Monday Poster Session
Category: Diet, Nutrition, and Obesity
P2683 - The Obesity Paradox: Nationwide Analysis Using the National Inpatient Sample
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vignesh Krishnan Nagesh, MBBS
Hackensack Meridian Health - Palisades Medical Center
Rochester, MN
Presenting Author(s)
Vignesh Krishnan Nagesh, MBBS1, Vivek Joseph Varughese, MBBS2, Gomathy Nageswaran, MBBS3, Emelyn Martinez, MD4, Marina Basta, MBBS4, Adam Atoot, MD4
1Hackensack Meridian Health - Palisades Medical Center, North Bergen, NJ; 2Prisma Health, University of South Carolina School of Medicine, Columbia, SC; 3University of Arkansas for Medical Sciences, Little Rock, AR; 4Hackensack Meridian Palisades Medical Center, North Bergen, NJ
Introduction: Obesity is a well-established risk factor for numerous chronic conditions, including cardiovascular disease, respiratory illness, and metabolic disorders. However, the "obesity paradox" suggests that obese individuals may experience lower in-hospital mortality rates despite their higher burden of comorbidities. This study evaluates the impact of comorbid obesity on in-hospital outcomes for patients admitted with congestive heart failure (CHF), acute myocardial infarction (AMI), chronic obstructive pulmonary disease (COPD), sepsis, and cirrhosis.
Methods: Using data from the National Inpatient Sample (NIS), we conducted a retrospective analysis of inpatient outcomes, including all-cause mortality, length of hospital stay, and total hospital charges. Multivariate logistic regression analyses were performed to assess the association between obesity and in-hospital survival, accounting for potential confounders such as age, sex, race, and socioeconomic status.
