Monday Poster Session
Category: Colon
P2581 - When Ischemic Colitis Resembles Malignancy: A Case Report of Diagnostic and Therapeutic Challenges
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Neil Chokshi, DO
Mount Sinai Medical Center
Miami Beach, FL
Presenting Author(s)
Samuel Ramos Garcia, MD1, Neil Chokshi, DO2, Jignesh Parikh, MD3, Saad Khan, MD4, Vania Zayat, MD5
1University of Central Florida, HCA Healthcare GME, Kissimmee, FL; 2Mount Sinai Medical Center, Miami Beach, FL; 3Orlando VA Medical Center and UCF/HCA Greater Orlando, Kissimmee, FL; 4Orlando VA Healthcare System, Orlando, FL; 5University of Central Florida College of Medicine, Orlando, FL
Introduction: Ischemic colitis (IC) occurs due to reduced blood flow to the colon, leading to inflammation and mucosal injury. It commonly affects older adults with comorbidities such as cardiovascular disease, diabetes, and hypertension. IC typically presents with abdominal pain, hematochezia, and diarrhea, but in rare cases, it can mimic malignancy.
Case Description/
Methods: A 73-year-old male with multiple cardiovascular comorbidities presented with epigastric and midsternal pain. Laboratory results showed anemia (Hgb 7.2 g/dL), and further workup revealed iron deficiency. After receiving two packed red blood cell transfusions, he was discharged with iron supplementation. Eight months later, an esophagogastroduodenoscopy (EGD) and colonoscopy revealed a non-obstructing, ulcerated cecal mass suspected to be malignant (see figure 1). However, pathology confirmed ischemic colitis with no malignant characteristics (see figure 2). A PET scan showed no malignancy, and the patient was managed conservatively. Three months later, he presented with recurrent abdominal pain, weight loss, and nausea, leading to additional workup including repeat colonoscopy, which unexpectedly showed normal colonic mucosa with spontaneous resolution of the cecal mass. Further imaging confirmed mesenteric ischemia with complications of gastrointestinal bleeding and transfusion dependence.
