Monday Poster Session
Category: Colon
P2434 - Analyzing Surgical and Pathological Outcomes in Three-Port vs Five-Port Laparoscopic Colectomy for Colon Cancer: A Systematic Review and Meta Analysis

Simran Joshi, MD
Yale New Haven Health, Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
1Yale New Haven Health, Bridgeport Hospital, Bridgeport, CT; 2CMH Lahore Medical College, Lahore, Punjab, Pakistan; 3Andhra Medical College, Visakhapatnam, Andhra Pradesh, India; 4Jaipur national university institute for medical sciences and research center, Jaipur, Rajasthan, India; 5University of Michigan, Ann Arbor, MI; 6CMH Kharian, Sarghoda, Punjab, Pakistan; 7Yale New Haven Health, Bridgeport, CT
Introduction:
Minimally invasive laparoscopic colectomy incorporating a five-port approach is the current standard procedure for colon cancer resection. Novel variations in laparoscopic surgery such as three port laparoscopic colectomy (TPLRC) have emerged, reducing surgical trauma and enhancing recovery. However, specific evidence on the efficacy and safety of three-port approach is inconclusive. Evaluating port-related outcomes is critical for optimizing surgical strategies, perioperative and postoperative care. Therefore, this systematic review and meta-analysis compares TPLRC versus five-port laparoscopic colectomy (FPLRC) in colon cancer.
Methods:
A comprehensive literature search was conducted on MEDLINE (PubMed), Embase (Ovid), Scopus and Cochrane Library from inception to 21st May 2025, following PRISMA guidelines. Key surgical and pathological outcomes were evaluated. Mean Difference (MD) with 95% confidence intervals (CI) were calculated for continuous outcomes and risk ratios (RRs) with 95% CI for dichotomous outcomes. ROBINS-I tool was used for the risk of bias assessment. Meta-analysis was performed on Review Manager (RevMan) 5.4.1 using the random-effects model. I² statistic was used to assess heterogeneity.
Results:
Three non-randomized studies comprising 423 patients (TPLRC 199 and FPLRC 224; 52.25% female, mean age 66.43 ± 10.72) met the inclusion criteria. TPLRC significantly reduced operative time (MD: -26.33, 95% CI: -44.75 to -7.91, p = 0.005, I2 = 86%, Figure 1A) and estimated blood loss (MD: -54.27, 95% CI: -74.46 to -34.08, p < 0.001, I2 = 0%, Figure 1B). A significantly higher number of lymph nodes were harvested using TPLRC compared with FPLRC (MD: 3.78, 95% CI: 2.41 to 5.14, p < 0.001, I2 = 0%, Figure 1C). However, there were no significant differences in postoperative hospital stay (MD: 0.03, 95% CI: -0.46 to 0.52, p = 0.90, I2 = 0%, Figure 1D), time to first passage of flatus (MD: -0.25, 95% CI: -1.29 to 0.80, p = 0.64, I2 = 93%, Figure 1E), time to first oral diet (MD: 0.11, 95% CI: -1.37 to 1.59, p = 0.89, I2 = 94%, Figure 1F), and adverse events (RR: 0.83, 95% CI: 0.29 to 2.36, p = 0.72, I2 = 85%, Figure 1G) between the two groups.
Discussion:
TPLRC in patients with colon cancer improved peri-operative outcomes and oncological yield without compromising safety and patient recovery compared with FPLRC. Further large multicenter randomized controlled trials are warranted to validate these findings and inform clinical guidelines.
