Monday Poster Session
Category: Esophagus
P2756 - E-POEM Outcomes in Patients With Spastic Esophageal Disorders: A Single Center Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ross M. Dies, MD, MS
Louisiana State University Health
New Orleans, LA
Presenting Author(s)
Ross M. Dies, MD, MS1, Farhan Mohiuddin, MD2, Natalie Roppolo, MD3, Megan Maloz, BS2, Sofia Novacic, BS3, William Haynes, BS3, Michelle Neice, MD4, Michael Tran, MD5, Omar Khan, MD5, Qiang Cai, MD, PhD, MACG6
1Louisiana State University Health, New Orleans, LA; 2Louisiana State University School of Medicine, New Orleans, LA; 3Louisiana State University School of Medicine, Shreveport, LA; 4Louisiana State University Health, Shreveport, LA; 5LSU Health Shreveport, Shreveport, LA; 6LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA
Introduction: Esophageal per-oral endoscopic myotomy (POEM) has arisen as an acceptable minimally invasive approach for the treatment of achalasia. It has been shown to be comparable to Heller myotomy (HM) in relation to safety, efficacy, and complications; outcomes are strong even in patients failing prior HM. In addition, POEM is increasingly being considered as a promising treatment for spastic esophageal disorders (SED). Although long-term data are limited, early studies suggest it may benefit patients unresponsive to prior therapies. This study explores the clinical success of POEM in these patients at our institution, including follow-up to 31 months.
Methods: We reviewed all patients with SED treated with POEM from October 2021 to October 2023 at our institution. Each patient suffered from dysphagia, chest pain, or both. The diagnosis of distal esophageal spasm or hypercontractile esophagus was confirmed by esophagogastroduodenoscopy and high-resolution manometry. Pre-procedure and follow-up Eckardt scores were documented. Fisher’s exact test was used to compare differences in outcomes for myotomy length less than and greater than 10 cm.
Results: 13 patients were reviewed, 62% of whom were female. The average age of patients was 62 years. POEM was successfully performed in all 13 patients; one patient underwent POEM twice for recurrence of symptoms. The follow-up time ranged from 2 weeks to 31 months. The average Eckardt score before POEM was 5; the average score at follow-up was 1.07. 11 patients experienced symptom resolution at follow-up, with one patient experiencing minimal resolution of symptoms until POEM was repeated 5 months after the initial procedure, leading to resolution of symptoms at that time. The average procedure time was 26.1 minutes.
Discussion: Our study demonstrates the effectiveness of POEM in patients with SED refractory to medical therapy. Clinical success for esophageal disorders using the Eckardt score is generally defined as post-intervention Eckardt scores < 3. While myotomy length has been discussed as a possible variable affecting outcomes, a systematic review did not find a difference in clinical success rate in studies where total myotomy length was greater than 10 cm versus studies with myotomy length less than 10 cm. Indeed, our study also demonstrated no measurable difference in POEM with myotomy length less than or greater than 10 cm. These results highlight the clinical utility of POEM for SED, but additional research is needed to corroborate these findings.
