Monday Poster Session
Category: Colon
P2585 - A Bizarre Bridge: Colosalpingeal Fistula as a Complication of Sigmoid Diverticulitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Diego J. Duran Baez, MD (he/him/his)
Mount Sinai South Nassau,Icahn School of Medicine at Mount Sinai
Uniondale, NY
Presenting Author(s)
Diego J. Duran Baez, MD1, Lenura Ziyadin, DO2, Jonathan Vincent M Reyes, MD2, Lakhana Muhddesa, DO2, Kasim Kazbay, MD2, Frank G. Gress, MD, MBA2, Keith Brennan, MD3
1Mount Sinai South Nassau,Icahn School of Medicine at Mount Sinai, Uniondale, NY; 2Mount Sinai South Nassau,Icahn School of Medicine at Mount Sinai, Oceanside, NY; 3Mount Sinai South Nassau, Oceanside, NY
Introduction: Fistula formation is a known complication of acute diverticulitis and can form throughout multiple adjacent organs or structures with an initial incidence of 2-4%, rising to 20% in those with prior history of surgical treatment for diverticular disease. Colosalpingeal fistulas, forming between the intestine and fallopian tubes, are a very rare with few recorded cases. Here we present a case of a postmenopausal woman who presented with diverticular disease progressing to formation of a left colosapingeal fistula.
Case Description/
Methods: A 60-year-old postmenopausal female with prior medical history of Hodgkin’s lymphoma with remission and ectopic pregnancy status-post dilatation and curettage who presented to our institution with sudden-onset abdominal pain. The patient arrived tachycardic and physical exam was remarkable for diffuse tenderness to palpation. WBC on arrival was 21,400/μL. CT of the abdomen and pelvis showed marked sigmoid wall thickening consistent with diverticulitis (Figure 1A). Intravenous antibiotics (Zosyn) were started. Persistent fevers and no significant improvement in the initial leukocytosis were noted in the first days of hospitalization. A repeat CT was performed and showed an anterior contained sigmoid perforation (Figure 1B). The patient remained clinically stable and did not require surgical intervention at the time. Another repeat CT scan was performed as a method of monitoring the perforation and development of a left colosalpingeal fistula was seen (Figure 1C). MRI of the pelvis was then performed to confirm findings (Figure 2). The patient’s recurrent fevers resolved by the fifth day of admission, and it was determined that patient would require long term antibiotics. A peripheral central line was placed. The patient was discharged on a 6-week course of Invanz and then underwent colonoscopy which showed no significant findings. Sigmoidectomy with concurrent bilateral salpingoophorectomy (BSO) was performed later as part of definitive management.
Discussion: Colosalpingeal fistulas are difficult to diagnose as symptoms can be nonspecific. CT scans are the gold standard for diagnosis, and management will depend on the patient’s desire to maintain fertility. Definitive management in postmenopausal women is sigmoid resection with BSO. This case highlights the importance of multispecialty management in rare complications of diverticulitis.
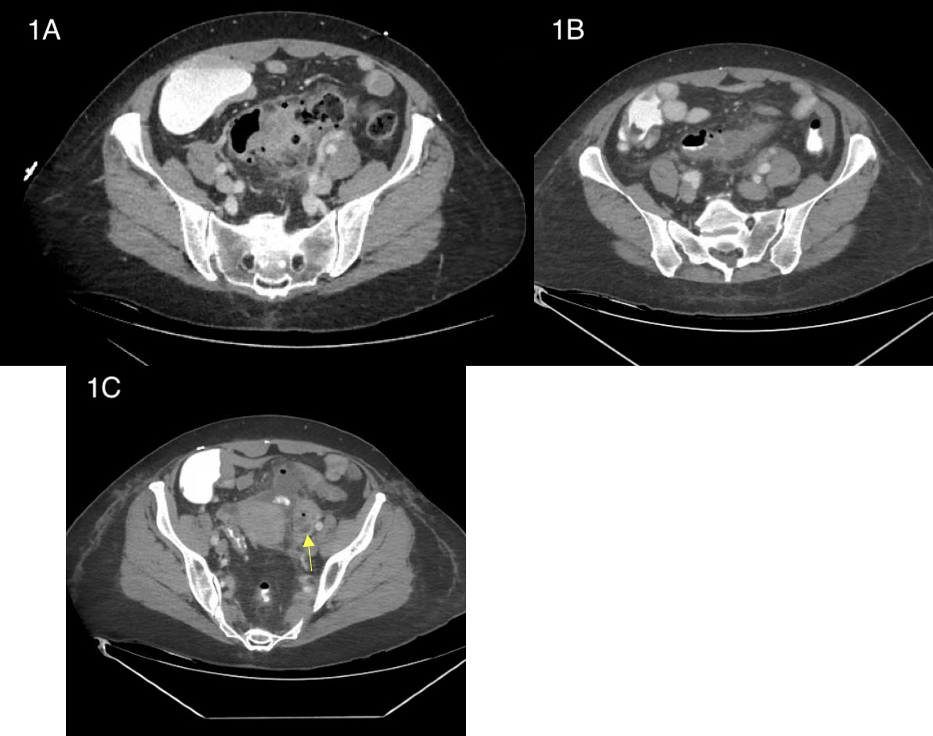
Figure: Figure 1: CT of the abdomen and pelvis on admission showing sigmoid wall thickening (A).
