Monday Poster Session
Category: Esophagus
P2788 - POEM Does Not Trigger Barrett’s Esophagus: A Multicenter TriNetX Study of Barrett’s Esophagus Prevalence
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Archana Kharel, MD (she/her/hers)
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Archana Kharel, MD1, Prabhat Kumar, MD2, Umesh Bhagat, MD3, Shivali Chava, 4, Ankit Kumar, 2, Prashanthi Thota, MD3, Madhusudhan Sanaka, MD1
1Cleveland Clinic, Cleveland, OH; 2Virginia Commonwealth University, Richmond, VA; 3Cleveland Clinic Foundation, Cleveland, OH; 4The University of Texas at Austin, Houston, TX
Introduction: Per-oral endoscopic myotomy (POEM) has become the standard therapy for achalasia, but its potential to promote Barrett’s esophagus (BE) is unclear. Given the high rate of post-POEM gastroesophageal reflux disease,a known risk factor for BE, we sought to determine whether POEM independently increases BE incidence
Methods: We queried the TriNetX Research Network (99 U.S. health-care organizations) for adults ≥ 18 years with achalasia (ICD-10 K22.0) who underwent POEM (CPT 43497) between 1 May 2005 and 1 May 2025. Patients with pre-existing BE, upper-GI malignancy, eosinophilic esophagitis, pregnancy, esophagectomy, or anti-reflux surgery were excluded. The primary outcome was first-ever BE (ICD-10 K22.7) occurring ≥ 1 day post-POEM. For context we also assessed gastro-esophageal reflux with esophagitis (GERD-E: ICD-10 K21.0) as a surrogate of reflux burden. Incidence proportions and prevalences were calculated for two prespecified eras—Era 1 (1 May 2015–1 May 2020) and Era 2 (2 May 2021–1 May 2025)—with stratification by sex, race, and ethnicity.
Results: Among 1,882 POEM recipients, no incident BE occurred in either era (0/1,882; incidence 0 %, prevalence 0 %, all demographic strata 0 %). Conversely, GERD-E rose four-fold: incidence 5.8 % in Era 1 versus 22.4 % in Era 2, and prevalence 7.7 % versus 26.9 %. Women showed slightly higher GERD-E incidence than men in the recent era (23.5 % vs 21.5 %); the largest absolute increases were observed among Asian (34 %) and Black (17 %) patients.
Discussion: In this national real-world cohort spanning a decade of modern POEM practice, no cases of de novo Barrett’s esophagus were identified, despite a marked escalation in reflux-associated esophagitis. These data suggest that POEM, even in the face of increasing post-procedure reflux, does not confer measurable risk for BE within the first 10 years. Routine Barrett’s surveillance solely on the basis of prior POEM appears unwarranted; attention should instead focus on symptomatic reflux control and longer-term follow-up to confirm these reassuring findings.
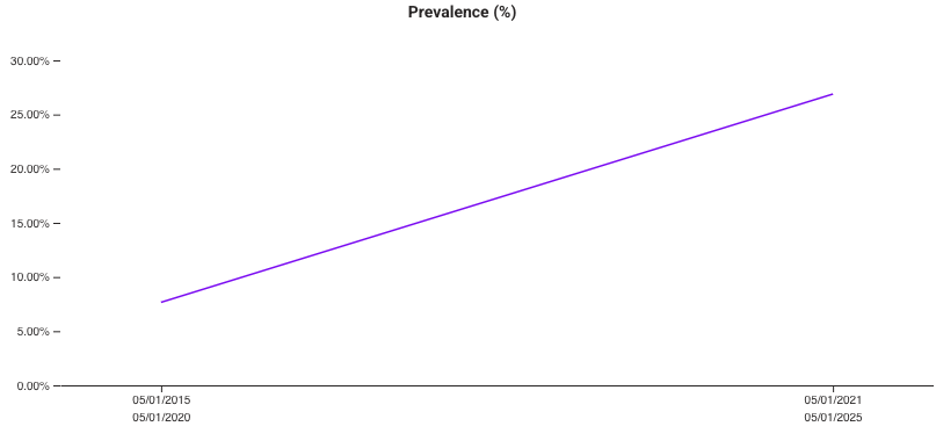
Figure: Figure 1. Post-POEM GERD Trend (2015-2025).
Prevalence of gastro-oesophageal reflux disease rose progressively in the POEM cohort, increasing from ≈8 % in 2015-2020 to ≈27 % in 2020-2025, underscoring the high burden of reflux symptoms after the procedure.