Discussion: This case highlights the diagnostic and therapeutic challenges of ischemic colitis, especially in patients with multiple comorbidities. Mass-forming ischemic colitis can mimic malignancy, making accurate diagnosis essential through multimodal imaging, endoscopic evaluation, and histopathology. The patient’s complex presentation, with ischemic colitis, gastritis, gastric ulcers, and arteriovenous malformations, demonstrates how various gastrointestinal conditions can overlap and complicate management. The case stresses the importance of a comprehensive approach, including timely diagnostics and appropriate interventions, to ensure effective management in high-risk patients. Early recognition and careful follow-up are crucial to preventing delays in treatment and avoiding complications such as anemia, gastrointestinal bleeding, and mesenteric ischemia.
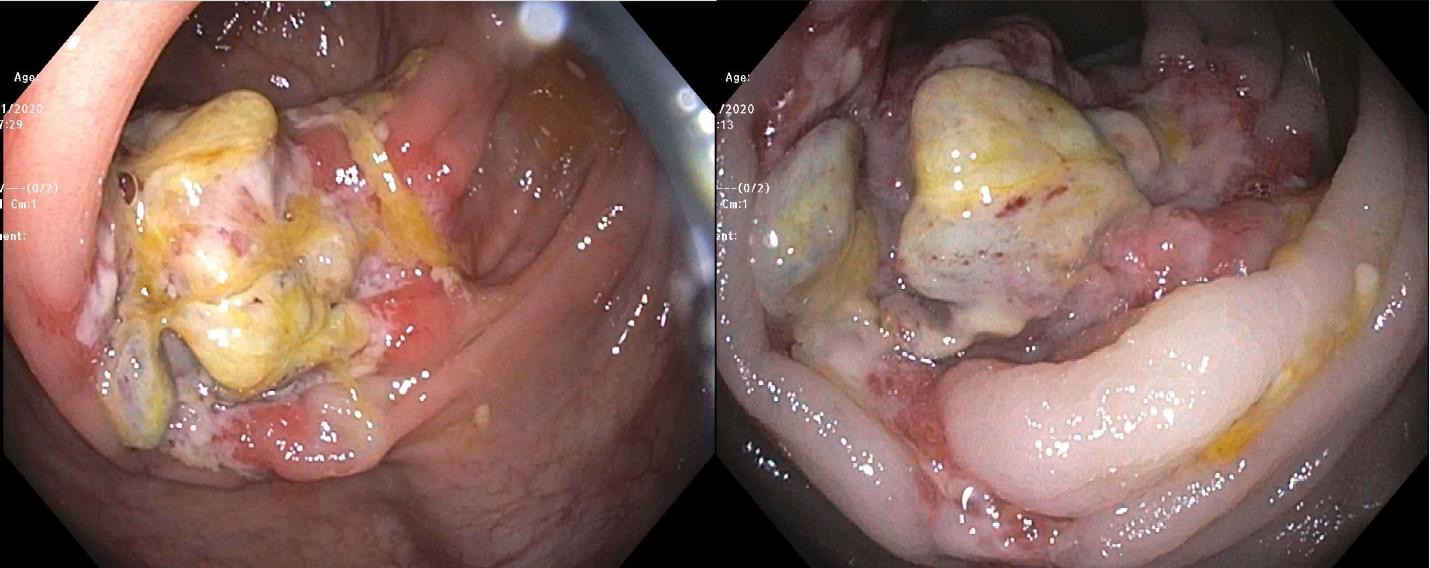
Figure: Figure 1 Endoscopic finding of a large non-obstructive ulcerated mass in the cecum, resembling a malignant tumor
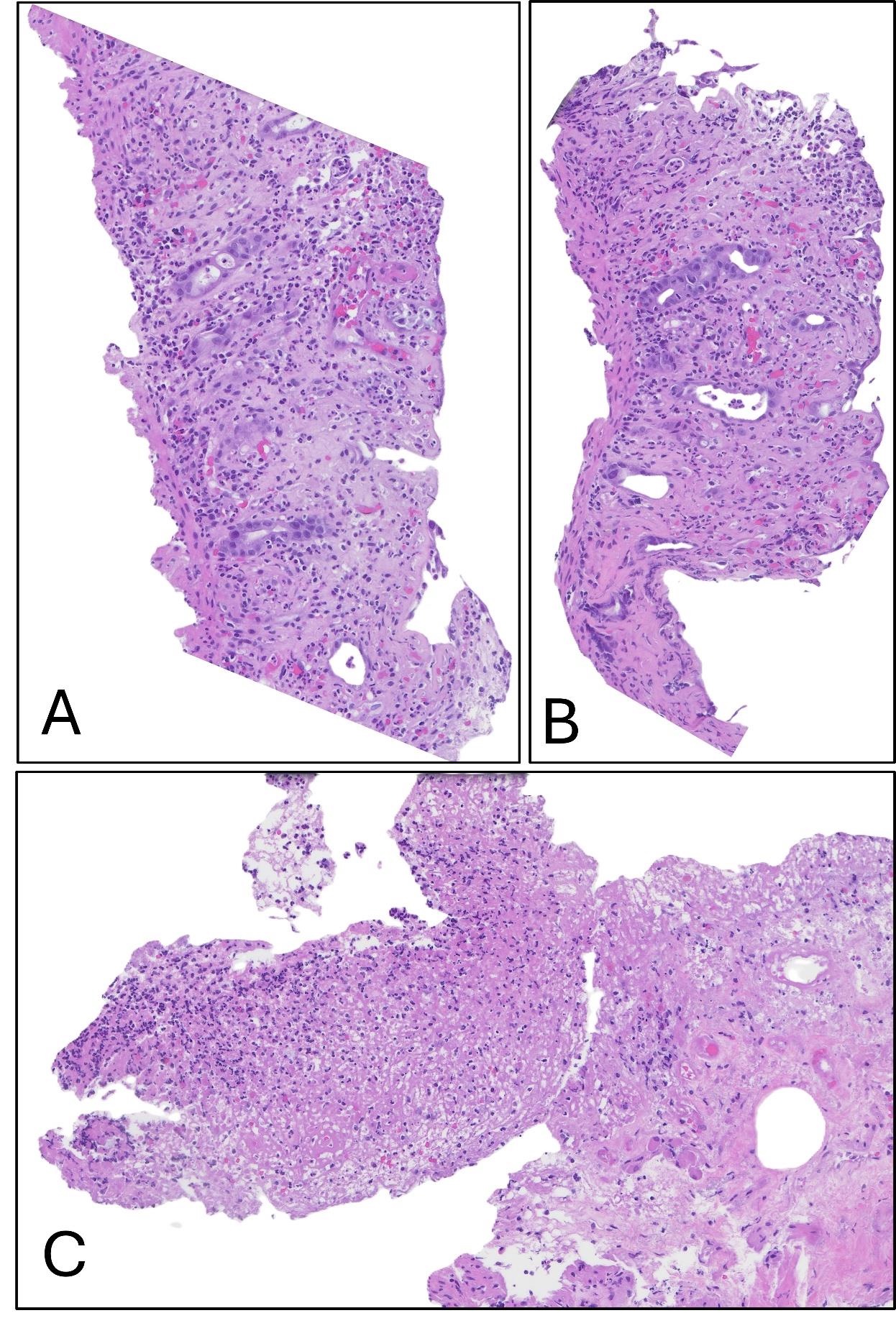
Figure: Figure 2 H&E stained sections show hyalinization of stroma, crypt withering and thinning of mucosa (Panel A and B, 20x). Focal area shows features suggestive of pseudomembrane (Panel C, 20x). No evidence of dysplasia or malignancy.
Disclosures:
Samuel Ramos Garcia indicated no relevant financial relationships.
Neil Chokshi indicated no relevant financial relationships.
Jignesh Parikh indicated no relevant financial relationships.
Saad Khan indicated no relevant financial relationships.
Vania Zayat indicated no relevant financial relationships.
