Monday Poster Session
Category: Colon
P2437 - Factors Associated With Patient Selection for Endoscopic Evaluation of Immune Checkpoint Inhibitor Colitis: A Retrospective Study

Sapana Gupta, MD
Brown University / Rhode Island Hospital
Providence, RI
Presenting Author(s)
Sapana Gupta, MD1, Jacqueline J. Chu, MD, MS1, Curtis Petruzzelli, MD1, MacKenzie Adams, MD1, Charmi Trivedi, MD1, Kanika Malani, MD2, William Park, MD1, Rebecca Steuer, MD1, Maria Constantinou, MD1, Galina Lagos, MD1, Megan Begnoche, RN1, Sandeep Jain, MD1, May Min, MD1, Matthew Hadfield, MD1
1Brown University / Rhode Island Hospital, Providence, RI; 2Yale New Haven Hospital, New Haven, CT
Introduction:
Immune checkpoint inhibitors (ICIs) are now widely utilized in both solid and hematological malignancies. Immune related adverse events (irAEs) develop because of autoimmune inflammation of healthy tissue, such as colitis. Current guidelines recommend imaging and endoscopy for patients with colitis or diarrhea grade ≥2, based on the Common Terminology Criteria for Adverse Events (CTCAE). Despite these recommendations, real-world adherence to endoscopic evaluation remains unclear. We characterize factors influencing the decision to pursue endoscopy in patients with ICI colitis and assess the clinical implications.
Methods:
Records from a tertiary care center were reviewed to identify patients who received ICIs between 2015 and 2024. Of 2,723 patients on ICIs, 102 were diagnosed with ICI colitis, defined as systemic steroid initiation for colitis or diarrhea symptoms. CTCAE grading system for diarrhea and enterocolitis was used. Patients were stratified based on whether they underwent endoscopy for evaluation of ICI colitis. Univariate regression and descriptive analyses were used to assess differences between the groups.
Results:
Of the 102 patients with ICI colitis, 6 (5.9%) had grade 1 diarrhea and 96 (94%) had grade ≥2. Of those with diarrhea grade ≥2, 68 (71%) did not receive endoscopic evaluation. Similarly, of the 102 patients with ICI colitis, 2 (2.0%) had grade 1 colitis, 50 (49%) had grade ≥2 colitis, and 50 (49%) had an unknown colitis grade. Of those with known colitis grade ≥2, 29 (58%) did not receive an endoscopy for ICI colitis diagnosis. Despite guideline recommendations, endoscopic evaluation was underutilized in patients with grade ≥2 ICI colitis. Hospital admission and concurrent CT imaging were associated with higher rates of endoscopic evaluation, suggesting that acuity and care setting may drive decision-making more than standardized criteria. These findings underscore the need for improved coordination between oncology and gastroenterology to ensure appropriate diagnostic evaluation.
There was no significant difference in overall survival between those who did and did not undergo endoscopy (36.0 vs. 37.0 months, p = 0.837). Patients who underwent endoscopy were more likely to have had CT imaging at diagnosis (89.7% vs. 61.6%, p = 0.006) and to require hospitalization (82.8% vs. 34.2%, p < 0.001). There were no significant differences in laboratory markers between groups.