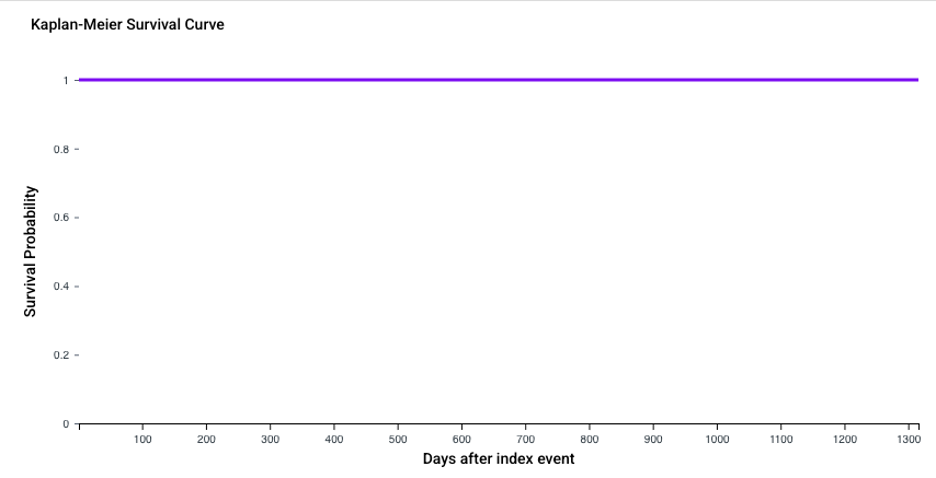
Figure: Figure 2. Kaplan–Meier Analysis of Barrett’s Esophagus After POEM.
Cumulative incidence of Barrett’s esophagus among 1,882 POEM patients remained 0 % throughout the 1,300-day follow-up, indicating no new BE diagnoses post-procedure
Disclosures:
Archana Kharel indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Shivali Chava indicated no relevant financial relationships.
Ankit Kumar indicated no relevant financial relationships.
Prashanthi Thota indicated no relevant financial relationships.
Madhusudhan Sanaka indicated no relevant financial relationships.
Archana Kharel, MD1, Prabhat Kumar, MD2, Umesh Bhagat, MD3, Shivali Chava, 4, Ankit Kumar, 2, Prashanthi Thota, MD3, Madhusudhan Sanaka, MD1. P2788 - POEM Does Not Trigger Barrett’s Esophagus: A Multicenter TriNetX Study of Barrett’s Esophagus Prevalence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Virginia Commonwealth University, Richmond, VA; 3Cleveland Clinic Foundation, Cleveland, OH; 4The University of Texas at Austin, Houston, TX
Introduction: Per-oral endoscopic myotomy (POEM) has become the standard therapy for achalasia, but its potential to promote Barrett’s esophagus (BE) is unclear. Given the high rate of post-POEM gastroesophageal reflux disease,a known risk factor for BE, we sought to determine whether POEM independently increases BE incidence
Methods: We queried the TriNetX Research Network (99 U.S. health-care organizations) for adults ≥ 18 years with achalasia (ICD-10 K22.0) who underwent POEM (CPT 43497) between 1 May 2005 and 1 May 2025. Patients with pre-existing BE, upper-GI malignancy, eosinophilic esophagitis, pregnancy, esophagectomy, or anti-reflux surgery were excluded. The primary outcome was first-ever BE (ICD-10 K22.7) occurring ≥ 1 day post-POEM. For context we also assessed gastro-esophageal reflux with esophagitis (GERD-E: ICD-10 K21.0) as a surrogate of reflux burden. Incidence proportions and prevalences were calculated for two prespecified eras—Era 1 (1 May 2015–1 May 2020) and Era 2 (2 May 2021–1 May 2025)—with stratification by sex, race, and ethnicity.
Results: Among 1,882 POEM recipients, no incident BE occurred in either era (0/1,882; incidence 0 %, prevalence 0 %, all demographic strata 0 %). Conversely, GERD-E rose four-fold: incidence 5.8 % in Era 1 versus 22.4 % in Era 2, and prevalence 7.7 % versus 26.9 %. Women showed slightly higher GERD-E incidence than men in the recent era (23.5 % vs 21.5 %); the largest absolute increases were observed among Asian (34 %) and Black (17 %) patients.
Discussion: In this national real-world cohort spanning a decade of modern POEM practice, no cases of de novo Barrett’s esophagus were identified, despite a marked escalation in reflux-associated esophagitis. These data suggest that POEM, even in the face of increasing post-procedure reflux, does not confer measurable risk for BE within the first 10 years. Routine Barrett’s surveillance solely on the basis of prior POEM appears unwarranted; attention should instead focus on symptomatic reflux control and longer-term follow-up to confirm these reassuring findings.
