Monday Poster Session
Category: Colon
P2519 - Cut It Out! Surgical Resection for a Case of Refractory Segmental Colitis Associated With Diverticulosis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Arvin N. Tan, MD
University of Hawaii, John A. Burns School of Medicine, Department of Medicine
Honolulu, HI
Presenting Author(s)
Arvin Jeremy N. Tan, MD1, Akiko Tokunaga, MD2, Toru Nakata, MD, PhD1, Yusuke Miyatani, MD1, Vishal Dobaria, MD1, Traci T. Murakami, MD, FACG3
1University of Hawaii, John A. Burns School of Medicine, Department of Medicine, Honolulu, HI; 2University of Hawaii, John A. Burns School of Medicine, Department of Pathology, Honolulu, HI; 3The Queen's Medical Center, Ewa Beach, HI
Introduction: Segmental Colitis Associated with Diverticulosis (SCAD) is a rare clinical entity characterized by non-specific, segmental thickening of the colonic wall with diverticulosis. The prevalence of SCAD is estimated at 2% to 11% in patients with diverticular disease. Here, we present a case of a patient with SCAD that was refractory to medical therapy and underwent sigmoidectomy.
Case Description/
Methods: A 49-year-old Hispanic and Native American male with a history of hypertension presented to the clinic with a one-month history of progressive hematochezia. This was accompanied by the sensation of incomplete emptying of the rectum and rectal pain. Otherwise, he denied abdominal pain, nausea, vomiting, unintended weight loss, and changes in appetite. During this time, his stools were softer than usual, but he did not have diarrhea. He underwent colonoscopy, which showed areas of colitis between 18 cm to 28 cm of the colon with biopsy revealing patchy, focally active, mild to moderate chronic colitis without evidence of granulomas, dysplasia, or malignancy (Image 1A-1B). The absence of basal lymphoplasmacytosis or granulomas suggested SCAD. He was started on oral mesalamine and a mesalamine suppository, with minimal relief. A trial of oral budesonide was done with relief of symptoms at a dose of 9 mg daily, but with recurrence once the taper was started. A repeat colonoscopy showed severe, localized inflammation of the sigmoid colon (Image 1C). The patient was then referred to surgery and underwent robot-assisted low anterior resection. The patient’s postoperative course was complicated by a small anastomotic leak and peritonitis, with subsequent ileostomy and then reversal thereafter. His symptoms improved significantly after surgery.
Discussion: The prevalence of SCAD in the general population is estimated between 0.25% to 1.4%. In comparison to inflammatory bowel disease (IBD), SCAD is more common in men and presents later in life, usually around the 6th decade. Mucosal prolapse, fecal stasis, and localized ischemia are some of the proposed mechanisms for its pathogenesis. The treatment for SCAD is typically oral 5-ASA, with 80% achieving remission in 6 months. Cases that are refractory to medical therapy may ultimately benefit from surgical resection as in this case, a rare occurrence. In one series, 4/23 (17%) of patients underwent surgery. Compared to inflammatory bowel disease, SCAD is a distinct entity with a self-limited disease course without the need for ongoing treatment.
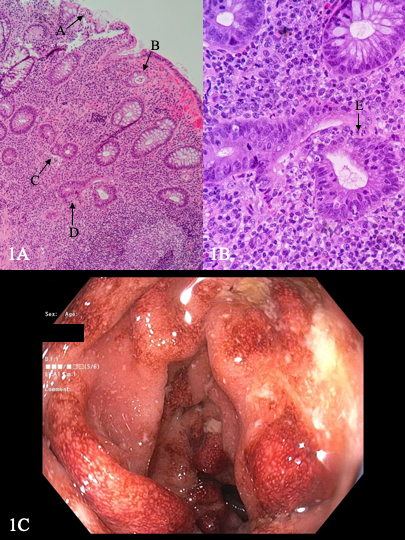
Figure: Image 1A-1B: Photomicrograph of colon biopsies demonstrating erosions (arrow A), neutrophils in the crypt lumen (arrow B), architectural distortion (arrow C and D), and neutrophils in the crypt epithelium (arrow E) without basal lymphoplasmacytosis or granulomas. 1C: Colonoscopy image showing severe inflammation in the sigmoid colon.
Disclosures:
Arvin Jeremy Tan indicated no relevant financial relationships.
Akiko Tokunaga indicated no relevant financial relationships.
Toru Nakata indicated no relevant financial relationships.
Yusuke Miyatani indicated no relevant financial relationships.
Vishal Dobaria indicated no relevant financial relationships.
Traci Murakami indicated no relevant financial relationships.