Results: Obesity was associated with significantly lower in-hospital mortality for CHF (OR: 1.26, 95% CI: 1.17-1.36,p-0.), AMI (OR: 1.19, 95% CI: 1.10-1.29), COPD (OR: 1.57, 95% CI: 1.29-1.92), and sepsis (OR: 1.48, 95% CI: 1.43-1.54), but not for cirrhosis (OR: 1.13, 95% CI: 0.92-1.39). However, obesity was associated with increased hospital length of stay and higher hospitalization costs across all conditions.
Discussion: This nationwide study confirms the obesity paradox, showing lower in-hospital mortality among obese patients with CHF, AMI, COPD, and sepsis, but not in those with liver cirrhosis. Proposed mechanisms include greater metabolic reserve and anti-inflammatory effects, though outcomes vary by disease. Despite survival benefits, obesity was linked to longer hospital stays and higher costs. The paradox remains poorly understood and highlights the need for further prospective studies to guide care for obese patients with chronic illnesses.
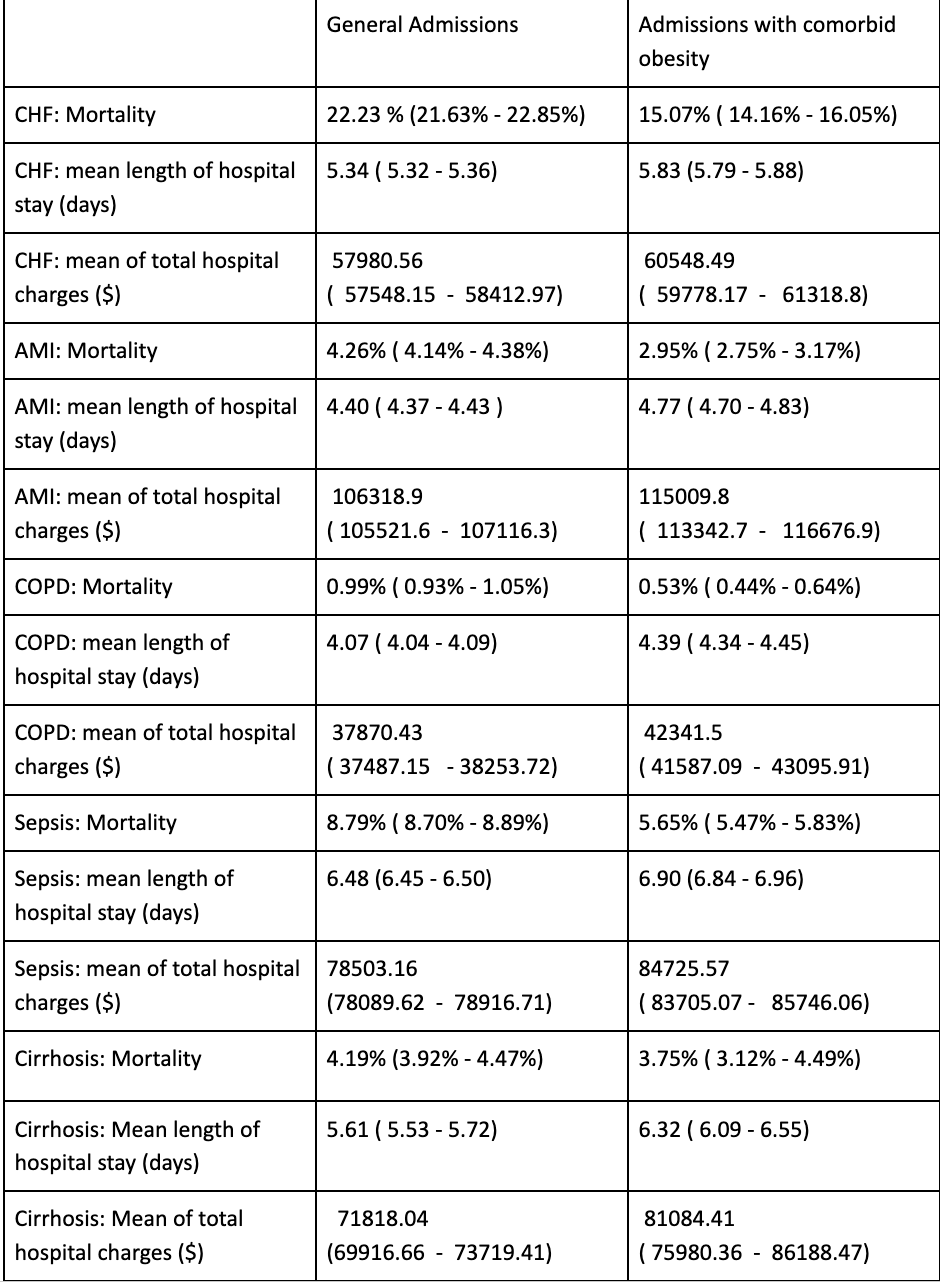
Figure: COMPARISON OF MORTALITY AND IN HOSPITAL OUTCOMES
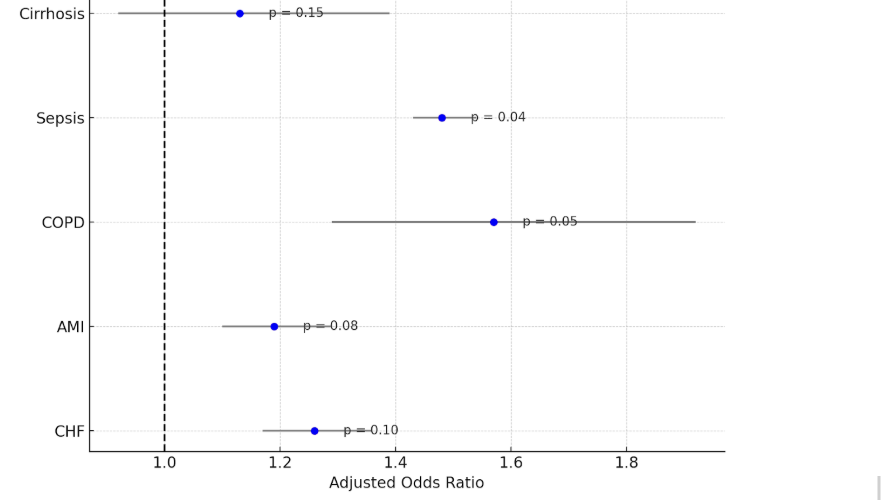
Figure: ASSOCIATION BETWEEN SURVIVAL AND OBESITY IN ADMISSIONS FOR CHRONIC CONDITIONS
Disclosures:
Vignesh Krishnan Nagesh indicated no relevant financial relationships.
Vivek Joseph Varughese indicated no relevant financial relationships.
Gomathy Nageswaran indicated no relevant financial relationships.
Emelyn Martinez indicated no relevant financial relationships.
Marina Basta indicated no relevant financial relationships.
Adam Atoot indicated no relevant financial relationships.
