Monday Poster Session
Category: Colon
P2418 - Cold vs Hot Snare Endoscopic Mucosal Resection for Large Nonpedunculated Colorectal Polyps: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ali Emre Bardak, MD
St. Elizabeth's Medical Center, Boston University School of Medicine
Boston, MA
Presenting Author(s)
Ali Emre Bardak, MD1, Stefan Mitev, MD2, Yusuf Yalcin, MD3, Saqr Alsakarneh, MD, MS4, Gizem Teker, MD5, Nazli Begum Ozturk, MD6, Merve Gurakar, MD, MPH7, Kavin Kanthasamy, MD8
1St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA; 2University Hospital St Ivan Rilski, Sofiya, Sofiya, Bulgaria; 3Boston Medical Center - South, Boston, MA; 4Mayo Clinic, Kansas City, MO; 5Istanbul University, Istanbul, Istanbul, Turkey; 6Corewell Health William Beaumont University Hospital, Royal Oak, MI; 7Johns Hopkins University School of Medicine, Baltimore, MD; 8Houston Methodist Hospital, Houston, TX
Introduction: Endoscopic mucosal resection (EMR) is pivotal in managing large nonpedunculated colorectal polyps (LNPCPs). While hot snare EMR (HS-EMR) is traditionally favored for its lower recurrence rates, cold snare EMR (CS-EMR) has attracted interest due to its superior safety profile. We aimed to compare CS-EMR and HS-EMR in terms of efficacy and safety outcomes for the removal of LNPCPs.
Methods: We systematically searched PubMed, Embase, and Cochrane databases through February 2025 to identify randomized controlled trials comparing CS-EMR with HS-EMR in LNPCPs. Recurrence rate and safety profile were the outcomes of interest. Data were pooled using random-effects models with subgroup analyses based on polyp size and histologic subtype.
Results: Four studies were included in the meta-analysis. Of these, three were full-text articles and one was an abstract. Three studies examined colorectal polyps larger than 20 mm, while one study included polyps larger than 15 mm. In this study, the median polyp size was 30 mm (IQR 25-35). A total of 1,429 patients and 1,516 polyps were included. Of these, 722 patients (50.5%) and 766 polyps (50.5%) underwent CS-EMR. The risk of recurrence in the CS-EMR was significantly higher (≥15 mm: RR 2.02, 95% CI 1.44-2.84; ≥20 mm: RR 1.91, 95% CI 1.50-2.43). The subgroup including adenomatous polyps showed similar trends (≥15 mm: RR 2.05, 95% CI 1.38-3.03; ≥20 mm: RR 1.93, 95% CI 1.49-2.50), whereas the risk of recurrence in sessile serrated polyps (SSP) did not differ significantly (≥20 mm: RR 2.00, 95% CI 0.59-6.79). Safety outcomes favored CS-EMR, with lower risks of perforation (RR 0.11, 95% CI 0.02-0.63), postprocedural bleeding (RR 0.34, 95% CI 0.13–0.88), and clip closure (RR 0.35, 95% CI 0.16-0.78), while intraprocedural bleeding (RR 0.58, 95% CI 0.30-1.10) and postpolypectomy syndrome (RR 0.60, 95% CI 0.24-1.46) were similar.
Discussion: Our meta-analysis shows that CS-EMR offers a safer profile with significantly lower perforation and postprocedural bleeding rates in the removal of LNPCPs. As for the recurrence risk, it is higher with CS-EMR compared to HS-EMR for the large nonpedunculated adenomatous polyps, while it did not reach statistical significance for sessile serrated polyps. These findings support current guidelines favoring HS-EMR for large nonpedunculated adenomatous polyps while highlighting that CS-EMR may be a viable alternative in select clinical scenarios.