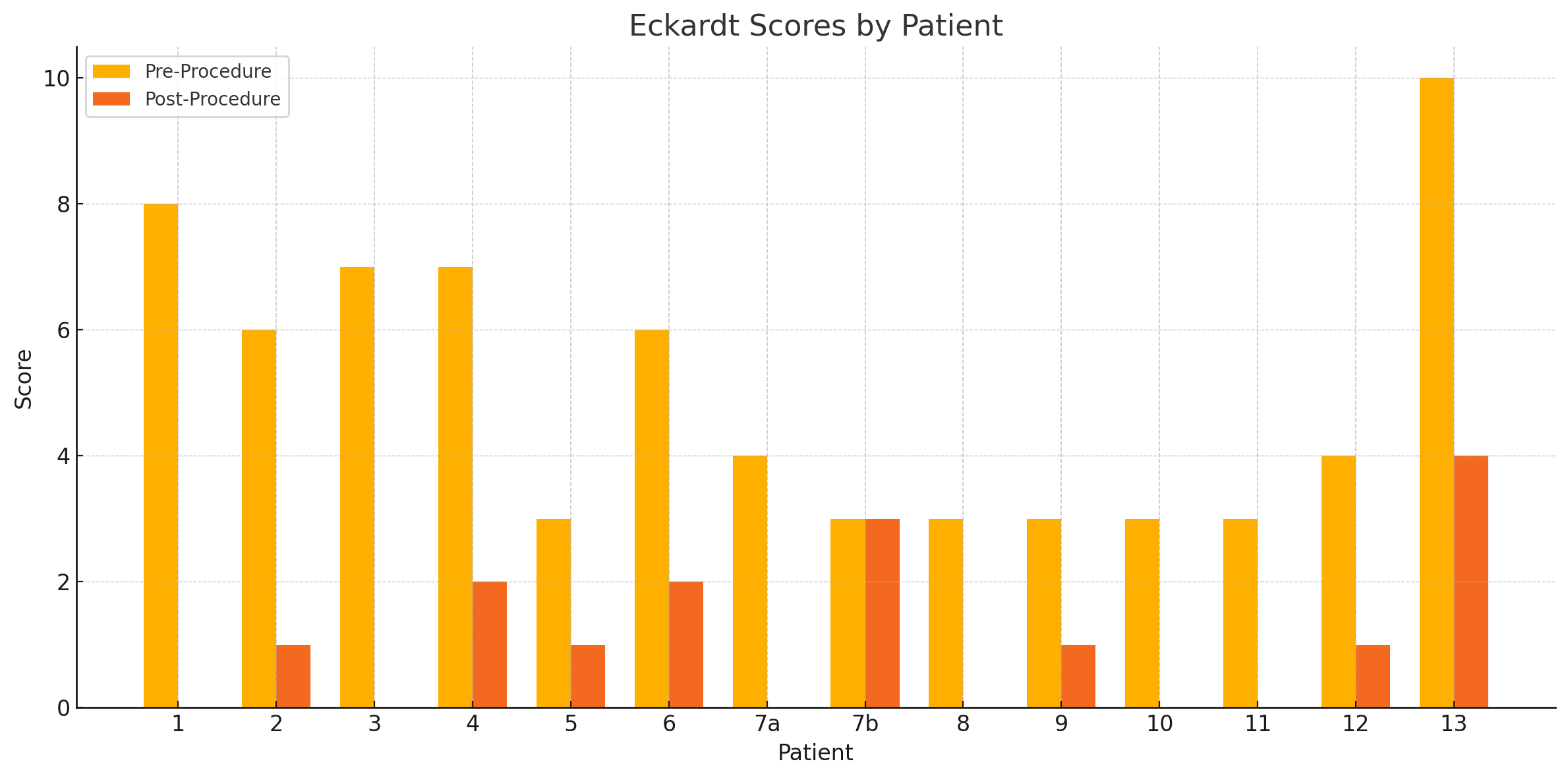
Figure: Eckardt scores by patient, both prior to and after POEM; patient 7 had a repeat POEM to address recurrence of symptoms
Disclosures:
Ross Dies indicated no relevant financial relationships.
Farhan Mohiuddin indicated no relevant financial relationships.
Natalie Roppolo indicated no relevant financial relationships.
Megan Maloz indicated no relevant financial relationships.
Sofia Novacic indicated no relevant financial relationships.
William Haynes indicated no relevant financial relationships.
Michelle Neice indicated no relevant financial relationships.
Michael Tran indicated no relevant financial relationships.
