Monday Poster Session
Category: Colorectal Cancer Prevention
P2640 - Long-Term Outcomes Following Resection of Large and Complex Colorectal Polyps
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- NB
Nathan Billett, MD
Kaiser Permanente
San Francisco, CA
Presenting Author(s)
Nathan Billett, MD, Shiyun Zhu, BS, Vincent Zhang, BS, Kevin Su, BS, Sabrina Zhong, BS, Jeffrey Lee, MD
Kaiser Permanente, San Francisco, CA
Introduction: Current guidelines recommend a follow-up colonoscopy six months after endoscopic resection of large non-pedunculated colorectal polyps (LNPCPs). However, recent research suggests that the risk of residual or recurrent adenoma (RRA) is low for selected LNPCPs, with no significant difference in RRA rates between 6- and 12-month surveillance intervals. In this study, we examined whether RRA rates differed between early and late surveillance periods following endoscopic resection of LNPCPs in the Kaiser Permanente Northern California (KPNC) population.
Methods: This retrospective cohort study included KPNC patients who underwent endoscopic mucosal resection (EMR) of LNPCPs ≥20 mm between January 1, 2010, and December 31, 2022, and had a follow-up colonoscopy within 24 months. The primary outcomes were the rates of RRA, defined as any adenoma found at the prior EMR site, and synchronous advanced neoplasia, defined as adenocarcinoma, conventional adenoma with high-grade dysplasia, villous or tubulovillous histology, or any conventional adenoma >10 mm found outside the EMR site. RRA and synchronous advanced neoplasia rates were calculated overall, by LNPCP histology, and by timing of follow-up colonoscopy: early (3–10 months) and late (11–24 months).
Results: A total of 442 LNPCPs underwent EMR, with an overall RRA rate of 16.7%. Of these, 294 had follow-up colonoscopy during the early surveillance period and 148 during the late period. The RRA rates for early and late surveillance were 17.7% and 14.9%, respectively, with no significant difference between them. However, when stratified by LNPCP histology, RRA rates differed significantly: high-grade dysplasia (24.1%), villous or tubulovillous adenoma (22.7%), sessile serrated adenoma (14.5%), and other conventional adenomas (12.2%). The overall rate of synchronous advanced neoplasia was 7.2%, with no significant variation by surveillance period or histology type.
Discussion: There was no statistically significant difference in RRA rates of LNPCPs between early and late surveillance periods. Advanced histology was linked to higher RRA risk, with high-grade dysplasia posing the greatest risk and conventional adenomas the least. A key limitation was the 35.5% rate of EMR sites lacking biopsy, relying solely on visual inspection, which may have underestimated true RRA rates. Low-risk conventional adenomas may justify extending the first surveillance colonoscopy beyond six months.
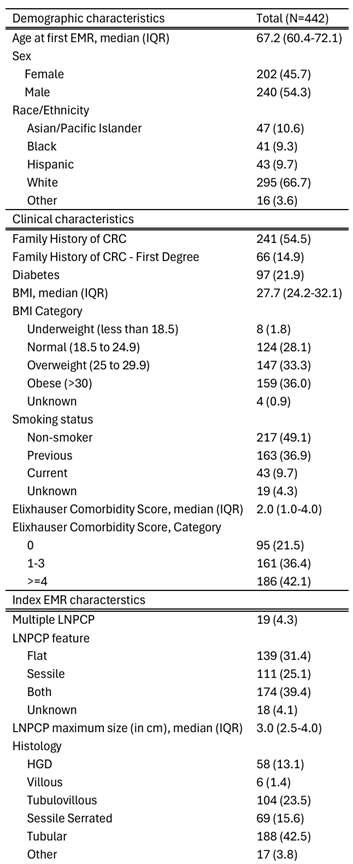
Figure: Table 1. Patient demographic and clinical characteristics. HGD = high-grade dysplasia.
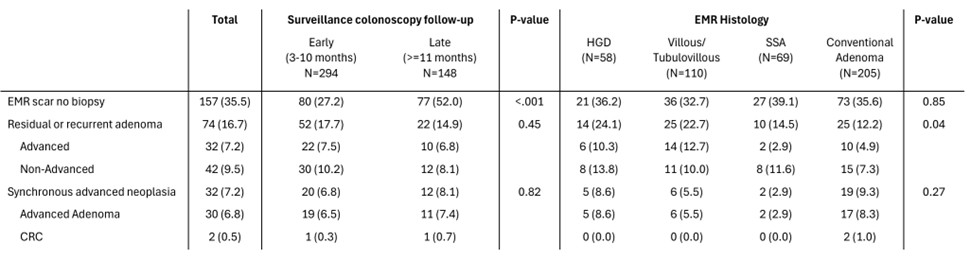
Figure: Table 2. Outcomes at first surveillance colonoscopy follow-up. HGD = high-grade dysplasia. SSA = sessile serrated adenoma. CRC = colorectal cancer.
Disclosures:
Nathan Billett indicated no relevant financial relationships.
Shiyun Zhu indicated no relevant financial relationships.
Vincent Zhang indicated no relevant financial relationships.
Kevin Su indicated no relevant financial relationships.
Sabrina Zhong indicated no relevant financial relationships.
Jeffrey Lee indicated no relevant financial relationships.
