Monday Poster Session
Category: Colon
P2446 - Prevalence and Inpatient Outcomes of Acute Diverticulitis Among Patients Hospitalized With COVID-19: A Nationwide Analysis

Anwar Uddin, MD (he/him/his)
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction:
SARS-CoV-2, the virus responsible for COVID-19, has demonstrated a tropism for the gastrointestinal tract via ACE2 receptor expression. This may induce inflammation, dysbiosis, and microvascular injury, factors implicated in diverticular disease pathophysiology. However, the prevalence and clinical impact of acute diverticulitis in COVID-19 hospitalizations remain unclear. We aimed to assess its frequency and associated inpatient outcomes in a large, nationally representative cohort.
Methods: We analyzed the 2020 National Inpatient Sample (NIS). COVID-19 hospitalizations were identified via ICD-10-CM codes (U07.1, U00, U49, U50, U85, J12.82, B34.2); acute diverticulitis was identified using ICD-10-CM codes. Primary outcome: in-hospital mortality. Secondary outcomes: length of stay (LOS) and hospitalization cost. Multivariable logistic regression estimated adjusted odds for mortality. Poisson regression assessed LOS. A gamma-distributed GLM with log link modeled cost. All models adjusted for age, sex, race/ethnicity, payer, Charlson comorbidity index (CCI), hospital region, bed size, and teaching status.
Results: Among 1,540,935 COVID-19-related hospitalizations in 2020, 5,465 (0.35%) had a concurrent diagnosis of acute diverticulitis. This prevalence remained stable throughout the year, from 0.25% in March to 0.33% in December (p = 0.11). Compared to patients without diverticulitis, those with diverticulitis had significantly lower in-hospital mortality (10% vs 13%, aOR 0.73, 95% CI: 0.59–0.90, p = 0.003), suggesting a potential protective