Omar Khan indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Ross M. Dies, MD, MS1, Farhan Mohiuddin, MD2, Natalie Roppolo, MD3, Megan Maloz, BS2, Sofia Novacic, BS3, William Haynes, BS3, Michelle Neice, MD4, Michael Tran, MD5, Omar Khan, MD5, Qiang Cai, MD, PhD, MACG6. P2756 - E-POEM Outcomes in Patients With Spastic Esophageal Disorders: A Single Center Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Louisiana State University Health, New Orleans, LA; 2Louisiana State University School of Medicine, New Orleans, LA; 3Louisiana State University School of Medicine, Shreveport, LA; 4Louisiana State University Health, Shreveport, LA; 5LSU Health Shreveport, Shreveport, LA; 6LSU Health Sciences Center - SHREVEPORT, LA, Shreveport, LA
Introduction: Esophageal per-oral endoscopic myotomy (POEM) has arisen as an acceptable minimally invasive approach for the treatment of achalasia. It has been shown to be comparable to Heller myotomy (HM) in relation to safety, efficacy, and complications; outcomes are strong even in patients failing prior HM. In addition, POEM is increasingly being considered as a promising treatment for spastic esophageal disorders (SED). Although long-term data are limited, early studies suggest it may benefit patients unresponsive to prior therapies. This study explores the clinical success of POEM in these patients at our institution, including follow-up to 31 months.
Methods: We reviewed all patients with SED treated with POEM from October 2021 to October 2023 at our institution. Each patient suffered from dysphagia, chest pain, or both. The diagnosis of distal esophageal spasm or hypercontractile esophagus was confirmed by esophagogastroduodenoscopy and high-resolution manometry. Pre-procedure and follow-up Eckardt scores were documented. Fisher’s exact test was used to compare differences in outcomes for myotomy length less than and greater than 10 cm.
Results: 13 patients were reviewed, 62% of whom were female. The average age of patients was 62 years. POEM was successfully performed in all 13 patients; one patient underwent POEM twice for recurrence of symptoms. The follow-up time ranged from 2 weeks to 31 months. The average Eckardt score before POEM was 5; the average score at follow-up was 1.07. 11 patients experienced symptom resolution at follow-up, with one patient experiencing minimal resolution of symptoms until POEM was repeated 5 months after the initial procedure, leading to resolution of symptoms at that time. The average procedure time was 26.1 minutes.
Discussion: Our study demonstrates the effectiveness of POEM in patients with SED refractory to medical therapy. Clinical success for esophageal disorders using the Eckardt score is generally defined as post-intervention Eckardt scores < 3. While myotomy length has been discussed as a possible variable affecting outcomes, a systematic review did not find a difference in clinical success rate in studies where total myotomy length was greater than 10 cm versus studies with myotomy length less than 10 cm. Indeed, our study also demonstrated no measurable difference in POEM with myotomy length less than or greater than 10 cm. These results highlight the clinical utility of POEM for SED, but additional research is needed to corroborate these findings.
