Monday Poster Session
Category: Colon
P2412 - Endoscopic Mucosal Resection vs Endoscopic Submucosal Dissection for Non-Pedunculated 20-40 mm Colonic Lesions: An Enhanced Markov Model Accounting for Recurrence, Recovery, and Adverse Events
- RB
Rami Basmaci, MD (he/him/his)
East Carolina University Medical Center
Greenville, NC
Presenting Author(s)
1East Carolina University Medical Center, Greenville, NC; 2East Carolina Gastroenterology, Greenville, NC; 3University of Kansas School of Medicine, Kansas City, KS; 4Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 5Mayo Clinic, Rochester, MN, USA., Rochester, MN
Introduction:
Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are standard approaches for 20–40 mm nonpedunculated colorectal polyps. While ESD achieves higher en bloc and R0 resection rates, it is technically demanding and resource intensive. We developed an enhanced Markov model comparing EMR and ESD over 5 years, incorporating recurrence, adverse events, surveillance burden, procedure time, and productivity loss.
Methods:
A 5-state Markov model (Initial, En Bloc, Recurrence, Surgery, Death) was applied to a hypothetical cohort of 1,000 patients over five 1-year cycles. Transition probabilities, recurrence rates, and adverse event frequencies were derived from published literature. Perforation and bleeding rates were assigned to both strategies (EMR: 2%/6%; ESD: 5%/4%). Utility decrements were applied for post-procedure recovery, complications, and surveillance. Costs included procedural fees, operating room time ($10/min), and productivity loss ($400/day). Outcomes were expressed as total costs, quality-adjusted life years (QALYs), and incremental cost-effectiveness ratios (ICERs) at a 3% discount rate.
Results:
Over the 5-year simulation period, the EMR strategy resulted in 3,628 total QALYs at a cost of $25.3 million, while the ESD strategy produced 3,847 QALYs at $39.4 million. This yielded an incremental gain of 218 QALYs at an additional $14.2 million, resulting in an ICER of $64,860 per QALY gained.
The model incorporated multiple real-world factors. Adverse event rates (EMR: 2% perforation, 6% bleeding; ESD: 5% perforation, 4% bleeding) increased procedural costs and modestly reduced QALYs. Surveillance burden was higher after EMR due to more frequent recurrence, adding both cost and quality-of-life penalties. Recovery-related productivity loss was incorporated, with EMR incurring 1 day off work, ESD 3 days, and surgery 21 days.
Finally, differences in recurrence were used to simulate R0 resection vs positive margins — ESD's higher en bloc and curative resection rates translated to fewer recurrences and better long-term QALYs. These enhancements provide a realistic and comprehensive view of downstream outcomes and resource needs.
Discussion:
ESD provides superior long-term outcomes compared to EMR for large nonpedunculated colonic polyps and remains cost-effective under standard willingness-to-pay thresholds. These findings support investment in advanced endoscopic training and procedural planning for optimized outcomes in colorectal neoplasia management.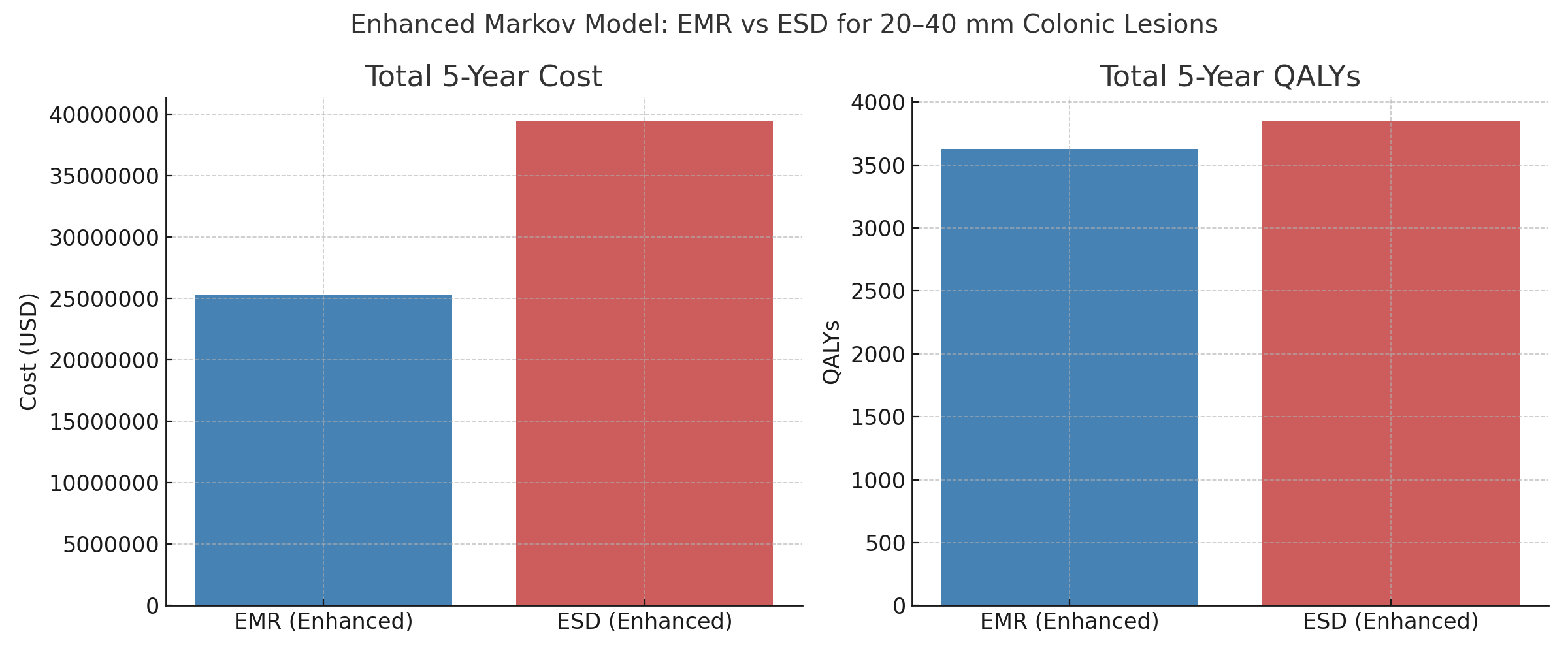
Figure: Figure 1.
Enhanced Markov model comparison of total 5-year cost (USD) and quality-adjusted life years (QALYs) for EMR versus ESD in 1,000 patients with nonpedunculated 20–40 mm colonic lesions.
Disclosures:
Rami Basmaci indicated no relevant financial relationships.
Hassam Ali indicated no relevant financial relationships.
Shiza Sarfraz indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Farah Fleti indicated no relevant financial relationships.
Eslam Ali indicated no relevant financial relationships.
Rami Basmaci, MD1, Hassam Ali, MD2, Shiza Sarfraz, MD1, Dushyant S. Dahiya, MD3, Umar Hayat, MD4, Farah Fleti, MD5, Eslam Ali, MD1. P2412 - Endoscopic Mucosal Resection vs Endoscopic Submucosal Dissection for Non-Pedunculated 20-40 mm Colonic Lesions: An Enhanced Markov Model Accounting for Recurrence, Recovery, and Adverse Events, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
