Monday Poster Session
Category: Esophagus
P2781 - Inpatient Outcomes of Alzheimer’s Dementia Patients With Dysphagia: A Nationwide Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Raj H. Patel, MD
St. Mary Medical Center
Langhorne, PA
Presenting Author(s)
Pranav Patel, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Charmy Parikh, MD4, Yash Shah, MD4, Dema Shamoon, MD1, Bradley D. Confer, DO1, Harshit S. Khara, MD5, David L.. Diehl, MD1, Danial Shaikh, MD1
1Geisinger Health System, Danville, PA; 2St. Mary Medical Center, Langhorne, PA; 3Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 4Mercy Catholic Medical Center, Darby, PA; 5Geisinger Health System, Danville, NJ
Introduction: Dysphagia is a common complication of Alzheimer’s disease dementia, contributing to malnutrition and frequent aspiration events. Patients with Alzheimer’s who develop swallowing difficulties are presumed to have higher morbidity and healthcare utilization, but large-scale data on their inpatient outcomes are limited. We aimed to evaluate the impact of dysphagia on clinical outcomes and resource use in hospitalized Alzheimer’s patients using a national inpatient database.
Methods: We analyzed the National Inpatient Sample (NIS) between 2016 and 2020, identifying all hospitalizations for patients aged ≥70 with a diagnosis of Alzheimer’s disease dementia. Cases with co-diagnosed dysphagia were identified via ICD-10 codes. We compared patient characteristics and outcomes between Alzheimer’s patients with dysphagia and those without. Primary outcomes included mortality, length of stay (LOS), and total hospital cost (THC). Secondary outcomes include endoscopic evaluation, PEG tube placement, and prevalence of aspiration pneumonia. t-Test and chi-square were utilized for analysis in SAS 9.4
Results: Among 1,965,035 patients with Alzheimer’s dementia, dysphagia was present in 205,565 cases (10.5%). Patients with dysphagia had a mean age of 83.98 years, were predominantly female (56.4%), and primarily white (65.9%). Alzheimer’s patients with dysphagia showed significantly worse outcomes than those without. Compared to patients without dysphagia, those with dysphagia had significantly higher inpatient mortality rates (7.0% vs. 4.9%, p < 0.05), longer hospital stays (mean LOS: 7.92 vs. 5.96 days, p < 0.05), and greater total hospital costs ($15,636 vs. $11,551). Aspiration pneumonia was notably more common among patients with dysphagia (27% vs. 5.4%, p< 0.05). Additionally, the dysphagia group had higher rates of upper endoscopy utilization (2.3% vs. 1.1%, p< 0.05) and PEG tube placements (675 vs. 435 cases). Baseline demographics and outcomes are summarized in Table 1
Discussion: Hospitalized Alzheimer’s disease patients with coexisting dysphagia have substantially worse inpatient outcomes and higher resource utilization than those without dysphagia. Given limited effectiveness of current interventions (e.g., thickened liquids have shown no clear mortality benefit in this population), a multidisciplinary approach and early swallowing assessments with personalized feeding strategies are essential to mitigate aspiration risks and improve outcomes.