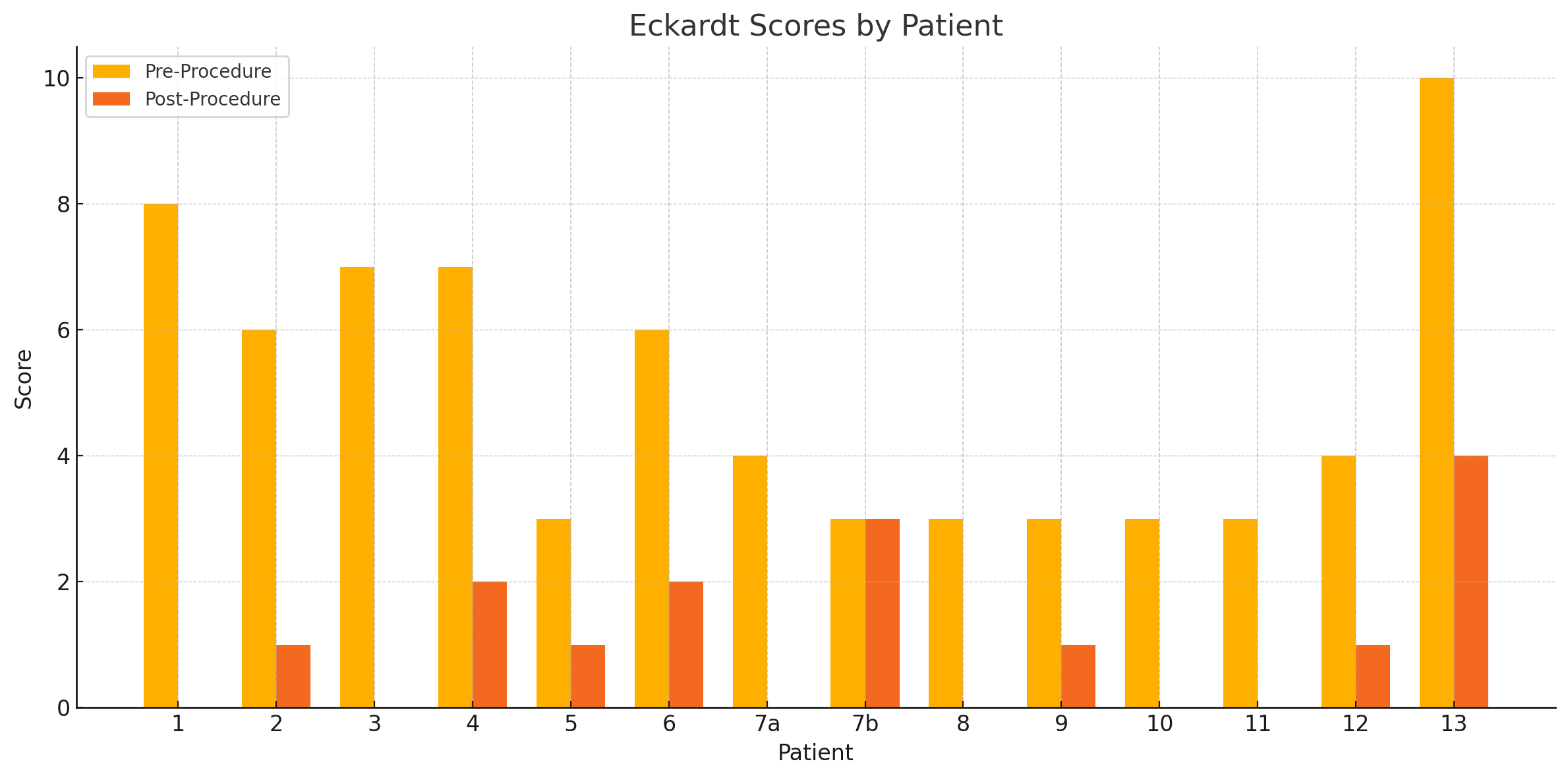
Figure: Eckardt scores by patient, both prior to and after POEM; patient 7 had a repeat POEM to address recurrence of symptoms
Disclosures:
Ross Dies indicated no relevant financial relationships.
Farhan Mohiuddin indicated no relevant financial relationships.
Natalie Roppolo indicated no relevant financial relationships.
Megan Maloz indicated no relevant financial relationships.
Sofia Novacic indicated no relevant financial relationships.
William Haynes indicated no relevant financial relationships.
Michelle Neice indicated no relevant financial relationships.
Michael Tran indicated no relevant financial relationships.
Omar Khan indicated no relevant financial relationships.
Qiang Cai indicated no relevant financial relationships.
Ross M. Dies, MD, MS1, Farhan Mohiuddin, MD2, Natalie Roppolo, MD3, Megan Maloz, BS2, Sofia Novacic, BS3, William Haynes, BS3, Michelle Neice, MD4, Michael Tran, MD5, Omar Khan, MD5, Qiang Cai, MD, PhD, MACG6. P2756 - E-POEM Outcomes in Patients With Spastic Esophageal Disorders: A Single Center Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