Samuel Ramos Garcia, MD1, Neil Chokshi, DO2, Jignesh Parikh, MD3, Saad Khan, MD4, Vania Zayat, MD5. P2581 - When Ischemic Colitis Resembles Malignancy: A Case Report of Diagnostic and Therapeutic Challenges, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Kissimmee, FL; 2Mount Sinai Medical Center, Miami Beach, FL; 3Orlando VA Medical Center and UCF/HCA Greater Orlando, Kissimmee, FL; 4Orlando VA Healthcare System, Orlando, FL; 5University of Central Florida College of Medicine, Orlando, FL
Introduction: Ischemic colitis (IC) occurs due to reduced blood flow to the colon, leading to inflammation and mucosal injury. It commonly affects older adults with comorbidities such as cardiovascular disease, diabetes, and hypertension. IC typically presents with abdominal pain, hematochezia, and diarrhea, but in rare cases, it can mimic malignancy.
Case Description/
Methods: A 73-year-old male with multiple cardiovascular comorbidities presented with epigastric and midsternal pain. Laboratory results showed anemia (Hgb 7.2 g/dL), and further workup revealed iron deficiency. After receiving two packed red blood cell transfusions, he was discharged with iron supplementation. Eight months later, an esophagogastroduodenoscopy (EGD) and colonoscopy revealed a non-obstructing, ulcerated cecal mass suspected to be malignant (see figure 1). However, pathology confirmed ischemic colitis with no malignant characteristics (see figure 2). A PET scan showed no malignancy, and the patient was managed conservatively. Three months later, he presented with recurrent abdominal pain, weight loss, and nausea, leading to additional workup including repeat colonoscopy, which unexpectedly showed normal colonic mucosa with spontaneous resolution of the cecal mass. Further imaging confirmed mesenteric ischemia with complications of gastrointestinal bleeding and transfusion dependence.