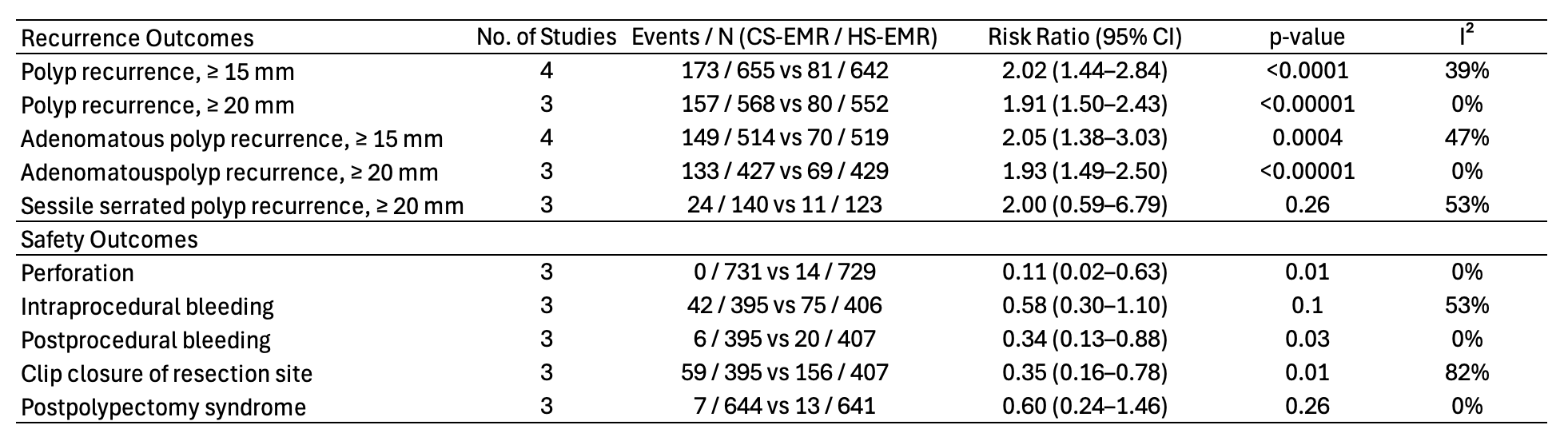
Figure: Figure 1: Baseline characteristics of patients in included studies. † Values are presented as mean ± standard deviation, ‡ values are presented as median (interquartile range), § first endoscopic follow-up, ¶ interval for the first endoscopic follow-up as specified in the study protocol. ASA = American Society of Anesthesiologists, N/A = Not available.
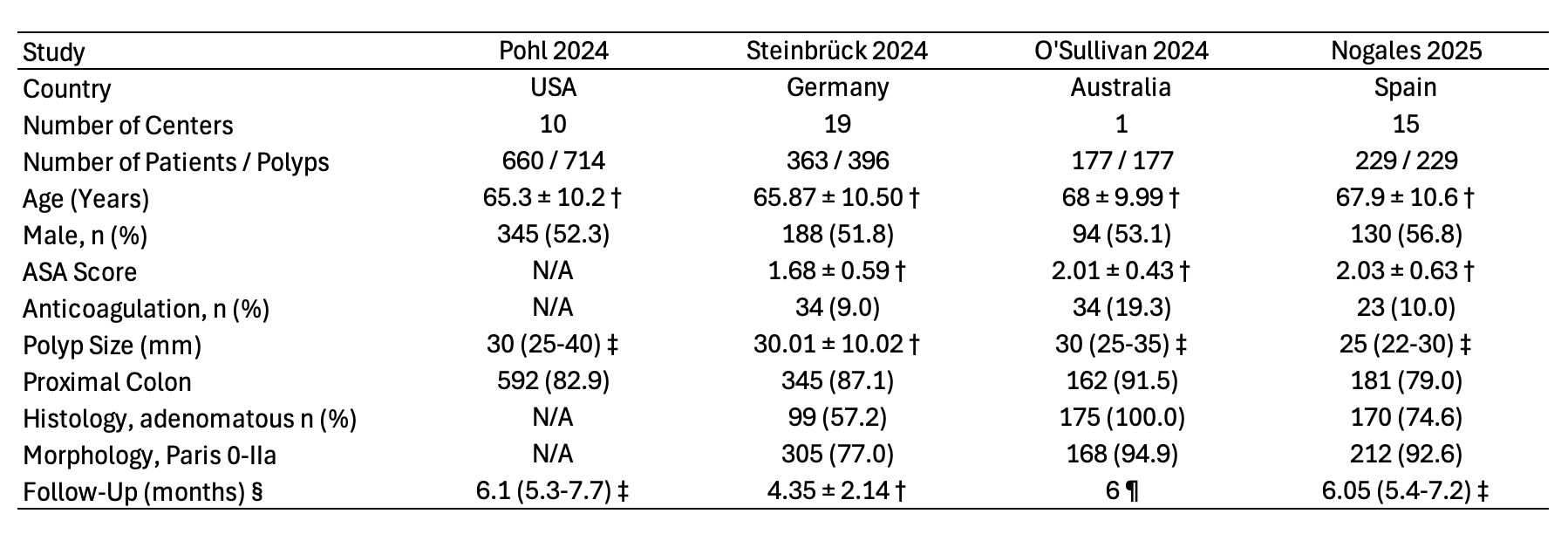
Figure: Figure 2: Pooled recurrence and safety outcomes comparing CS-EMR versus HS-EMR. CS-EMR = cold snare endoscopic mucosal resection ; HS-EMR = hot snare endoscopic mucosal resection.
Disclosures:
Ali Emre Bardak indicated no relevant financial relationships.
Stefan Mitev indicated no relevant financial relationships.
Yusuf Yalcin indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Gizem Teker indicated no relevant financial relationships.
Nazli Begum Ozturk indicated no relevant financial relationships.
Merve Gurakar indicated no relevant financial relationships.
Kavin Kanthasamy indicated no relevant financial relationships.
Ali Emre Bardak, MD1, Stefan Mitev, MD2, Yusuf Yalcin, MD3, Saqr Alsakarneh, MD, MS4, Gizem Teker, MD5, Nazli Begum Ozturk, MD6, Merve Gurakar, MD, MPH7, Kavin Kanthasamy, MD8. P2418 - Cold vs Hot Snare Endoscopic