Discussion: 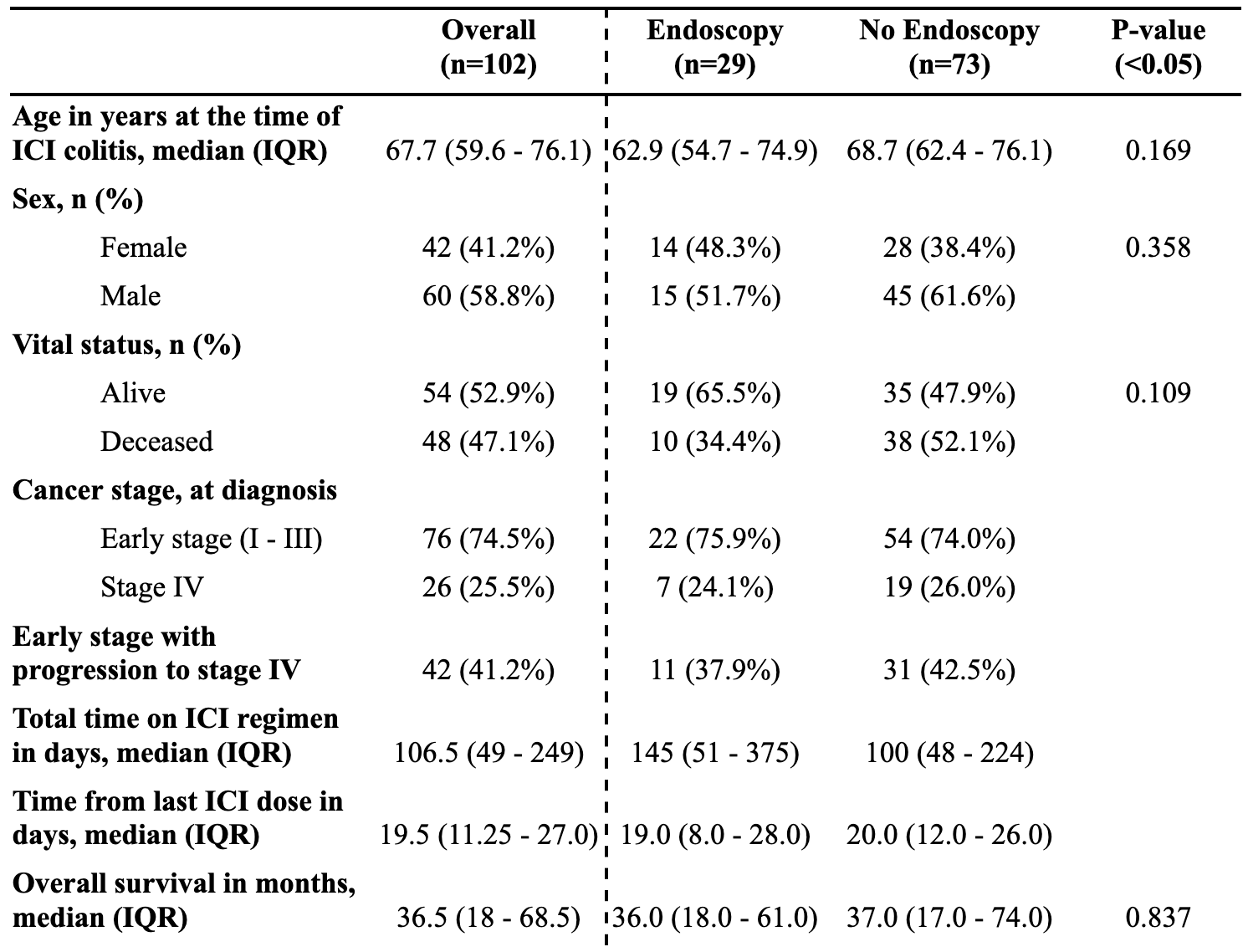
Figure: Table 1: Characteristics of patients with ICI colitis at presentation 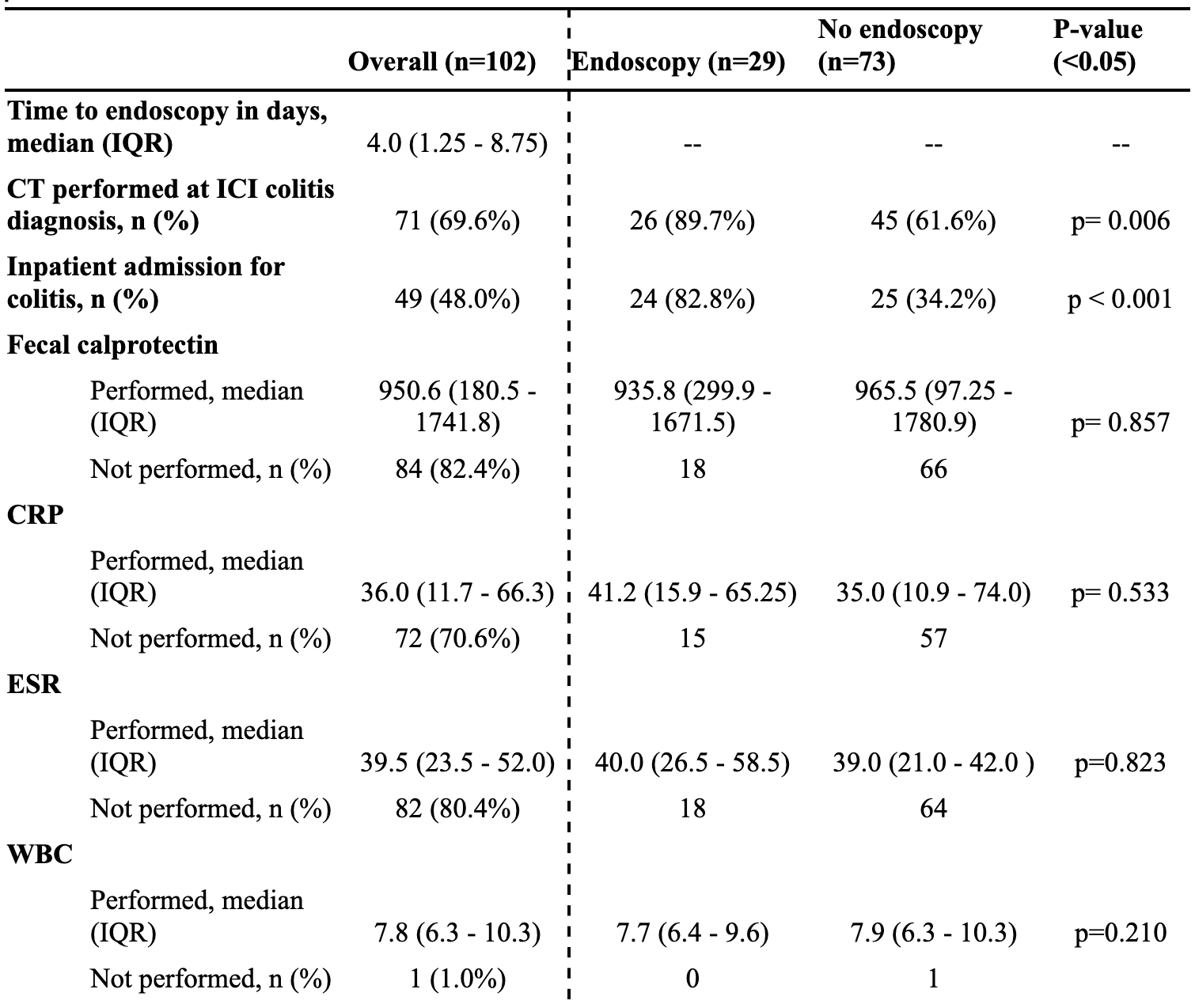
Figure: Table 2: Factors that may influence the decision to perform endoscopy in patients with ICI colitis
Disclosures:
Sapana Gupta indicated no relevant financial relationships.
Jacqueline Chu indicated no relevant financial relationships.
Curtis Petruzzelli indicated no relevant financial relationships.
MacKenzie Adams indicated no relevant financial relationships.
Charmi Trivedi indicated no relevant financial relationships.
Kanika Malani indicated no relevant financial relationships.
William Park indicated no relevant financial relationships.
Rebecca Steuer indicated no relevant financial relationships.
Maria Constantinou indicated no relevant financial relationships.
Galina Lagos indicated no relevant financial relationships.
Megan Begnoche indicated no relevant financial relationships.
Sandeep Jain indicated no relevant financial relationships.
May Min indicated no relevant financial relationships.
Matthew Hadfield indicated no relevant financial relationships.
Sapana Gupta, MD1, Jacqueline J. Chu, MD, MS1, Curtis Petruzzelli, MD1, MacKenzie Adams, MD1, Charmi Trivedi, MD1, Kanika Malani, MD2, William Park, MD1, Rebecca Steuer, MD1, Maria Constantinou, MD1, Galina Lagos, MD1, Megan Begnoche, RN1, Sandeep Jain, MD1, May Min, MD1, Matthew Hadfield, MD1. P2437 - Factors Associated With Patient Selection for Endoscopic Evaluation of Immune Checkpoint Inhibitor Colitis: A Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