association. However, these patients experienced a longer hospital stay (9.7 ± 0.34 vs 8.1 ± 0.04 days; adjusted RR 1.23, 95% CI: 1.15–1.32, p < 0.001) and incurred greater hospitalization costs ($29,173 ± 1,564 vs $21,776 ± 231; adjusted RR 1.38, 95% CI: 1.26–1.50, p < 0.001), reflecting increased resource utilization.
Discussion:
Although uncommon, acute diverticulitis among hospitalized COVID-19 patients was associated with lower inpatient mortality despite significantly longer LOS and higher costs. The reduced mortality may reflect earlier clinical recognition, increased diagnostic testing, or patient selection with milder respiratory illness. Nonetheless, the elevated resource use underscores the importance of identifying and managing gastrointestinal comorbidities in COVID-19 hospitalizations. Further investigation is warranted to explore the underlying mechanisms and guide evidence-based management strategies in this population.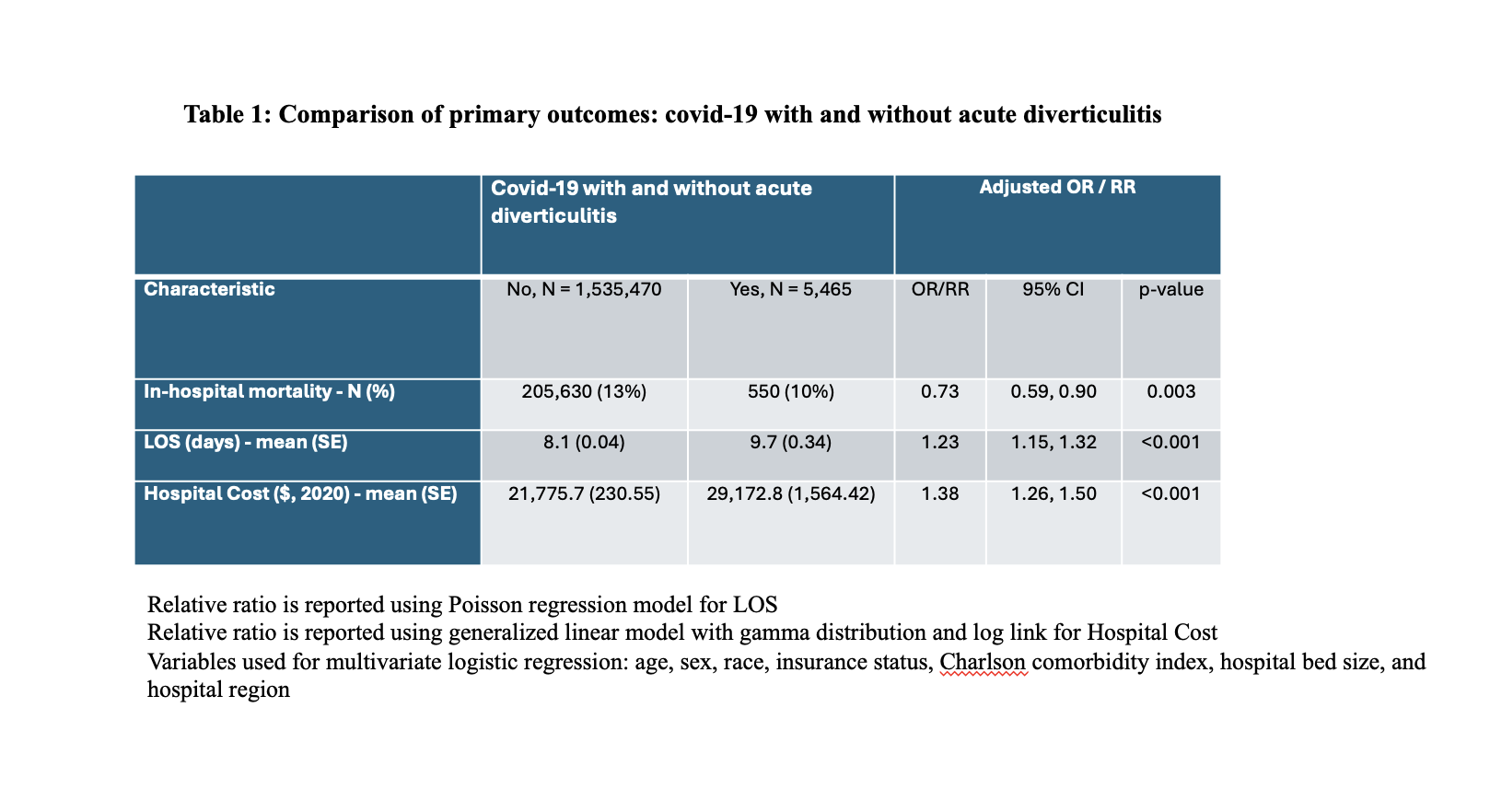
Figure: Table 1: Comparison of Primary Outcome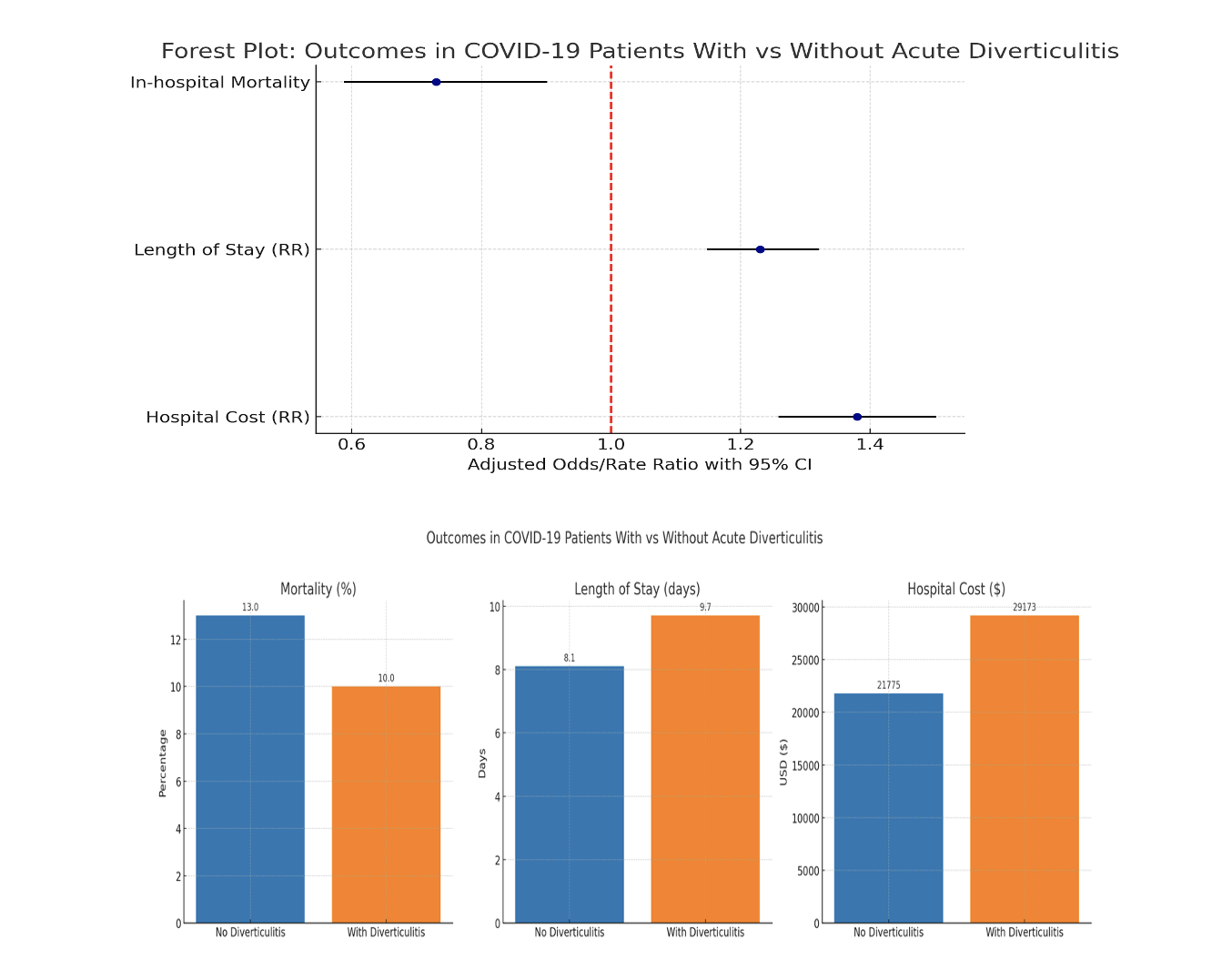
Figure: Figure 1 and Figure 2: Forest Plot of Odds ratio of outcomes and Bar Chart of Outcomes
Disclosures:
Anwar Uddin indicated no relevant financial relationships.
Madia Ahad indicated no relevant financial relationships.
Narinderjeet Kaur indicated no relevant financial relationships.
Peter Lymberopoulos indicated no relevant financial relationships.
Rafat Uddin indicated no relevant financial relationships.
Savanna Thor indicated no relevant financial relationships.
Anwar Uddin, MD, Madia Ahad, MD, Narinderjeet Kaur, MD, MS, Peter Lymberopoulos, MD, Rafat Uddin, MS, Savanna Thor, DO, MPH. P2446 - Prevalence and Inpatient Outcomes of Acute Diverticulitis Among Patients Hospitalized With COVID-19: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