Mucosal Resection for Large Nonpedunculated Colorectal Polyps: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Elizabeth's Medical Center, Boston University School of Medicine, Boston, MA; 2University Hospital St Ivan Rilski, Sofiya, Sofiya, Bulgaria; 3Boston Medical Center - South, Boston, MA; 4Mayo Clinic, Kansas City, MO; 5Istanbul University, Istanbul, Istanbul, Turkey; 6Corewell Health William Beaumont University Hospital, Royal Oak, MI; 7Johns Hopkins University School of Medicine, Baltimore, MD; 8Houston Methodist Hospital, Houston, TX
Introduction: Endoscopic mucosal resection (EMR) is pivotal in managing large nonpedunculated colorectal polyps (LNPCPs). While hot snare EMR (HS-EMR) is traditionally favored for its lower recurrence rates, cold snare EMR (CS-EMR) has attracted interest due to its superior safety profile. We aimed to compare CS-EMR and HS-EMR in terms of efficacy and safety outcomes for the removal of LNPCPs.
Methods: We systematically searched PubMed, Embase, and Cochrane databases through February 2025 to identify randomized controlled trials comparing CS-EMR with HS-EMR in LNPCPs. Recurrence rate and safety profile were the outcomes of interest. Data were pooled using random-effects models with subgroup analyses based on polyp size and histologic subtype.
