Monday Poster Session
Category: Esophagus
P2770 - Distinct Clinical Risk of Barrett’s Esophagus in Younger vs Older Adults: A Nationwide Inpatient Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Daniel Alejandro Gonzalez Mosquera, MD (he/him/his)
NYC Health + Hospitals/Lincoln
Bronx, NY
Presenting Author(s)
Daniel Alejandro. Gonzalez Mosquera, MD1, Maria Belen Mateo, MD2, Carolina Gonzalez Mosquera, MD3, Juan Martinez-Ortega, MD4, Yassine Kilani, MD5, Carla Evangelista, MD4
1NYC Health + Hospitals/Lincoln, Bronx, NY; 2Knowledge and Research Evaluation Unit, Mayo Clinic, Rochester, Minnesota, USA, Rochester, MN; 3Universidad Católica Santiago de Guayaquil, Guayaquil, Guayas, Ecuador; 4New York Health + Hospitals | Lincoln–Weill Cornell Medical College Affiliate, New York, USA, Bronx, NY; 5Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Barrett’s Esophagus (BE) has been considered a condition primarily affecting older adults, with an estimated prevalence of 5.6% among U.S. adults. It is most commonly linked to longstanding gastroesophageal reflux disease (GERD). However, recent evidence suggests a rising prevalence in younger individuals, with rates of approximately 0.06% among those aged 0–29 years and 1.6% among those aged 30–44 years. While GERD remains a central risk factor, younger patients may present with a distinct constellation of associated conditions. We aimed to characterize and compare risk profiles for BE using a nationally representative inpatient database.
Methods: We conducted a retrospective analysis using the National Inpatient Sample (NIS) from 2018 to 2022. Adult hospitalizations with a diagnosis of BE were identified and stratified into young-onset (≤50 years) and typical-onset ( >50 years). Multivariable logistic regression analyses were performed separately within each age group to evaluate independent associations between demographic and clinical factors and BE, adjusted for sex, race, income quartile, insurance status, comorbidity burden, and hospital characteristics. Analyses accounted for NIS survey design and weighting.
Results: A total of 618,090 weighted hospitalizations for BE were identified; 58,075 (9.4%) occurred in the young-onset group, and 560,015 (90.6%) in the typical-onset group. While GERD was a strong predictor of BE in both groups, the association was markedly stronger in young adults (aOR 12.75 [95% CI 12.16–13.38]) compared to older adults (aOR 4.35 [95% CI 4.28–4.41]). Hiatal hernia emerged as the single strongest predictor of BE across age groups but demonstrated notably greater odds in young adults (aOR 29.71 [95% CI 28.19–31.31]) compared to older adults (aOR 8.74 [95% CI 8.58–8.90]). Additionally, obstructive sleep apnea (OSA) (aOR 2.74 vs 1.49), scleroderma (aOR 7.27 vs 4.73), eosinophilic esophagitis (aOR 6.45 vs 4.68), alcohol use disorder (aOR 2.82 vs 1.66), and hypertension (aOR 2.95 vs 1.17), were significantly more associated with BE in younger adults.
Discussion: Young-onset BE is characterized by distinct and significantly stronger associations with GERD, hiatal hernia, OSA, eosinophilic esophagitis, alcohol use, and cardiometabolic conditions compared to typical-onset BE. These results show the importance of recognizing younger adults as a unique population with a specific risk profile, necessitating targeted screening and tailored management strategies.
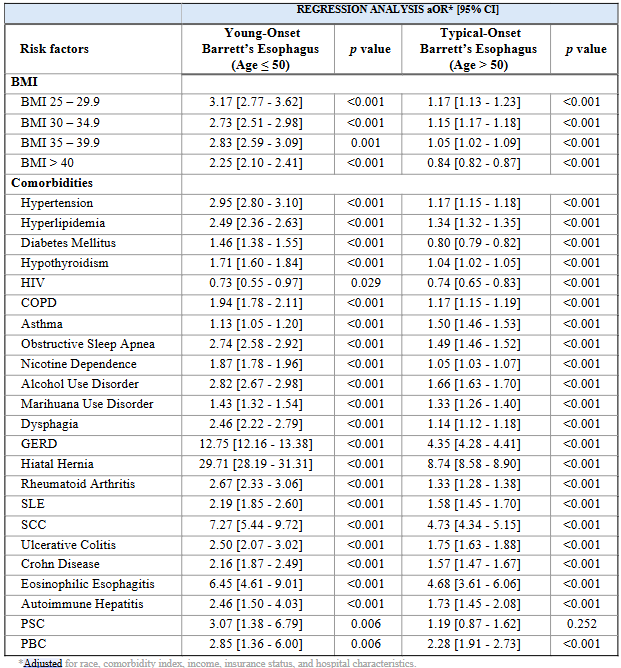
Figure: Table 1. Distinct Risk Profiles for Young-Onset Versus Typical-Onset Barrett’s Esophagus: Multivariable Regression Analysis
Disclosures:
Daniel Gonzalez Mosquera indicated no relevant financial relationships.
Maria Belen Mateo indicated no relevant financial relationships.
Carolina Gonzalez Mosquera indicated no relevant financial relationships.
Juan Martinez-Ortega indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Carla Evangelista indicated no relevant financial relationships.
