Monday Poster Session
Category: Colon
P2452 - Trends in Mortality Related to Colorectal Cancer Among Adults in the United States, 1999-2023: An Analysis of the CDC WONDER Database

Muhammad Faiq Akram, MBBS
Allama Iqbal Medical College, Lahore
Lahore, Punjab, Pakistan
Presenting Author(s)
1King Edward Medical University, Lahore, Lahore, Punjab, Pakistan; 2Allama Iqbal Medical College, Lahore, Lahore, Punjab, Pakistan; 3Amna Inayat Medical College, Sheikhupura, Pakistan, Lahore, Punjab, Pakistan; 4Liaquat University of Medical and Health Science, Jamshoro, Pakistan, Jamshoro, Sindh, Pakistan; 5Jinnah Sindh Medical University, Karachi, Sindh, Pakistan; 6Dow University of Health Sciences, Karachi, Sindh, Pakistan
Introduction:
Colorectal cancer (CRC) remains the third most commonly diagnosed cancer and the second leading cause of cancer-related deaths in the U.S. Despite advances in screening and treatment that have significantly reduced mortality, significant disparities persist across various population subgroups. This study examines CRC-related mortality trends across demographic and regional subgroups in the U.S. from 1999 to 2023.
Methods:
CRC mortality data for individuals aged ≥25 years were obtained from the CDC WONDER Multiple Cause of Death database using the ICD-10 code C18. Crude mortality rates (CMRs) and age-adjusted mortality rates (AAMRs) were calculated per 100,000 people. Temporal trends were analyzed using Joinpoint regression to determine the annual percent change (APC) and the average annual percent change (AAPC).
Results:
From 1999 to 2023, the U.S. recorded 1,272,568 CRC-related deaths. The overall AAMR declined significantly (AAPC: -2.71%; 95% CI: -2.87 to -2.54), with a steeper drop from 1999 to 2014 (APC: -3.35%), followed by a slower decline after 2014 (APC: -1.63%). Men experienced a higher AAMR (28.20) than women (20.01). Pronounced racial and ethnic disparities were observed, with non-Hispanic (NH) Black individuals experiencing the highest AAMR (32.48), followed by NH White (23.30), NH American Indian/Alaska Native (20.75), Hispanic (17.62), and NH Asian/Pacific Islander (15.08) groups. Regionally, the Midwest reported the highest AAMR (24.80), followed by the South (23.88), Northeast (23.60), and West (21.16). States with the highest AAMRs included Mississippi, West Virginia, the District of Columbia, and Kentucky. Mortality was higher in non-metropolitan areas (AAMR: 26.63) compared to metropolitan areas (AAMR: 23.02). Adults aged ≥65 experienced the highest CMR (91.06). Most deaths occurred at the decedent’s home (40.25%) or in medical facilities (29.74%).
Discussion:
Although CRC mortality in the U.S. has declined over the past 25 years, the rate of decline has notably slowed since 2014. Persistent disparities across sex, race, geographic region, and urbanization level underscore the need for targeted public health strategies. Strengthening healthcare access, increasing screening uptake, and addressing socioeconomic determinants are essential to mitigate these inequities.