Arvin Jeremy N. Tan, MD1, Akiko Tokunaga, MD2, Toru Nakata, MD, PhD1, Yusuke Miyatani, MD1, Vishal Dobaria, MD1, Traci T. Murakami, MD, FACG3. P2519 - Cut It Out! Surgical Resection for a Case of Refractory Segmental Colitis Associated With Diverticulosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Hawaii, John A. Burns School of Medicine, Department of Medicine, Honolulu, HI; 2University of Hawaii, John A. Burns School of Medicine, Department of Pathology, Honolulu, HI; 3The Queen's Medical Center, Ewa Beach, HI
Introduction: Segmental Colitis Associated with Diverticulosis (SCAD) is a rare clinical entity characterized by non-specific, segmental thickening of the colonic wall with diverticulosis. The prevalence of SCAD is estimated at 2% to 11% in patients with diverticular disease. Here, we present a case of a patient with SCAD that was refractory to medical therapy and underwent sigmoidectomy.
Case Description/
Methods: A 49-year-old Hispanic and Native American male with a history of hypertension presented to the clinic with a one-month history of progressive hematochezia. This was accompanied by the sensation of incomplete emptying of the rectum and rectal pain. Otherwise, he denied abdominal pain, nausea, vomiting, unintended weight loss, and changes in appetite. During this time, his stools were softer than usual, but he did not have diarrhea. He underwent colonoscopy, which showed areas of colitis between 18 cm to 28 cm of the colon with biopsy revealing patchy, focally active, mild to moderate chronic colitis without evidence of granulomas, dysplasia, or malignancy (Image 1A-1B). The absence of basal lymphoplasmacytosis or granulomas suggested SCAD. He was started on oral mesalamine and a mesalamine suppository, with minimal relief. A trial of oral budesonide was done with relief of symptoms at a dose of 9 mg daily, but with recurrence once the taper was started. A repeat colonoscopy showed severe, localized inflammation of the sigmoid colon (Image 1C). The patient was then referred to surgery and underwent robot-assisted low anterior resection. The patient’s postoperative course was complicated by a small anastomotic leak and peritonitis, with subsequent ileostomy and then reversal thereafter. His symptoms improved significantly after surgery.
Discussion: The prevalence of SCAD in the general population is estimated between 0.25% to 1.4%. In comparison to inflammatory bowel disease (IBD), SCAD is more common in men and presents later in life, usually around the 6th decade. Mucosal prolapse, fecal stasis, and localized ischemia are some of the proposed mechanisms for its pathogenesis. The treatment for SCAD is typically oral 5-ASA, with 80% achieving remission in 6 months. Cases that are refractory to medical therapy may ultimately benefit from surgical resection as in this case, a rare occurrence. In one series, 4/23 (17%) of patients underwent surgery. Compared to inflammatory bowel disease, SCAD is a distinct entity with a self-limited disease course without the need for ongoing treatment.
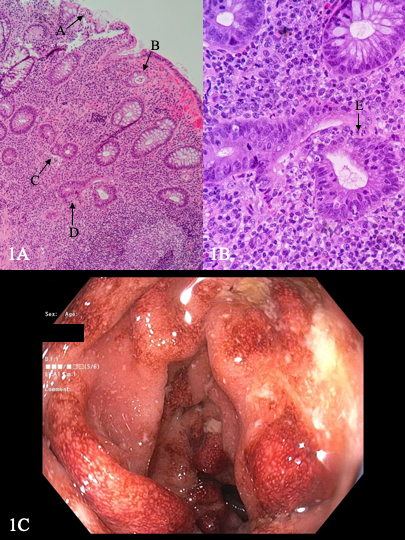
Figure: Image 1A-1B: Photomicrograph of colon biopsies demonstrating erosions (arrow A), neutrophils in the crypt lumen (arrow B), architectural distortion (arrow C and D), and neutrophils in the crypt epithelium (arrow E) without basal lymphoplasmacytosis or granulomas. 1C: Colonoscopy image showing severe inflammation in the sigmoid colon.
Disclosures:
Arvin Jeremy Tan indicated no relevant financial relationships.
Akiko Tokunaga indicated no relevant financial relationships.
Toru Nakata indicated no relevant financial relationships.
Yusuke Miyatani indicated no relevant financial relationships.
Vishal Dobaria indicated no relevant financial relationships.
Traci Murakami indicated no relevant financial relationships.
Arvin Jeremy N. Tan, MD1, Akiko Tokunaga, MD2, Toru Nakata, MD, PhD1, Yusuke Miyatani, MD1, Vishal Dobaria, MD1, Traci T. Murakami, MD, FACG3. P2519 - Cut It Out! Surgical Resection for a Case of Refractory Segmental Colitis Associated With Diverticulosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