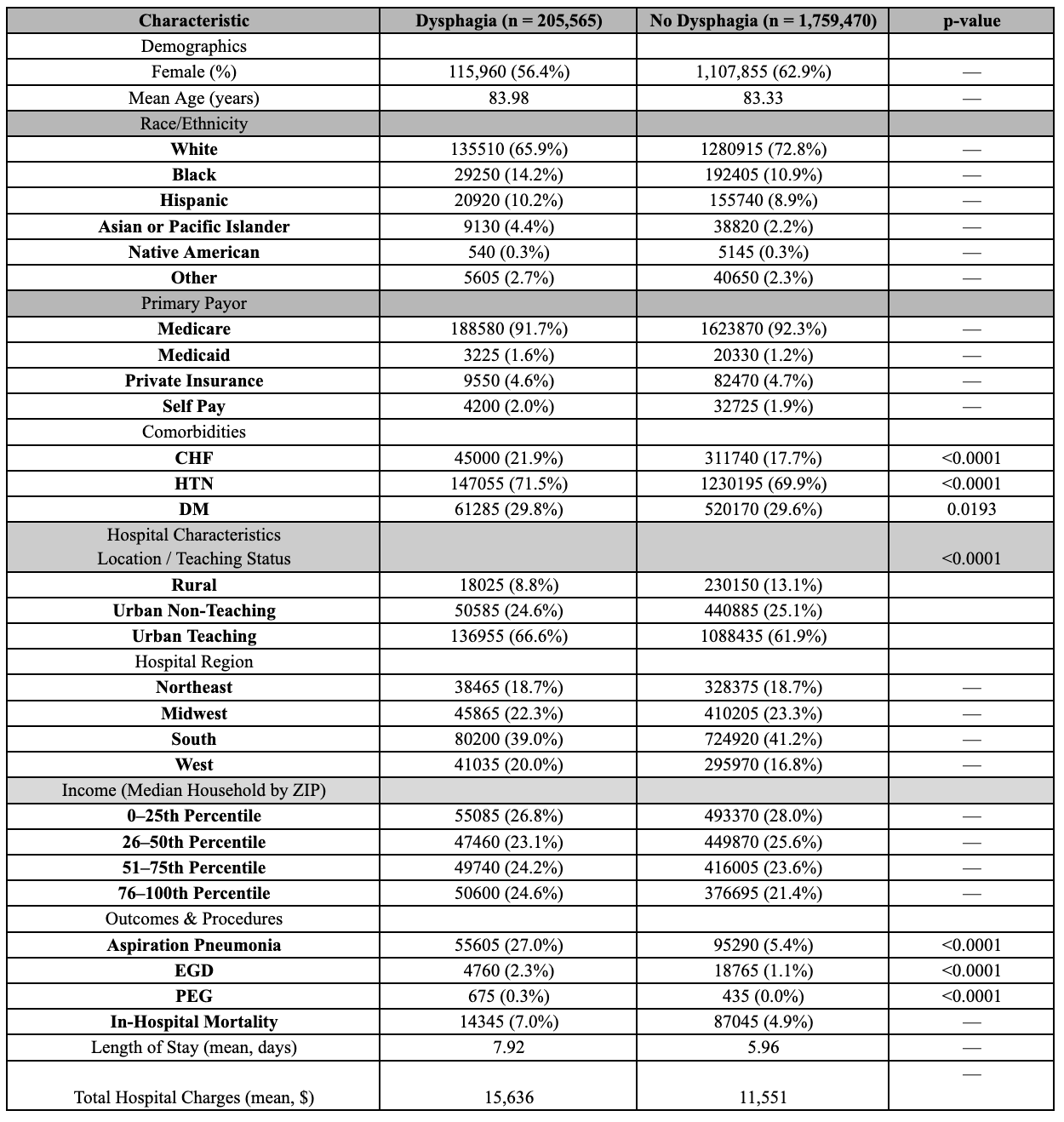
Figure: Table 1: Baseline Characteristics and Outcomes in Dementia Patients With and Without Dysphagia (National Inpatient Sample, 2016–2020)

Figure: Comparison of Key Inpatient Outcomes Among Dementia Patients With and Without Dysphagia (National
Inpatient Sample, 2016–2020).
This bar chart illustrates the significantly higher incidence of aspiration pneumonia, PEG tube placement, and
in-hospital mortality among dementia patients with dysphagia compared to those without. Patients with dysphagia
also had slightly higher rates of EGD. Error bars represent standard errors. All differences were statistically
significant (p < 0.001)
Disclosures:
Pranav Patel indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Dema Shamoon indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
David Diehl indicated no relevant financial relationships.
Danial Shaikh indicated no relevant financial relationships.