Results: Four studies were included in the meta-analysis. Of these, three were full-text articles and one was an abstract. Three studies examined colorectal polyps larger than 20 mm, while one study included polyps larger than 15 mm. In this study, the median polyp size was 30 mm (IQR 25-35). A total of 1,429 patients and 1,516 polyps were included. Of these, 722 patients (50.5%) and 766 polyps (50.5%) underwent CS-EMR. The risk of recurrence in the CS-EMR was significantly higher (≥15 mm: RR 2.02, 95% CI 1.44-2.84; ≥20 mm: RR 1.91, 95% CI 1.50-2.43). The subgroup including adenomatous polyps showed similar trends (≥15 mm: RR 2.05, 95% CI 1.38-3.03; ≥20 mm: RR 1.93, 95% CI 1.49-2.50), whereas the risk of recurrence in sessile serrated polyps (SSP) did not differ significantly (≥20 mm: RR 2.00, 95% CI 0.59-6.79). Safety outcomes favored CS-EMR, with lower risks of perforation (RR 0.11, 95% CI 0.02-0.63), postprocedural bleeding (RR 0.34, 95% CI 0.13–0.88), and clip closure (RR 0.35, 95% CI 0.16-0.78), while intraprocedural bleeding (RR 0.58, 95% CI 0.30-1.10) and postpolypectomy syndrome (RR 0.60, 95% CI 0.24-1.46) were similar.
Discussion: Our meta-analysis shows that CS-EMR offers a safer profile with significantly lower perforation and postprocedural bleeding rates in the removal of LNPCPs. As for the recurrence risk, it is higher with CS-EMR compared to HS-EMR for the large nonpedunculated adenomatous polyps, while it did not reach statistical significance for sessile serrated polyps. These findings support current guidelines favoring HS-EMR for large nonpedunculated adenomatous polyps while highlighting that CS-EMR may be a viable alternative in select clinical scenarios.
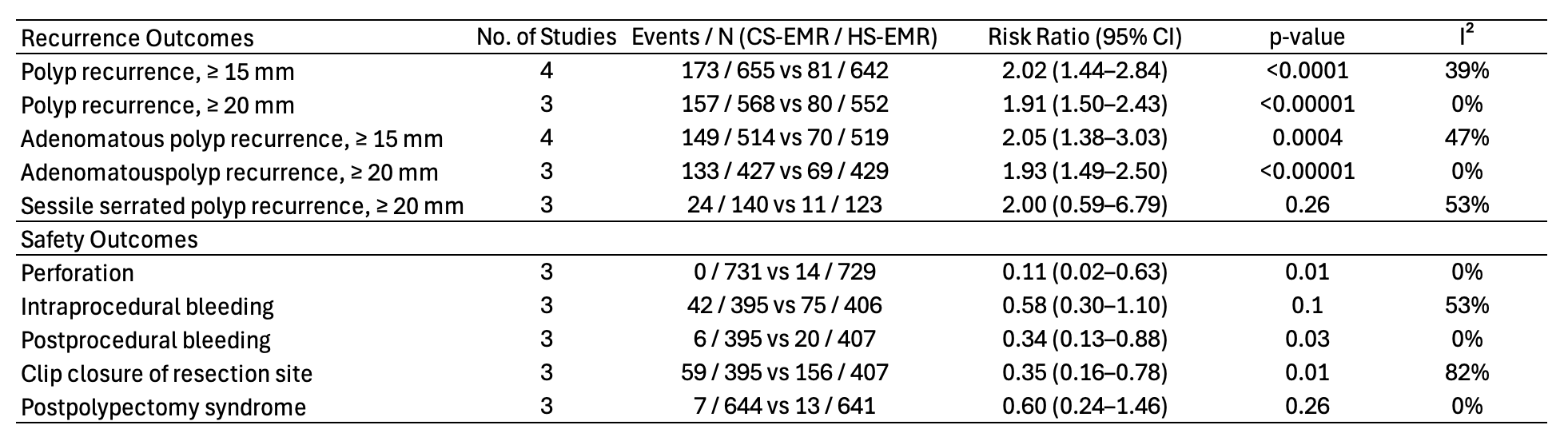
Figure: Figure 1: Baseline characteristics of patients in included studies. † Values are presented as mean ± standard deviation, ‡ values are presented as median (interquartile range), § first endoscopic follow-up, ¶ interval for the first endoscopic follow-up as specified in the study protocol. ASA = American Society of Anesthesiologists, N/A = Not available.