Second CT abdomen and pelvis presenting contained perforation within sigmoid wall (B).
Third CT abdomen and pelvis showing new left colosalpingeal fistula (yellow arrow) (C).
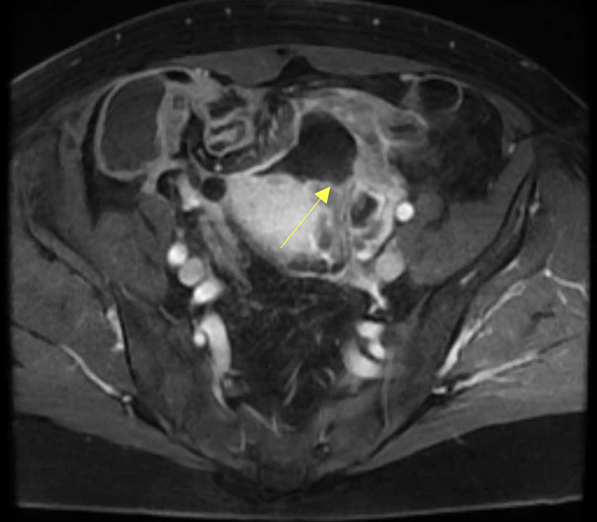
Figure: Figure 2: MRI of the pelvis showing a fluid collection in the sigmoid colon communicating with the left fallopian tube (yellow arrow)
Disclosures:
Diego J. Duran Baez indicated no relevant financial relationships.
Lenura Ziyadin indicated no relevant financial relationships.
Jonathan Vincent M Reyes indicated no relevant financial relationships.
Lakhana Muhddesa indicated no relevant financial relationships.
Kasim Kazbay indicated no relevant financial relationships.
Frank Gress indicated no relevant financial relationships.
Keith Brennan indicated no relevant financial relationships.
Diego J. Duran Baez, MD1, Lenura Ziyadin, DO2, Jonathan Vincent M Reyes, MD2, Lakhana Muhddesa, DO2, Kasim Kazbay, MD2, Frank G. Gress, MD, MBA2, Keith Brennan, MD3. P2585 - A Bizarre Bridge: Colosalpingeal Fistula as a Complication of Sigmoid Diverticulitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai South Nassau,Icahn School of Medicine at Mount Sinai, Uniondale, NY; 2Mount Sinai South Nassau,Icahn School of Medicine at Mount Sinai, Oceanside, NY; 3Mount Sinai South Nassau, Oceanside, NY
Introduction: Fistula formation is a known complication of acute diverticulitis and can form throughout multiple adjacent organs or structures with an initial incidence of 2-4%, rising to 20% in those with prior history of surgical treatment for diverticular disease. Colosalpingeal fistulas, forming between the intestine and fallopian tubes, are a very rare with few recorded cases. Here we present a case of a postmenopausal woman who presented with diverticular disease progressing to formation of a left colosapingeal fistula.
Case Description/
Methods: A 60-year-old postmenopausal female with prior medical history of Hodgkin’s lymphoma with remission and ectopic pregnancy status-post dilatation and curettage who presented to our institution with sudden-onset abdominal pain. The patient arrived tachycardic and physical exam was remarkable for diffuse tenderness to palpation. WBC on arrival was 21,400/μL. CT of the abdomen and pelvis showed marked sigmoid wall thickening consistent with diverticulitis (Figure 1A). Intravenous antibiotics (Zosyn) were started. Persistent fevers and no significant improvement in the initial leukocytosis were noted in the first days of hospitalization. A repeat CT was performed and showed an anterior contained sigmoid perforation (Figure 1B). The patient remained clinically stable and did not require surgical intervention at the time. Another repeat CT scan was performed as a method of monitoring the perforation and development of a left colosalpingeal fistula was seen (Figure 1C). MRI of the pelvis was then performed to confirm findings (Figure 2). The patient’s recurrent fevers resolved by the fifth day of admission, and it was determined that patient would require long term antibiotics. A peripheral central line was placed. The patient was discharged on a 6-week course of Invanz and then underwent colonoscopy which showed no significant findings. Sigmoidectomy with concurrent bilateral salpingoophorectomy (BSO) was performed later as part of definitive management.