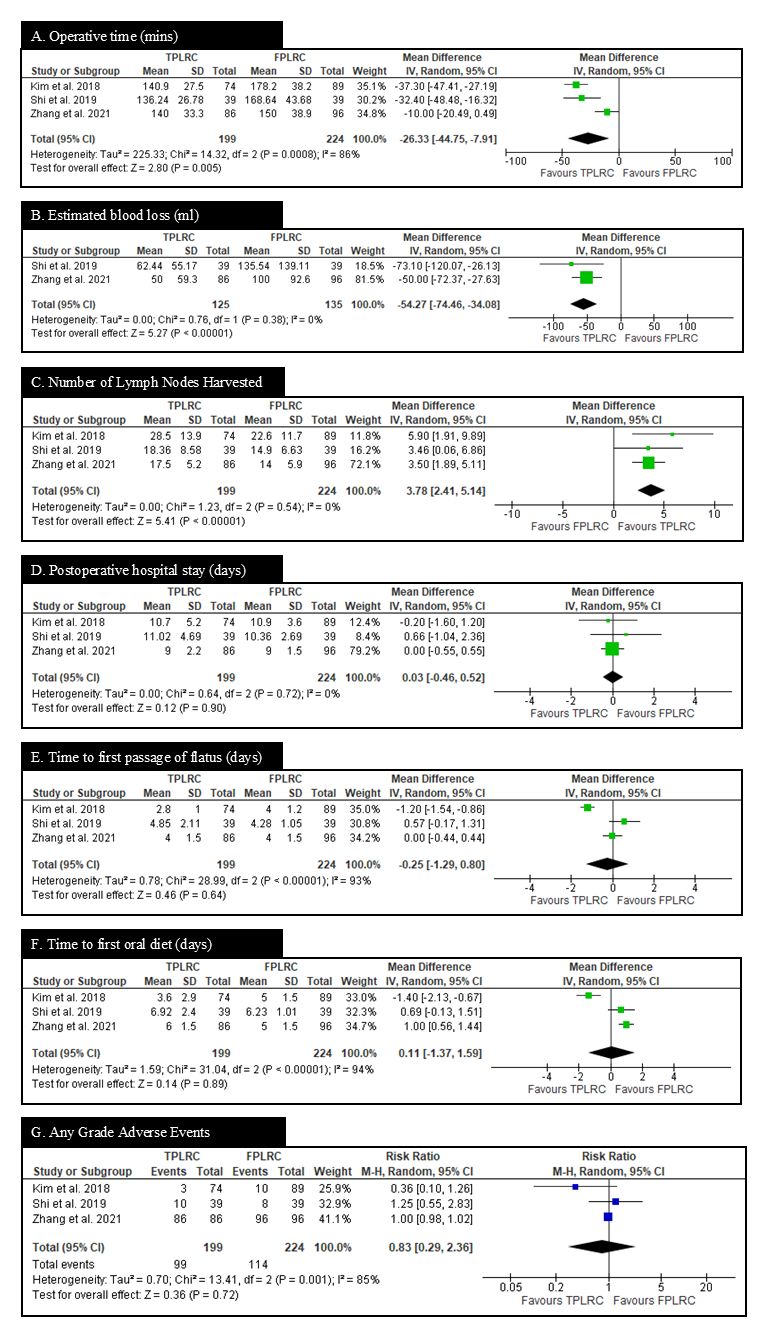
Figure: Figure 1. Forest plots comparing outcomes between Three-Port and Five-Port Laparoscopic Colectomy
Disclosures:
Simran Joshi indicated no relevant financial relationships.
Khawaja Abdul Rehman indicated no relevant financial relationships.
Sri Anjali Gorle indicated no relevant financial relationships.
Gaurav Sharma indicated no relevant financial relationships.
Syed Hassan indicated no relevant financial relationships.
Saman Javaid indicated no relevant financial relationships.
Corinne Caissie indicated no relevant financial relationships.
Mohammad Islam indicated no relevant financial relationships.
Cheng-Hung Tai indicated no relevant financial relationships.
Simran Joshi, MD1, Khawaja Abdul Rehman, MBBS2, Sri Anjali Gorle, 3, Gaurav Sharma, MBBS4, Syed A. Hassan, MBBS5, Saman Javaid, MBBS6, Corinne Caissie, MD1, Mohammad Islam, MD7, Cheng-Hung Tai, MD1. P2434 - Analyzing Surgical and Pathological Outcomes in Three-Port vs Five-Port Laparoscopic Colectomy for Colon Cancer: A Systematic Review and Meta Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