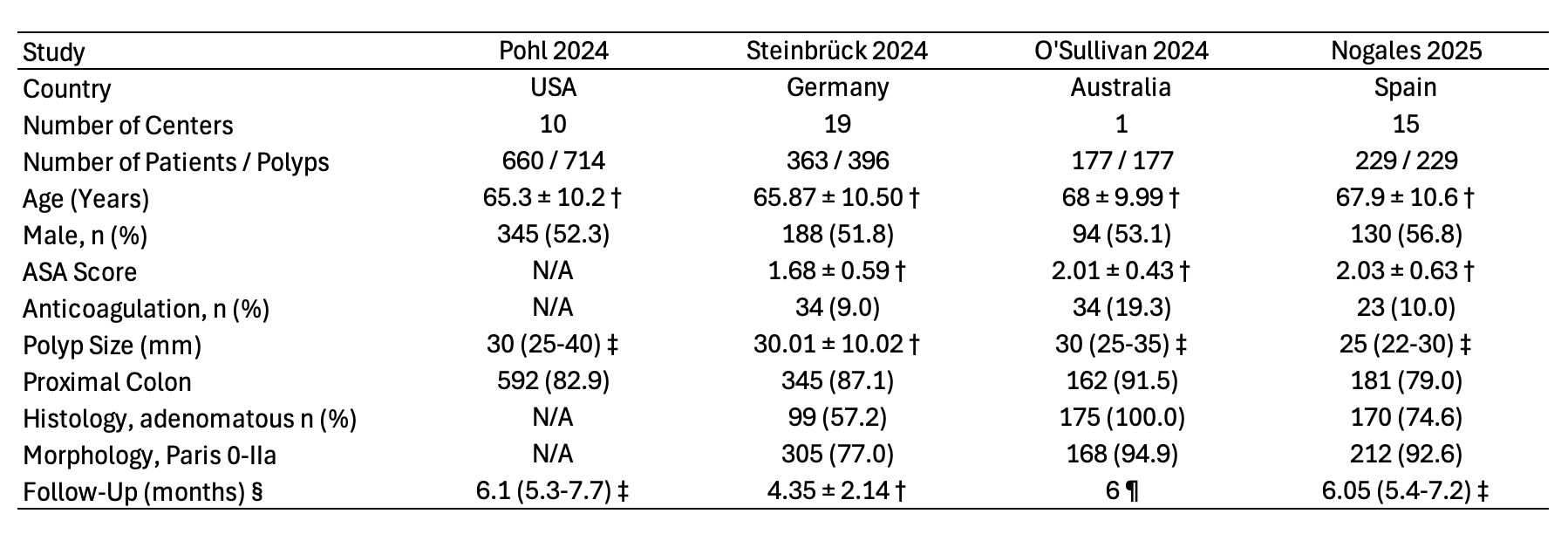
Figure: Figure 2: Pooled recurrence and safety outcomes comparing CS-EMR versus HS-EMR. CS-EMR = cold snare endoscopic mucosal resection ; HS-EMR = hot snare endoscopic mucosal resection.
Disclosures:
Ali Emre Bardak indicated no relevant financial relationships.
Stefan Mitev indicated no relevant financial relationships.
Yusuf Yalcin indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Gizem Teker indicated no relevant financial relationships.
Nazli Begum Ozturk indicated no relevant financial relationships.
Merve Gurakar indicated no relevant financial relationships.
Kavin Kanthasamy indicated no relevant financial relationships.
Ali Emre Bardak, MD1, Stefan Mitev, MD2, Yusuf Yalcin, MD3, Saqr Alsakarneh, MD, MS4, Gizem Teker, MD5, Nazli Begum Ozturk, MD6, Merve Gurakar, MD, MPH7, Kavin Kanthasamy, MD8. P2418 - Cold vs Hot Snare Endoscopic Mucosal Resection for Large Nonpedunculated Colorectal Polyps: A Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