Nathan Billett, MD, Shiyun Zhu, BS, Vincent Zhang, BS, Kevin Su, BS, Sabrina Zhong, BS, Jeffrey Lee, MD. P2640 - Long-Term Outcomes Following Resection of Large and Complex Colorectal Polyps, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Kaiser Permanente, San Francisco, CA
Introduction: Current guidelines recommend a follow-up colonoscopy six months after endoscopic resection of large non-pedunculated colorectal polyps (LNPCPs). However, recent research suggests that the risk of residual or recurrent adenoma (RRA) is low for selected LNPCPs, with no significant difference in RRA rates between 6- and 12-month surveillance intervals. In this study, we examined whether RRA rates differed between early and late surveillance periods following endoscopic resection of LNPCPs in the Kaiser Permanente Northern California (KPNC) population.
Methods: This retrospective cohort study included KPNC patients who underwent endoscopic mucosal resection (EMR) of LNPCPs ≥20 mm between January 1, 2010, and December 31, 2022, and had a follow-up colonoscopy within 24 months. The primary outcomes were the rates of RRA, defined as any adenoma found at the prior EMR site, and synchronous advanced neoplasia, defined as adenocarcinoma, conventional adenoma with high-grade dysplasia, villous or tubulovillous histology, or any conventional adenoma >10 mm found outside the EMR site. RRA and synchronous advanced neoplasia rates were calculated overall, by LNPCP histology, and by timing of follow-up colonoscopy: early (3–10 months) and late (11–24 months).
Results: A total of 442 LNPCPs underwent EMR, with an overall RRA rate of 16.7%. Of these, 294 had follow-up colonoscopy during the early surveillance period and 148 during the late period. The RRA rates for early and late surveillance were 17.7% and 14.9%, respectively, with no significant difference between them. However, when stratified by LNPCP histology, RRA rates differed significantly: high-grade dysplasia (24.1%), villous or tubulovillous adenoma (22.7%), sessile serrated adenoma (14.5%), and other conventional adenomas (12.2%). The overall rate of synchronous advanced neoplasia was 7.2%, with no significant variation by surveillance period or histology type.
Discussion: There was no statistically significant difference in RRA rates of LNPCPs between early and late surveillance periods. Advanced histology was linked to higher RRA risk, with high-grade dysplasia posing the greatest risk and conventional adenomas the least. A key limitation was the 35.5% rate of EMR sites lacking biopsy, relying solely on visual inspection, which may have underestimated true RRA rates. Low-risk conventional adenomas may justify extending the first surveillance colonoscopy beyond six months.
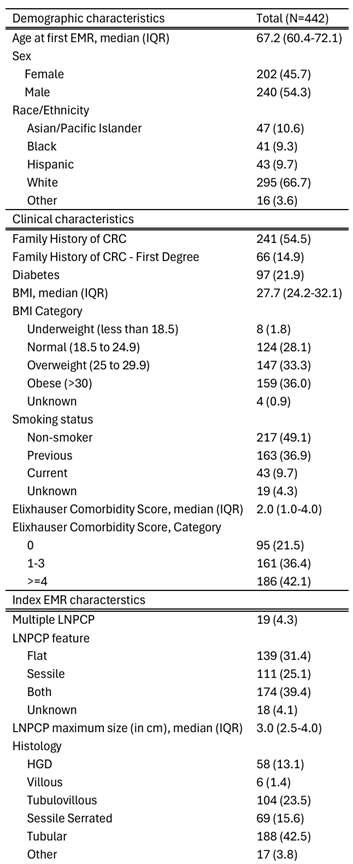
Figure: Table 1. Patient demographic and clinical characteristics. HGD = high-grade dysplasia.
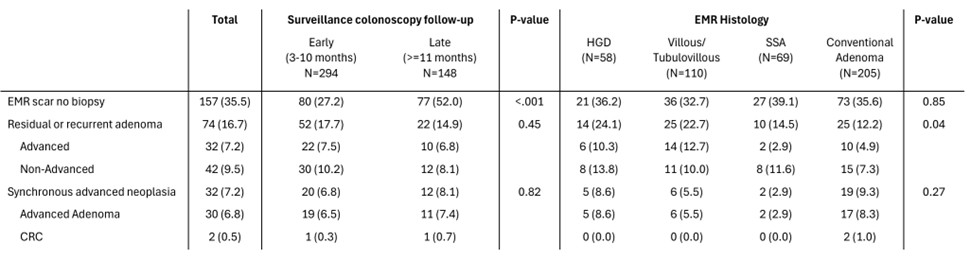
Figure: Table 2. Outcomes at first surveillance colonoscopy follow-up. HGD = high-grade dysplasia. SSA = sessile serrated adenoma. CRC = colorectal cancer.
Disclosures:
Nathan Billett indicated no relevant financial relationships.
Shiyun Zhu indicated no relevant financial relationships.
Vincent Zhang indicated no relevant financial relationships.
Kevin Su indicated no relevant financial relationships.
Sabrina Zhong indicated no relevant financial relationships.
Jeffrey Lee indicated no relevant financial relationships.
Nathan Billett, MD, Shiyun Zhu, BS, Vincent Zhang, BS, Kevin Su, BS, Sabrina Zhong, BS, Jeffrey Lee, MD. P2640 - Long-Term Outcomes Following Resection of Large and Complex Colorectal Polyps, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