Pranav Patel, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Charmy Parikh, MD4, Yash Shah, MD4, Dema Shamoon, MD1, Bradley D. Confer, DO1, Harshit S. Khara, MD5, David L.. Diehl, MD1, Danial Shaikh, MD1. P2781 - Inpatient Outcomes of Alzheimer’s Dementia Patients With Dysphagia: A Nationwide Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Geisinger Health System, Danville, PA; 2St. Mary Medical Center, Langhorne, PA; 3Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 4Mercy Catholic Medical Center, Darby, PA; 5Geisinger Health System, Danville, NJ
Introduction: Dysphagia is a common complication of Alzheimer’s disease dementia, contributing to malnutrition and frequent aspiration events. Patients with Alzheimer’s who develop swallowing difficulties are presumed to have higher morbidity and healthcare utilization, but large-scale data on their inpatient outcomes are limited. We aimed to evaluate the impact of dysphagia on clinical outcomes and resource use in hospitalized Alzheimer’s patients using a national inpatient database.
Methods: We analyzed the National Inpatient Sample (NIS) between 2016 and 2020, identifying all hospitalizations for patients aged ≥70 with a diagnosis of Alzheimer’s disease dementia. Cases with co-diagnosed dysphagia were identified via ICD-10 codes. We compared patient characteristics and outcomes between Alzheimer’s patients with dysphagia and those without. Primary outcomes included mortality, length of stay (LOS), and total hospital cost (THC). Secondary outcomes include endoscopic evaluation, PEG tube placement, and prevalence of aspiration pneumonia. t-Test and chi-square were utilized for analysis in SAS 9.4
Results: Among 1,965,035 patients with Alzheimer’s dementia, dysphagia was present in 205,565 cases (10.5%). Patients with dysphagia had a mean age of 83.98 years, were predominantly female (56.4%), and primarily white (65.9%). Alzheimer’s patients with dysphagia showed significantly worse outcomes than those without. Compared to patients without dysphagia, those with dysphagia had significantly higher inpatient mortality rates (7.0% vs. 4.9%, p < 0.05), longer hospital stays (mean LOS: 7.92 vs. 5.96 days, p < 0.05), and greater total hospital costs ($15,636 vs. $11,551). Aspiration pneumonia was notably more common among patients with dysphagia (27% vs. 5.4%, p< 0.05). Additionally, the dysphagia group had higher rates of upper endoscopy utilization (2.3% vs. 1.1%, p< 0.05) and PEG tube placements (675 vs. 435 cases). Baseline demographics and outcomes are summarized in Table 1