Discussion: Colosalpingeal fistulas are difficult to diagnose as symptoms can be nonspecific. CT scans are the gold standard for diagnosis, and management will depend on the patient’s desire to maintain fertility. Definitive management in postmenopausal women is sigmoid resection with BSO. This case highlights the importance of multispecialty management in rare complications of diverticulitis.
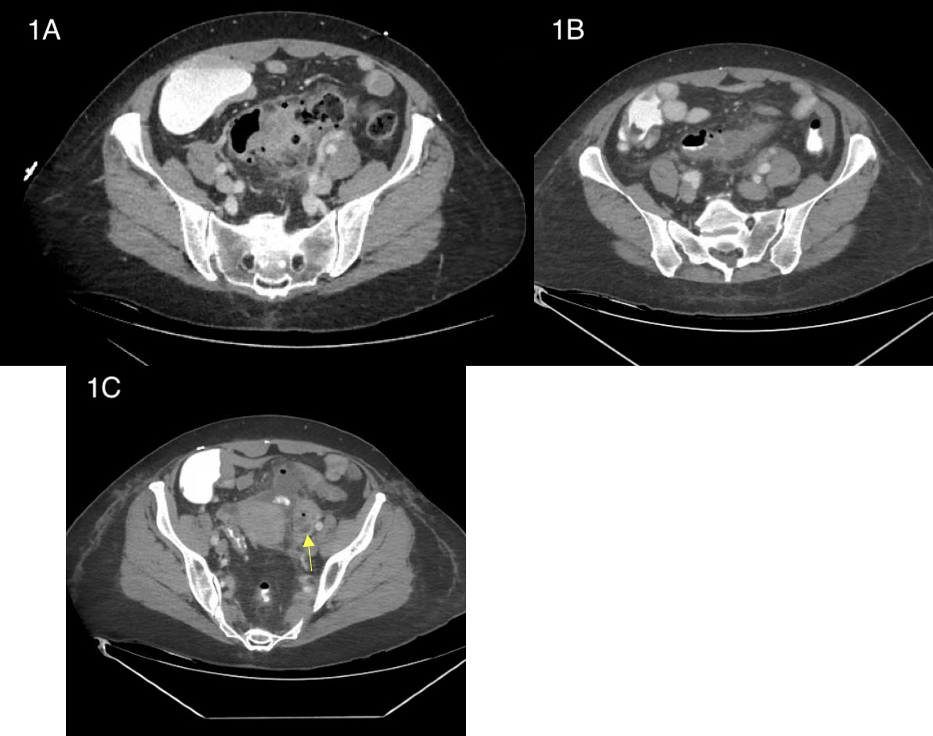
Figure: Figure 1: CT of the abdomen and pelvis on admission showing sigmoid wall thickening (A).
Second CT abdomen and pelvis presenting contained perforation within sigmoid wall (B).
Third CT abdomen and pelvis showing new left colosalpingeal fistula (yellow arrow) (C).
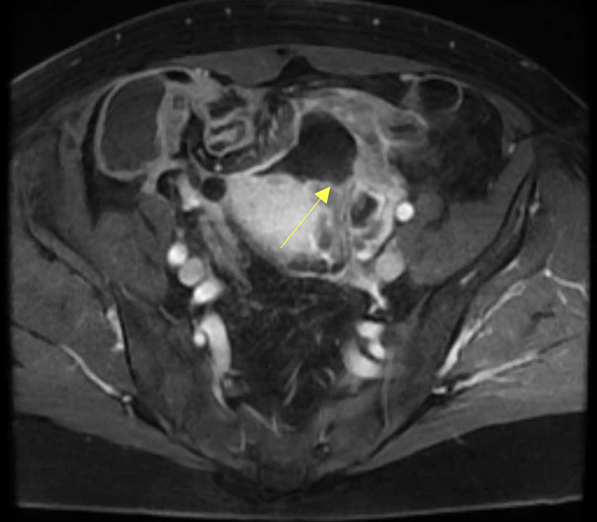
Figure: Figure 2: MRI of the pelvis showing a fluid collection in the sigmoid colon communicating with the left fallopian tube (yellow arrow)
Disclosures:
Diego J. Duran Baez indicated no relevant financial relationships.
Lenura Ziyadin indicated no relevant financial relationships.
Jonathan Vincent M Reyes indicated no relevant financial relationships.
Lakhana Muhddesa indicated no relevant financial relationships.
Kasim Kazbay indicated no relevant financial relationships.
Frank Gress indicated no relevant financial relationships.
Keith Brennan indicated no relevant financial relationships.
Diego J. Duran Baez, MD1, Lenura Ziyadin, DO2, Jonathan Vincent M Reyes, MD2, Lakhana Muhddesa, DO2, Kasim Kazbay, MD2, Frank G. Gress, MD, MBA2, Keith Brennan, MD3. P2585 - A Bizarre Bridge: Colosalpingeal Fistula as a Complication of Sigmoid Diverticulitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