Vignesh Krishnan Nagesh, MBBS1, Vivek Joseph Varughese, MBBS2, Gomathy Nageswaran, MBBS3, Emelyn Martinez, MD4, Marina Basta, MBBS4, Adam Atoot, MD4. P2683 - The Obesity Paradox: Nationwide Analysis Using the National Inpatient Sample, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hackensack Meridian Health - Palisades Medical Center, North Bergen, NJ; 2Prisma Health, University of South Carolina School of Medicine, Columbia, SC; 3University of Arkansas for Medical Sciences, Little Rock, AR; 4Hackensack Meridian Palisades Medical Center, North Bergen, NJ
Introduction: Obesity is a well-established risk factor for numerous chronic conditions, including cardiovascular disease, respiratory illness, and metabolic disorders. However, the "obesity paradox" suggests that obese individuals may experience lower in-hospital mortality rates despite their higher burden of comorbidities. This study evaluates the impact of comorbid obesity on in-hospital outcomes for patients admitted with congestive heart failure (CHF), acute myocardial infarction (AMI), chronic obstructive pulmonary disease (COPD), sepsis, and cirrhosis.
Methods: Using data from the National Inpatient Sample (NIS), we conducted a retrospective analysis of inpatient outcomes, including all-cause mortality, length of hospital stay, and total hospital charges. Multivariate logistic regression analyses were performed to assess the association between obesity and in-hospital survival, accounting for potential confounders such as age, sex, race, and socioeconomic status.