Discussion: Hospitalized Alzheimer’s disease patients with coexisting dysphagia have substantially worse inpatient outcomes and higher resource utilization than those without dysphagia. Given limited effectiveness of current interventions (e.g., thickened liquids have shown no clear mortality benefit in this population), a multidisciplinary approach and early swallowing assessments with personalized feeding strategies are essential to mitigate aspiration risks and improve outcomes.
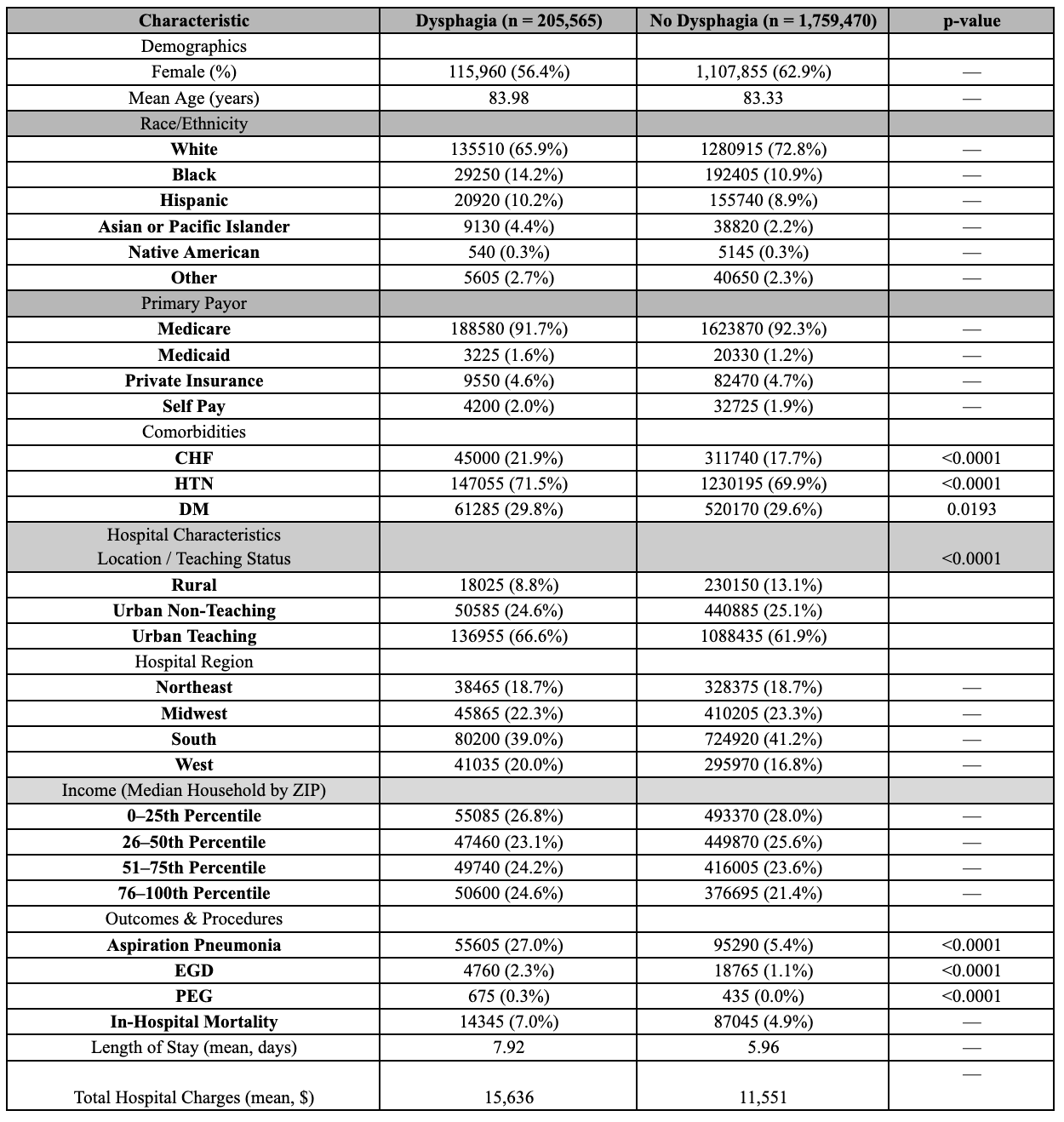
Figure: Table 1: Baseline Characteristics and Outcomes in Dementia Patients With and Without Dysphagia (National Inpatient Sample, 2016–2020)

Figure: Comparison of Key Inpatient Outcomes Among Dementia Patients With and Without Dysphagia (National
Inpatient Sample, 2016–2020).
This bar chart illustrates the significantly higher incidence of aspiration pneumonia, PEG tube placement, and
in-hospital mortality among dementia patients with dysphagia compared to those without. Patients with dysphagia
also had slightly higher rates of EGD. Error bars represent standard errors. All differences were statistically
significant (p < 0.001)
Disclosures:
Pranav Patel indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Charmy Parikh indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Dema Shamoon indicated no relevant financial relationships.
Bradley Confer indicated no relevant financial relationships.
Harshit Khara indicated no relevant financial relationships.
David Diehl indicated no relevant financial relationships.
Danial Shaikh indicated no relevant financial relationships.
Pranav Patel, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Charmy Parikh, MD4, Yash Shah, MD4, Dema Shamoon, MD1, Bradley D. Confer, DO1, Harshit S. Khara, MD5, David L.. Diehl, MD1, Danial Shaikh, MD1. P2781 - Inpatient Outcomes of Alzheimer’s Dementia Patients With Dysphagia: A Nationwide Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
