Monday Poster Session
Category: Colon
P2501 - A Surprising Twist: Colonic Ischemia Following Ileocolic Artery Embolization

Fnu Soxi, MD
Jersey City Medical Center
Jersey City, NJ
Presenting Author(s)
Jersey City Medical Center, Jersey City, NJ
Introduction:
Colonic ischemia is a rare but serious complication that can occur post-embolization and has annual mortality rate of 50-75%. Diagnosis can be challenging due to non-specific symptoms and imaging often look like other, non-ischemic conditions. We present case of colonic ischemia after embolization of ileocolic and ascending branch of right colic artery.
Case Description/
Methods:
A 68-year-old male with history of hypertension, diabetes Mellitus, hyperlipidemia, cerebrovascular disease on ASA and diverticulosis presented with multiple episodes of maroon colored stool. On physical examination, abdomen was soft, non-tender. Blood pressure was 76/40 mmHg, heart rate 85/minute. Hemoglobin was 12.1 g/dL. Lactate was 2.1 mmol/L. CT abdomen with IV contrast showed active arterial bleed at the mid ascending colon. Patient was taken for urgent IR guided embolization. The following arteries were embolized:
1. Cecal branch #1 of ileocolic artery,
2. Cecal branch #2 of ileocolic artery,
3. Right colic artery supplying the proximal/mid ascending colon. Ten minutes post procedure patient complained of severe abdominal pain and a large bloody bowel movement. Hemoglobin dropped to 9.3 g/dL.
Repeat CTA showed no active bleed. However, the patient continued to complain of abdominal pain. On examination, patient was tachycardic (HR 130/min) and the abdomen was soft, tender in the right lower quadrant but no guarding or rigidity. Hemoglobin was stable at 9, white blood count increased to 22 and lactate trended up to 5.6. The patient continued to have abdominal pain, prompting a repeat CT scan of the abdomen with IV contrast, showed prominent gas attenuation at the ascending colon wall and peri colonic ascites. The patient was taken to the operating room for an emergent exploratory laparotomy, which revealed frank gangrene involving the ascending colon up to the hepatic flexure, as well as the terminal ileum and appendix, with foul-smelling, murky fluid in the right abdominal cavity.
Discussion:
This case highlights importance of timely decisions and closely monitor patients after procedure. In this patient, the development of frank gangrene of the ascending colon, terminal ileum, and appendix following ileocolic artery embolization underscores the importance of close post-procedural monitoring and maintaining a high index of suspicion for bowel ischemia. Reducing the time to diagnosis remains the most effective way to lower the risk of complications and mortality rate associated with this condition.
Figure: Post embolization: Gas attenuation involving ascending colon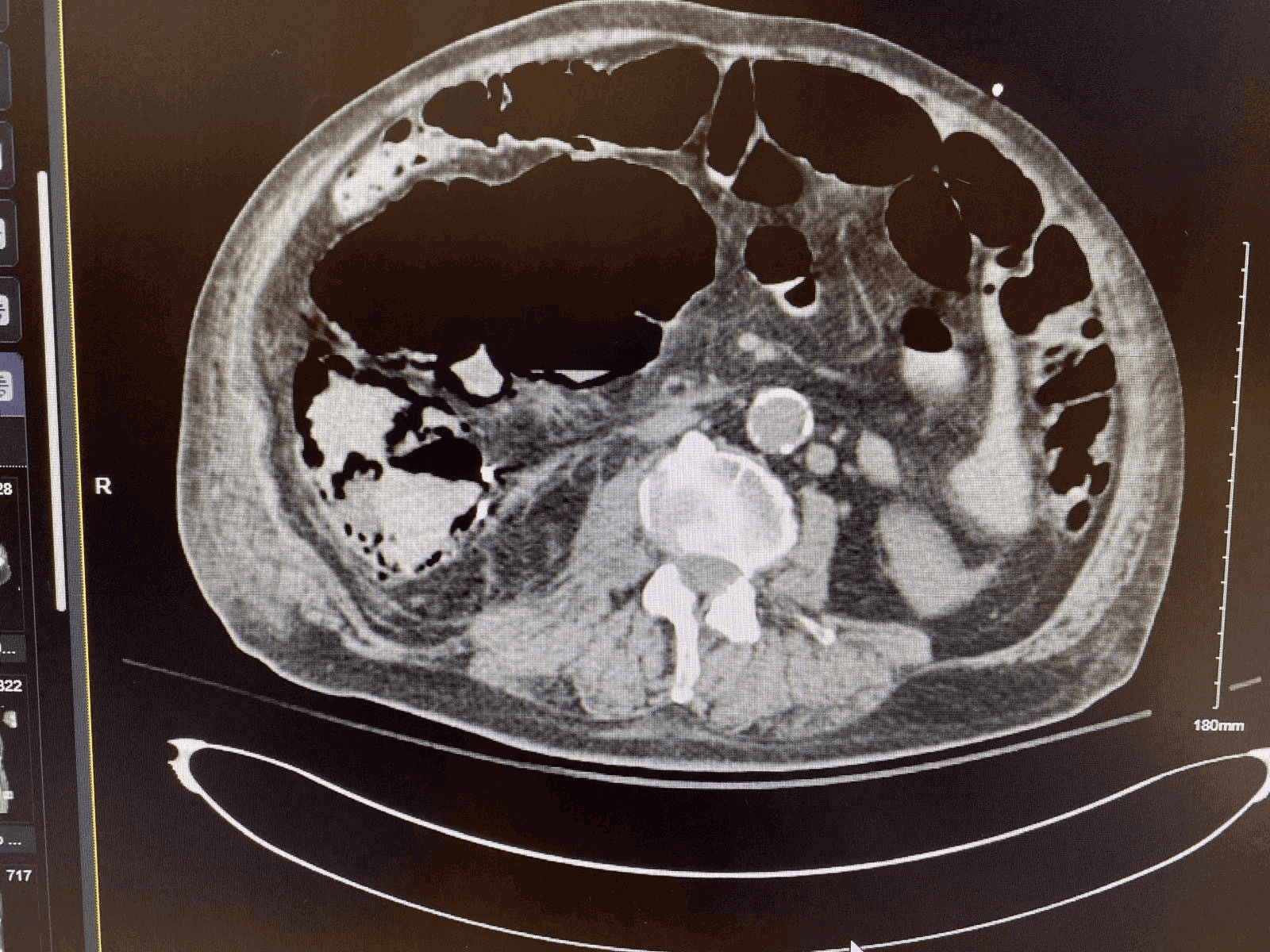
Figure: Post embolization: Gas attenuation involving ascending colon
Disclosures:
Fnu Soxi indicated no relevant financial relationships.
Rabiya Nasr indicated no relevant financial relationships.
Fnu Soxi, MD, Rabiya Nasr, MD. P2501 - A Surprising Twist: Colonic Ischemia Following Ileocolic Artery Embolization, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
