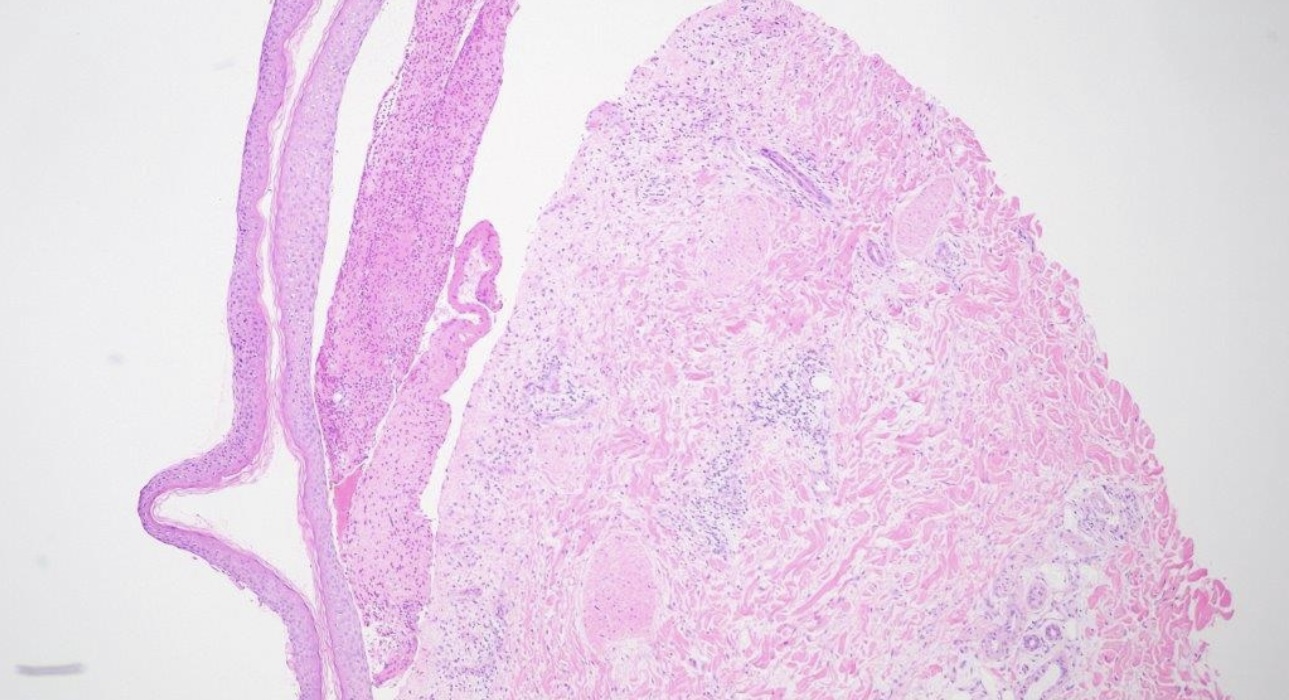
Figure: Skin Punch-10x. Subepidermal blister with accumulation of inflammatory cells, predominately eosinophils (H&E, x100)

Figure: EGD shows a hemorrhagic, tense, fluid-filled bullous lesion in the oropharynx and esophagus, consistent with mucosal involvement of BP.
Disclosures:
Diksha Kajal indicated no relevant financial relationships.
Khrystyna Babenko indicated no relevant financial relationships.
Marilin Rosa indicated no relevant financial relationships.
Iryna Hepburn indicated no relevant financial relationships.
Diksha Kajal, MD1, Khrystyna Babenko, DMD2, Marilin Rosa, MD3, Iryna S. Hepburn, MD, FACG1. P2850 - Oral and Esophageal Blisters: Unusual Cause of Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Florida State University, Cape Coral, FL; 2Temple University Kornberg School of Dentistry, Philadelphia, PA; 3NeoGenomics Laboratories, Fort Myers, FL
Introduction: Bullous pemphigoid (BP) is an autoimmune disease that often affects the elderly, presenting with mucocutaneous bullae. We describe a patient with an unusual case of dysphagia after developing oral and esophageal bullae despite taking steroid therapy
Case Description/
Methods: 89y male presented to the ED with dysphagia and inability to manage secretions after he felt a blister in his throat. On exam, he was drooling and had painful oral bullae. He was hospitalized six weeks prior for diffuse skin blistering. Skin biopsy showed subepidermal bullae, spongiosis, and eosinophilic infiltration, confirming BP. Serum BP180 Abs were >180. He was treated with IV steroids and discharged on prednisone 50 mg/d and doxycycline 100mg/d. GI was consulted for suspected esophageal obstruction. Due to concerns of airway compromise, the patient was intubated; EGD revealed multiple hemorrhagic bullae and ulcerations in the oropharynx and esophagus. Multispecialty teams(GI, ID, ENT) were involved. Transfer to a tertiary center was attempted but declined multiple times due to lack of inpatient dermatology expertise. After prolonged hospitalization, the patient was discharged and was ultimately started on IVIG.