Discussion: This case highlights the diagnostic and therapeutic challenges of ischemic colitis, especially in patients with multiple comorbidities. Mass-forming ischemic colitis can mimic malignancy, making accurate diagnosis essential through multimodal imaging, endoscopic evaluation, and histopathology. The patient’s complex presentation, with ischemic colitis, gastritis, gastric ulcers, and arteriovenous malformations, demonstrates how various gastrointestinal conditions can overlap and complicate management. The case stresses the importance of a comprehensive approach, including timely diagnostics and appropriate interventions, to ensure effective management in high-risk patients. Early recognition and careful follow-up are crucial to preventing delays in treatment and avoiding complications such as anemia, gastrointestinal bleeding, and mesenteric ischemia.
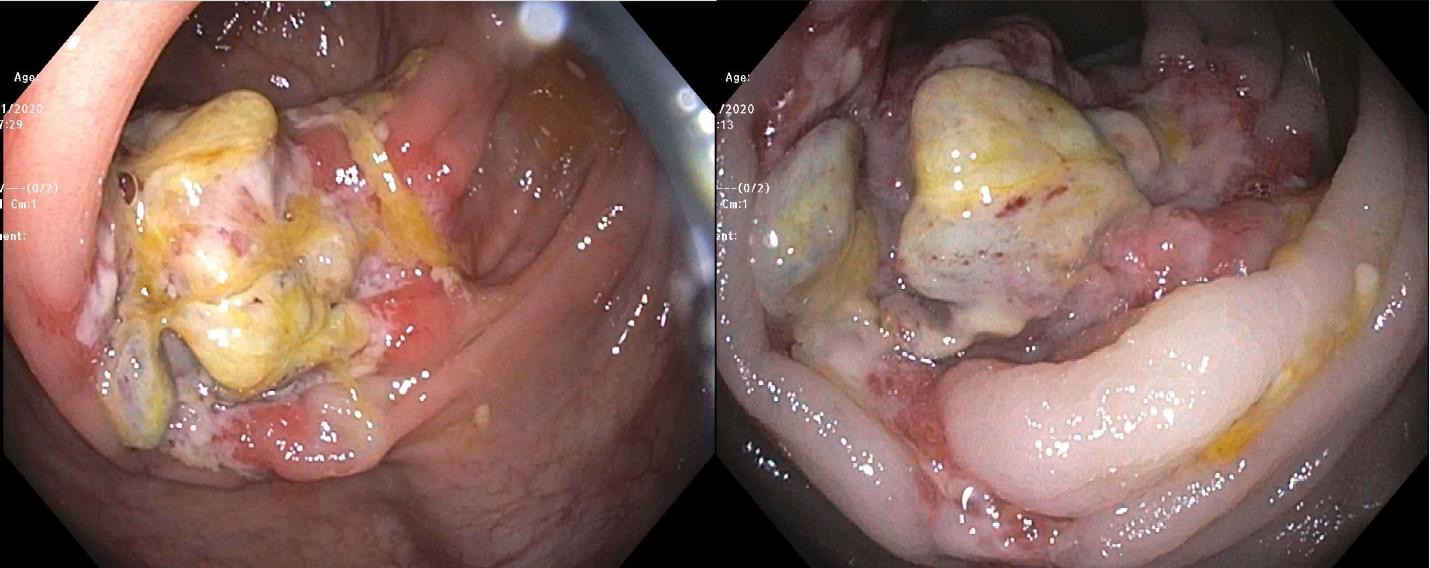