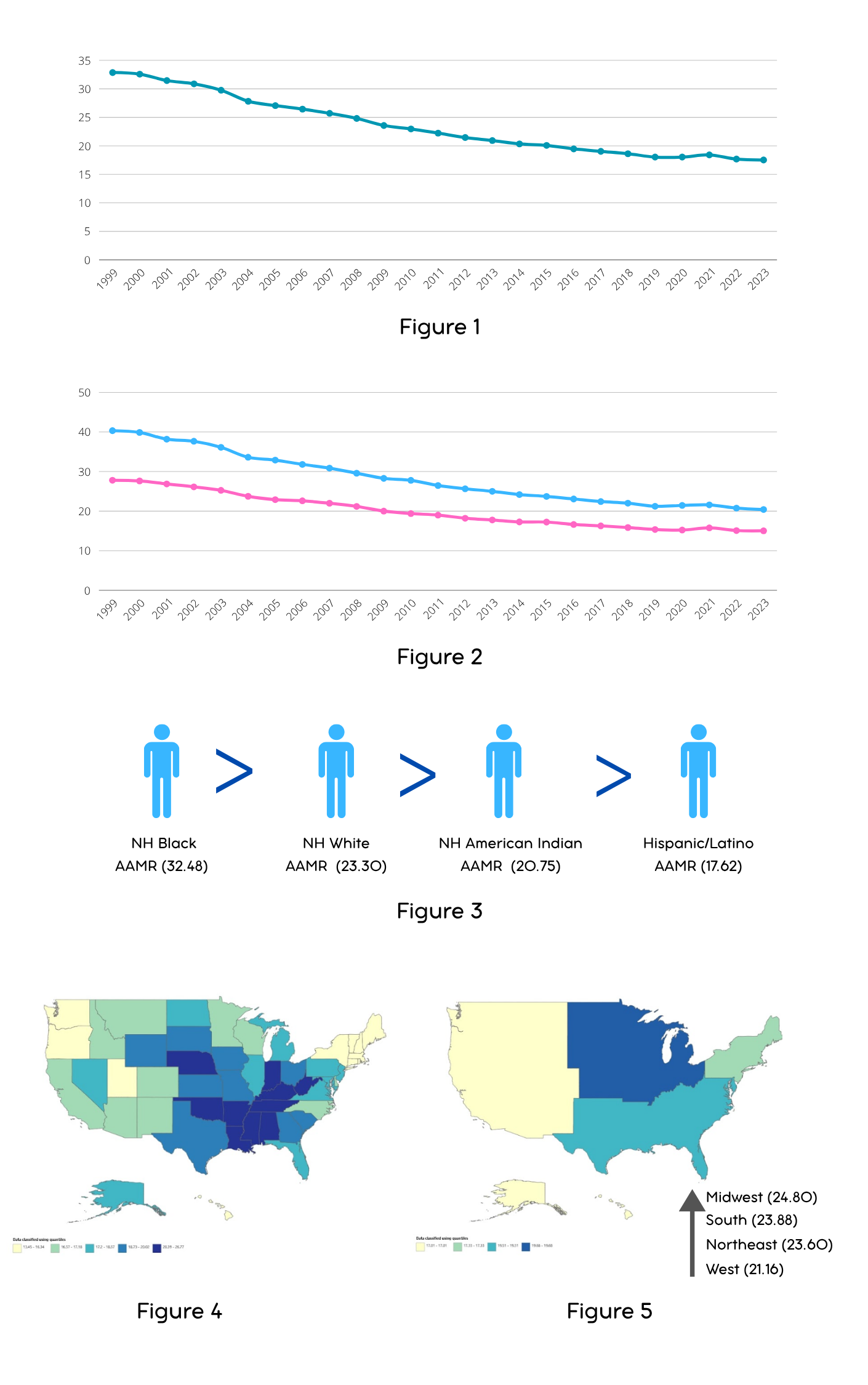
Figure: Figure 1: Overall Age-adjusted Mortality Rates per 100,000 persons
Figure 2: Sex-stratified Trends (Age-adjusted Mortality Rates per 100,000 persons)
Figure 3: Racial Disparities (Age-adjusted Mortality Rates per 100,000 persons)
Figure 4: State-stratified Trends (Age-adjusted Mortality Rates per 100,000 persons)
Figure 5: Census Region-stratified Trends (Age-adjusted Mortality Rates per 100,000 persons)
Disclosures:
Maha Sajjad indicated no relevant financial relationships.
Muhammad Faiq Akram indicated no relevant financial relationships.
Sajjad Hasan indicated no relevant financial relationships.
Muhammad Imaz Bhatti indicated no relevant financial relationships.
Sahil Jairamani indicated no relevant financial relationships.
Maryam Saghir indicated no relevant financial relationships.
Hiba Sohail indicated no relevant financial relationships.
Maha Sajjad, MBBS1, Muhammad Faiq Akram, MBBS2, Sajjad U.. Hasan, MBBS, MPH3, Muhammad Imaz Bhatti, MBBS1, Sahil Jairamani, MBBS4, Maryam Saghir, MBBS5, Hiba Sohail, MBBS6. P2452 - Trends in Mortality Related to Colorectal Cancer Among Adults in the United States, 1999-2023: An Analysis of the CDC WONDER Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