Discussion: BP is a rare autoimmune disorder associated with medication, skin infection or injury, or malignancy. Formation of antibodies to basal membrane proteins BP180&BP230 leads to T cell and complement activation, proteolytic enzymes release and blistering. Patients have itchy tense fluid-filled bullae that form erosions on rupture. Mucosal involvement with large sanguinous bullae and erosion is rare. Mucosal BP leads to serious morbidity and mortality in steroid resistant cases due to infectious complications. Skin biopsy shows a split under the epidermis and dermal neutrophilic infiltrate with eosinophils. Patients are initially treated with high potency topical steroids, doxycycline, and oral steroids; extensive disease requires IV steroids. Steroid sparing agents include mycophenolate, dapsone, azathioprine, and methotrexate. Refractory disease may require rituximab, dupilumab, omalizumab, and IVIG. IVIG was used successfully in our patient. Patients with mucosal BP are at risk of morbidity and mortality and require significant resources. There are few proven treatment options which are often associated with complications. Absence of inpatient dermatology expertise hinders care of these patients. Higher awareness of BP and its treatment among gastroenterologists would potentially improve outcomes.
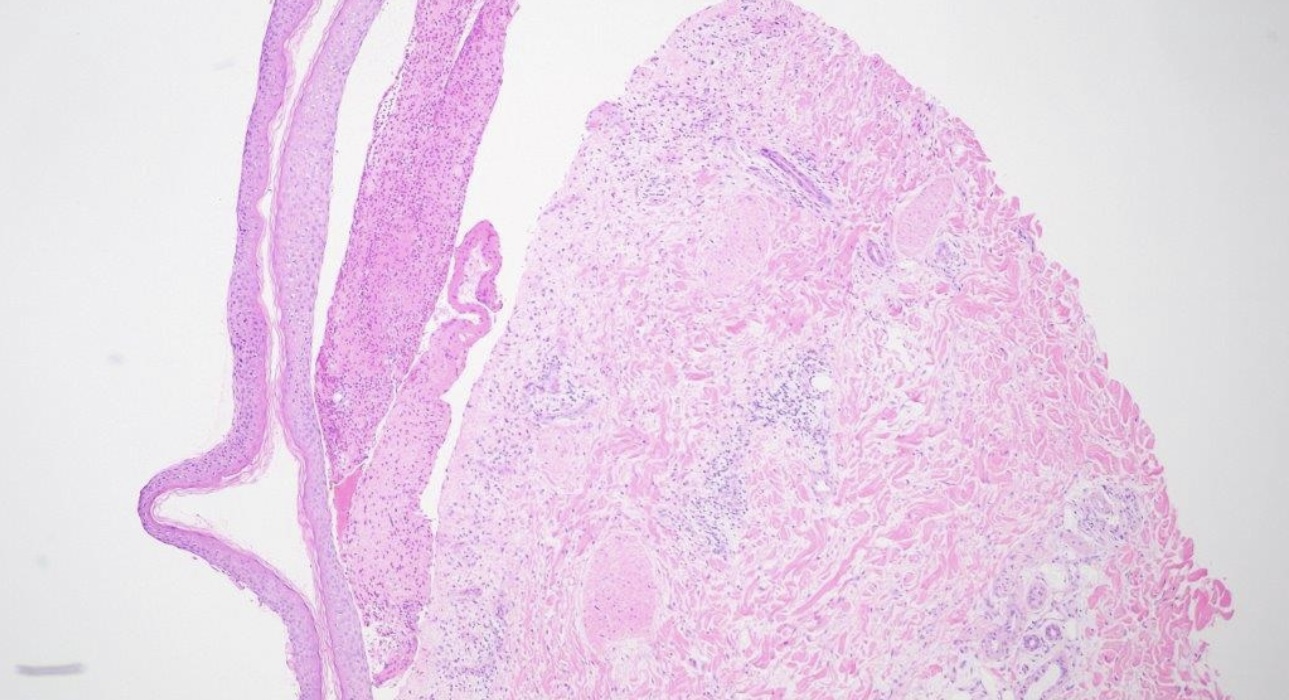
Figure: Skin Punch-10x. Subepidermal blister with accumulation of inflammatory cells, predominately eosinophils (H&E, x100)

Figure: EGD shows a hemorrhagic, tense, fluid-filled bullous lesion in the oropharynx and esophagus, consistent with mucosal involvement of BP.
Disclosures:
Diksha Kajal indicated no relevant financial relationships.
Khrystyna Babenko indicated no relevant financial relationships.
Marilin Rosa indicated no relevant financial relationships.
Iryna Hepburn indicated no relevant financial relationships.
Diksha Kajal, MD1, Khrystyna Babenko, DMD2, Marilin Rosa, MD3, Iryna S. Hepburn, MD, FACG1. P2850 - Oral and Esophageal Blisters: Unusual Cause of Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