Figure: Figure 1 Endoscopic finding of a large non-obstructive ulcerated mass in the cecum, resembling a malignant tumor
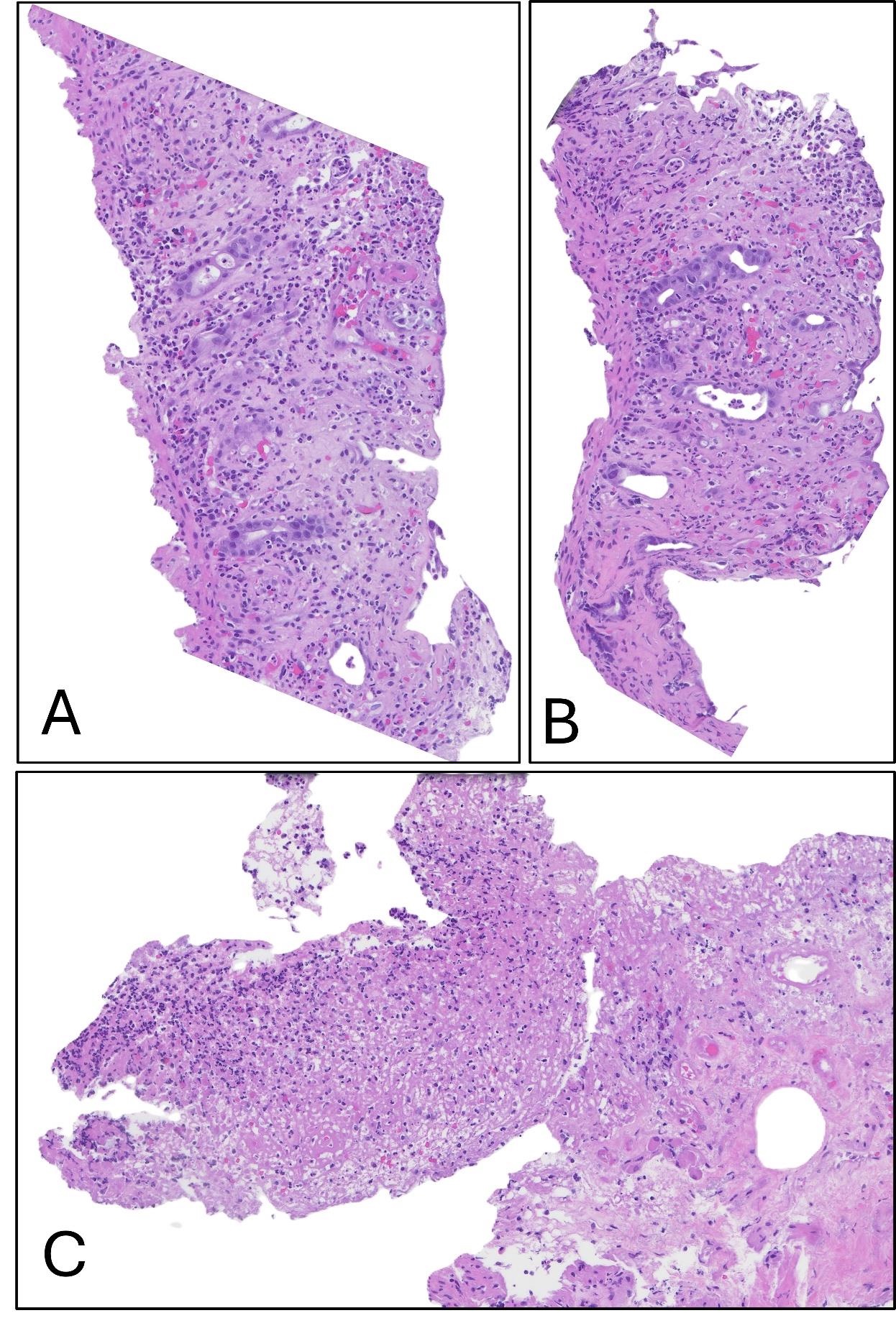
Figure: Figure 2 H&E stained sections show hyalinization of stroma, crypt withering and thinning of mucosa (Panel A and B, 20x). Focal area shows features suggestive of pseudomembrane (Panel C, 20x). No evidence of dysplasia or malignancy.
Disclosures:
Samuel Ramos Garcia indicated no relevant financial relationships.
Neil Chokshi indicated no relevant financial relationships.
Jignesh Parikh indicated no relevant financial relationships.
Saad Khan indicated no relevant financial relationships.
Vania Zayat indicated no relevant financial relationships.
Samuel Ramos Garcia, MD1, Neil Chokshi, DO2, Jignesh Parikh, MD3, Saad Khan, MD4, Vania Zayat, MD5. P2581 - When Ischemic Colitis Resembles Malignancy: A Case Report of Diagnostic and Therapeutic Challenges, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