Daniel Alejandro. Gonzalez Mosquera, MD1, Maria Belen Mateo, MD2, Carolina Gonzalez Mosquera, MD3, Juan Martinez-Ortega, MD4, Yassine Kilani, MD5, Carla Evangelista, MD4. P2770 - Distinct Clinical Risk of Barrett’s Esophagus in Younger vs Older Adults: A Nationwide Inpatient Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1NYC Health + Hospitals/Lincoln, Bronx, NY; 2Knowledge and Research Evaluation Unit, Mayo Clinic, Rochester, Minnesota, USA, Rochester, MN; 3Universidad Católica Santiago de Guayaquil, Guayaquil, Guayas, Ecuador; 4New York Health + Hospitals | Lincoln–Weill Cornell Medical College Affiliate, New York, USA, Bronx, NY; 5Saint Louis University School of Medicine, Saint Louis, MO
Introduction: Barrett’s Esophagus (BE) has been considered a condition primarily affecting older adults, with an estimated prevalence of 5.6% among U.S. adults. It is most commonly linked to longstanding gastroesophageal reflux disease (GERD). However, recent evidence suggests a rising prevalence in younger individuals, with rates of approximately 0.06% among those aged 0–29 years and 1.6% among those aged 30–44 years. While GERD remains a central risk factor, younger patients may present with a distinct constellation of associated conditions. We aimed to characterize and compare risk profiles for BE using a nationally representative inpatient database.
Methods: We conducted a retrospective analysis using the National Inpatient Sample (NIS) from 2018 to 2022. Adult hospitalizations with a diagnosis of BE were identified and stratified into young-onset (≤50 years) and typical-onset ( >50 years). Multivariable logistic regression analyses were performed separately within each age group to evaluate independent associations between demographic and clinical factors and BE, adjusted for sex, race, income quartile, insurance status, comorbidity burden, and hospital characteristics. Analyses accounted for NIS survey design and weighting.
Results: A total of 618,090 weighted hospitalizations for BE were identified; 58,075 (9.4%) occurred in the young-onset group, and 560,015 (90.6%) in the typical-onset group. While GERD was a strong predictor of BE in both groups, the association was markedly stronger in young adults (aOR 12.75 [95% CI 12.16–13.38]) compared to older adults (aOR 4.35 [95% CI 4.28–4.41]). Hiatal hernia emerged as the single strongest predictor of BE across age groups but demonstrated notably greater odds in young adults (aOR 29.71 [95% CI 28.19–31.31]) compared to older adults (aOR 8.74 [95% CI 8.58–8.90]). Additionally, obstructive sleep apnea (OSA) (aOR 2.74 vs 1.49), scleroderma (aOR 7.27 vs 4.73), eosinophilic esophagitis (aOR 6.45 vs 4.68), alcohol use disorder (aOR 2.82 vs 1.66), and hypertension (aOR 2.95 vs 1.17), were significantly more associated with BE in younger adults.
Discussion: Young-onset BE is characterized by distinct and significantly stronger associations with GERD, hiatal hernia, OSA, eosinophilic esophagitis, alcohol use, and cardiometabolic conditions compared to typical-onset BE. These results show the importance of recognizing younger adults as a unique population with a specific risk profile, necessitating targeted screening and tailored management strategies.
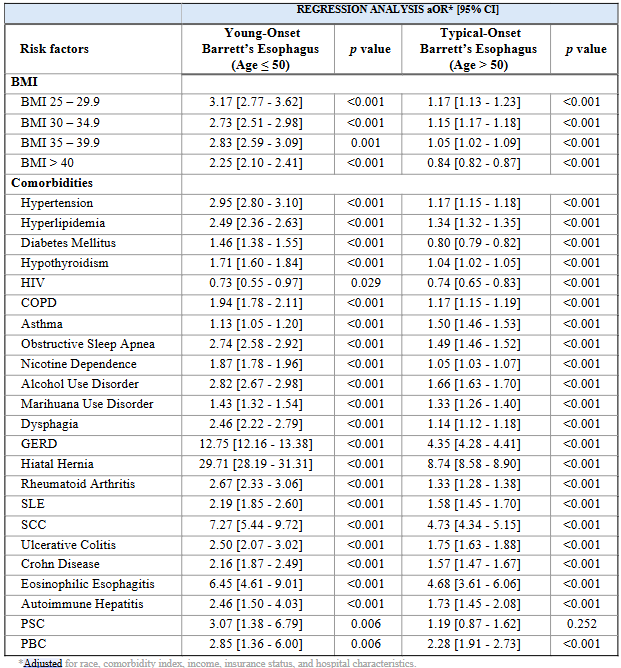
Figure: Table 1. Distinct Risk Profiles for Young-Onset Versus Typical-Onset Barrett’s Esophagus: Multivariable Regression Analysis
Disclosures:
Daniel Gonzalez Mosquera indicated no relevant financial relationships.
Maria Belen Mateo indicated no relevant financial relationships.
Carolina Gonzalez Mosquera indicated no relevant financial relationships.
Juan Martinez-Ortega indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Carla Evangelista indicated no relevant financial relationships.
Daniel Alejandro. Gonzalez Mosquera, MD1, Maria Belen Mateo, MD2, Carolina Gonzalez Mosquera, MD3, Juan Martinez-Ortega, MD4, Yassine Kilani, MD5, Carla Evangelista, MD4. P2770 - Distinct Clinical Risk of Barrett’s Esophagus in Younger vs Older Adults: A Nationwide Inpatient Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