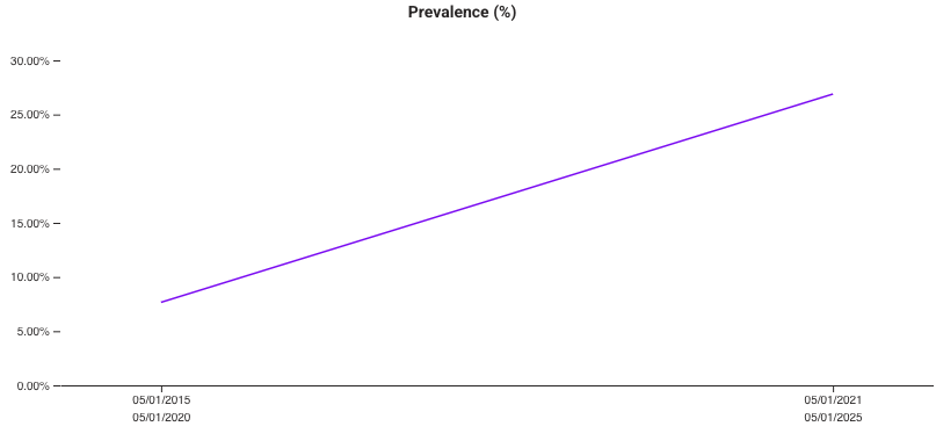
Figure: Figure 1. Post-POEM GERD Trend (2015-2025).
Prevalence of gastro-oesophageal reflux disease rose progressively in the POEM cohort, increasing from ≈8 % in 2015-2020 to ≈27 % in 2020-2025, underscoring the high burden of reflux symptoms after the procedure.
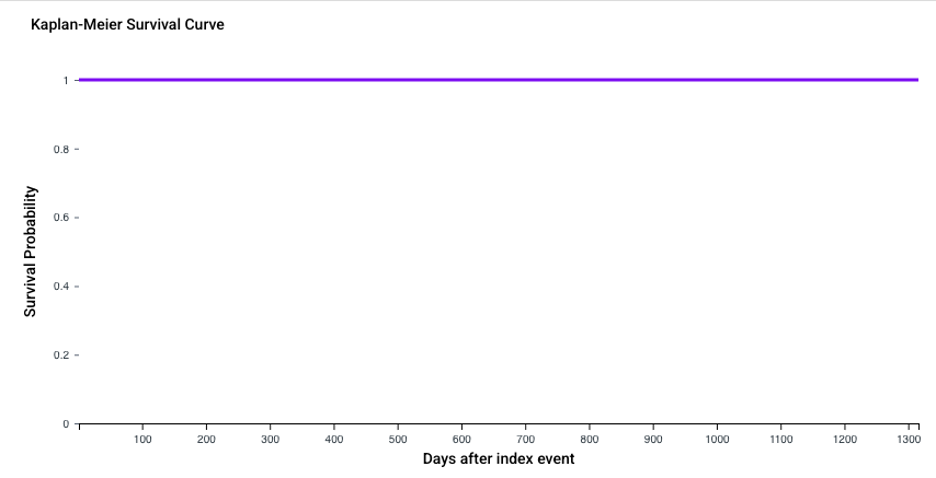
Figure: Figure 2. Kaplan–Meier Analysis of Barrett’s Esophagus After POEM.
Cumulative incidence of Barrett’s esophagus among 1,882 POEM patients remained 0 % throughout the 1,300-day follow-up, indicating no new BE diagnoses post-procedure
Disclosures:
Archana Kharel indicated no relevant financial relationships.
Prabhat Kumar indicated no relevant financial relationships.
Umesh Bhagat indicated no relevant financial relationships.
Shivali Chava indicated no relevant financial relationships.
Ankit Kumar indicated no relevant financial relationships.
Prashanthi Thota indicated no relevant financial relationships.
Madhusudhan Sanaka indicated no relevant financial relationships.
Archana Kharel, MD1, Prabhat Kumar, MD2, Umesh Bhagat, MD3, Shivali Chava, 4, Ankit Kumar, 2, Prashanthi Thota, MD3, Madhusudhan Sanaka, MD1. P2788 - POEM Does Not Trigger Barrett’s Esophagus: A Multicenter TriNetX Study of Barrett’s Esophagus Prevalence, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