Results: Obesity was associated with significantly lower in-hospital mortality for CHF (OR: 1.26, 95% CI: 1.17-1.36,p-0.), AMI (OR: 1.19, 95% CI: 1.10-1.29), COPD (OR: 1.57, 95% CI: 1.29-1.92), and sepsis (OR: 1.48, 95% CI: 1.43-1.54), but not for cirrhosis (OR: 1.13, 95% CI: 0.92-1.39). However, obesity was associated with increased hospital length of stay and higher hospitalization costs across all conditions.
Discussion: This nationwide study confirms the obesity paradox, showing lower in-hospital mortality among obese patients with CHF, AMI, COPD, and sepsis, but not in those with liver cirrhosis. Proposed mechanisms include greater metabolic reserve and anti-inflammatory effects, though outcomes vary by disease. Despite survival benefits, obesity was linked to longer hospital stays and higher costs. The paradox remains poorly understood and highlights the need for further prospective studies to guide care for obese patients with chronic illnesses.
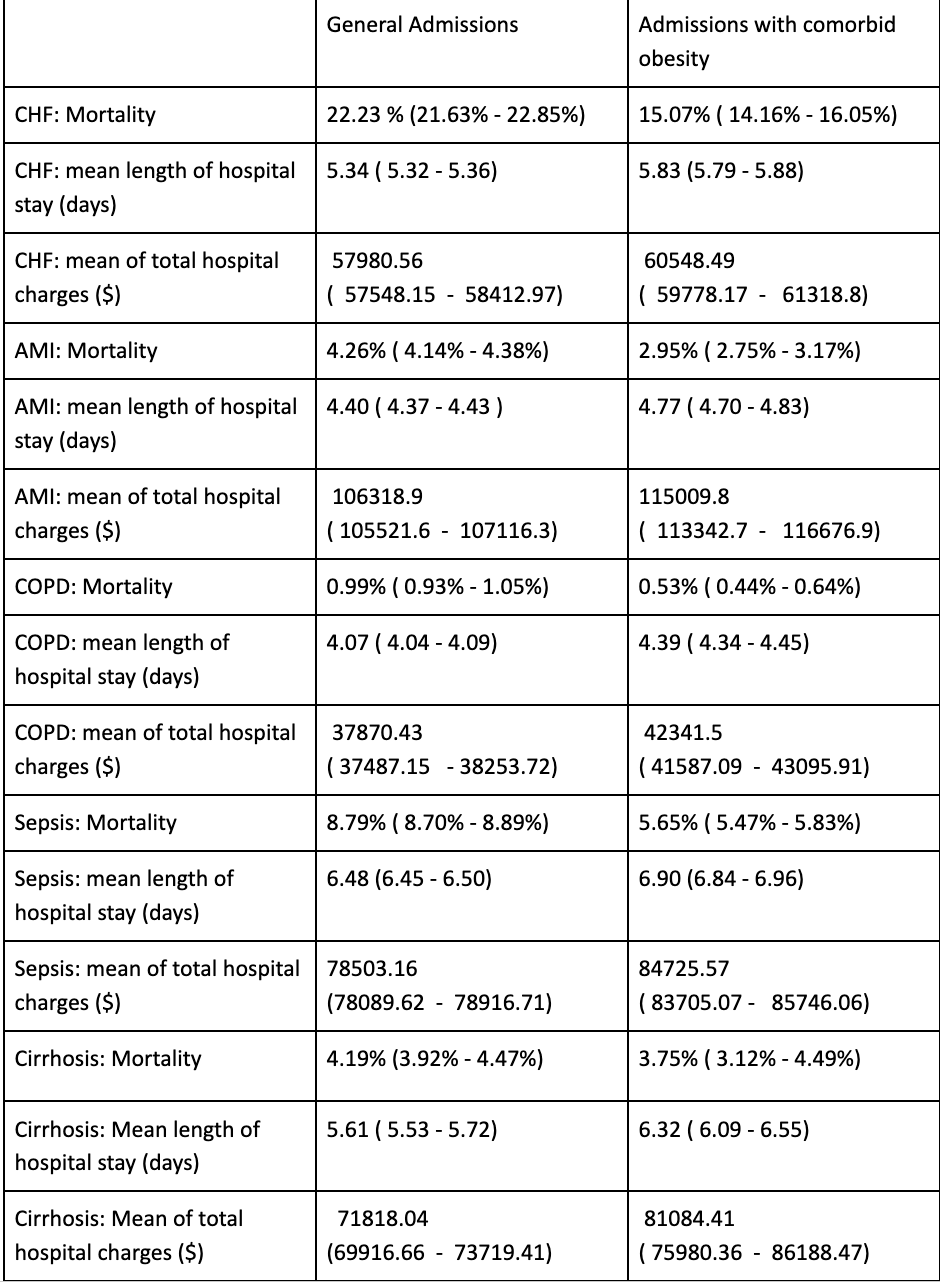
Figure: COMPARISON OF MORTALITY AND IN HOSPITAL OUTCOMES
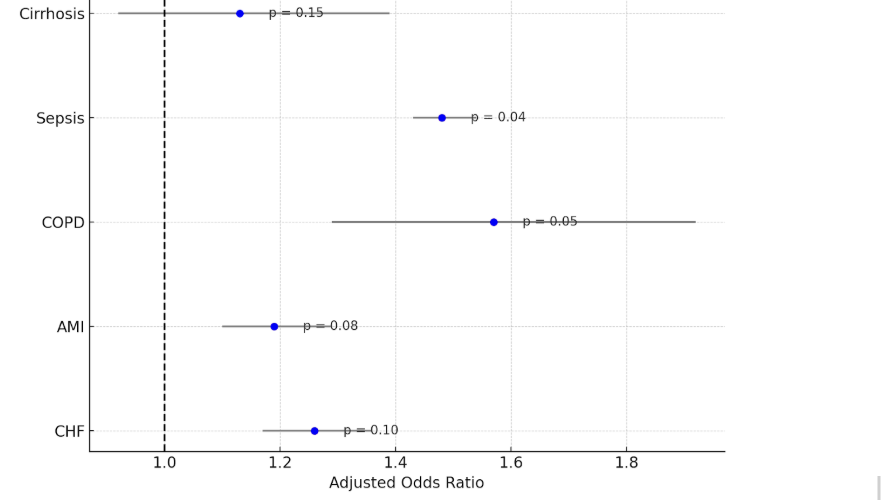
Figure: ASSOCIATION BETWEEN SURVIVAL AND OBESITY IN ADMISSIONS FOR CHRONIC CONDITIONS
Disclosures:
Vignesh Krishnan Nagesh indicated no relevant financial relationships.
Vivek Joseph Varughese indicated no relevant financial relationships.
Gomathy Nageswaran indicated no relevant financial relationships.
Emelyn Martinez indicated no relevant financial relationships.
Marina Basta indicated no relevant financial relationships.
Adam Atoot indicated no relevant financial relationships.
Vignesh Krishnan Nagesh, MBBS1, Vivek Joseph Varughese, MBBS2, Gomathy Nageswaran, MBBS3, Emelyn Martinez, MD4, Marina Basta, MBBS4, Adam Atoot, MD4. P2683 - The Obesity Paradox: Nationwide Analysis Using the National Inpatient Sample, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
