Monday Poster Session
Category: Biliary/Pancreas
P2376 - Avoiding the Scalpel: Endoscopic and Percutaneous Management of Iatrogenic Common Hepatic Duct Injury
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SN
Samia Nadeem, MD (she/her/hers)
University of Massachusetts Chan Medical School-Baystate Medical Center
Broad Brook, CT
Presenting Author(s)
Samia Nadeem, MD1, Syed Hamza Sohail, MD2, Hamza Khalid, MD3, Nha Duong, DO2
1University of Massachusetts Chan Medical School-Baystate Medical Center, Broad Brook, CT; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3Shifa College of Medicine, Broad Brook, CT
Introduction: Bile duct injury is a rare but serious complication of laparoscopic cholecystectomy, with an estimated 0.3-0.6% of cases. However, these injuries are associated with substantial morbidity and often necessitate hepaticojejunostomy. We present a case in which a multidisciplinary approach combining advanced endoscopic techniques successfully managed an iatrogenic common hepatic duct (CHD) injury, avoiding the need for major surgery.
Case Description/
Methods: A 73-year-old male with right upper quadrant pain was diagnosed with acute cholecystitis from a gallstone at the gallbladder neck. He underwent laparoscopic cholecystectomy, complicated by cystic duct avulsion and bile leak, managed intraoperatively with ERCP and placement of a transpapillary biliary stent and JP drain.
Persistent high-output bilious drainage over the next few days prompted a repeat ERCP, which raised concerns for a bile duct avulsion injury, as the right hepatic duct could not be visualized. The stent was exchanged for a double-pigtail stent, which was placed into the suspected bile leak cavity. A percutaneous transhepatic cholangiogram (PTC) was attempted but failed due to minimally dilated ducts, and biliary access could not be achieved. The patient remained stable and was discharged with a drain in place for outpatient follow-up.
He was readmitted within a month for syncope due to volume loss from high-output biliary drainage. A PTC was attempted again and achieved biliary cannulation, but placement of an internal or external drain was unsuccessful due to interference from the existing transpapillary stent. A subsequent rendezvous procedure was undertaken with IR. The transpapillary stent was removed, and a cholangioscope was advanced through the CHD injury into the right hepatic duct with an IR cholangiogram serving as a guide. The surgical drain was visible at the CHD injury. Using a wire, we were able to place a straight plastic biliary stent into the right hepatic duct with bile flow noted, hence bridging the injured portion of the CHD. The same process was repeated for the left hepatic duct. The percutaneous biliary drain was removed, and the surgical drain was clamped and ultimately removed. A follow-up ERCP showed no bile leak, and the stents were replaced successfully.
Discussion: This case highlights that a multidisciplinary approach combining percutaneous and endoscopic approach may provide a non-surgical alternative for serious bile duct injuries, potentially avoiding highly morbid anatomy-altering procedures.
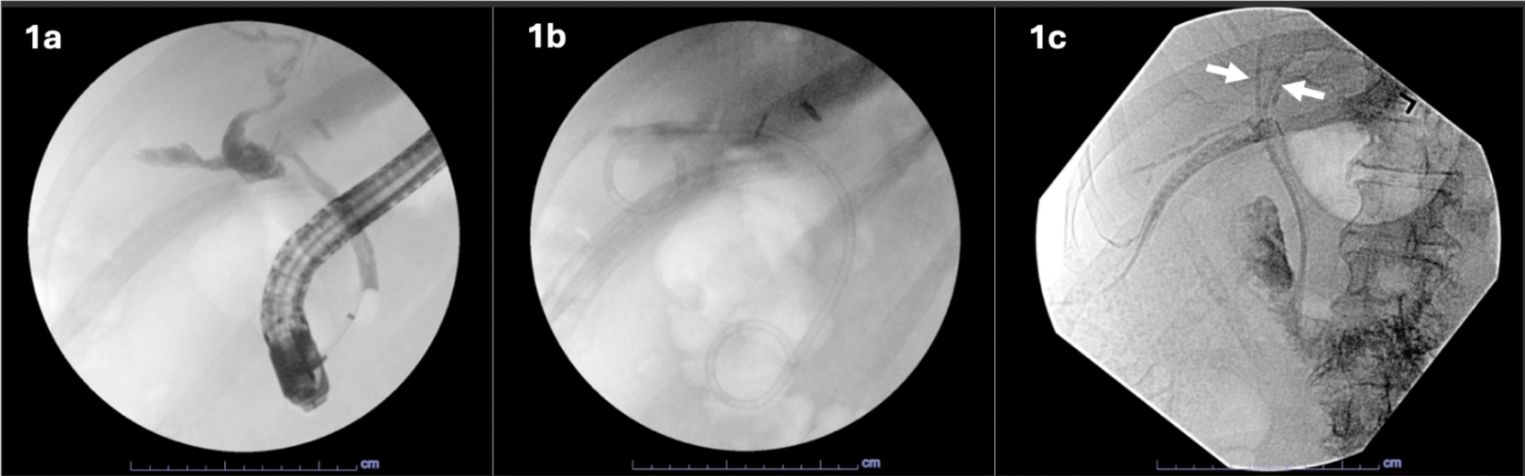
Figure: Figure 1 a) Extensive bile leak from cystic duct avulsion noted on initial ERCP b) A 10Fr x 10 cm double pigtail stent placed into suspected bile leak cavity with distal portion draining transpapillary c) Successful placement of a 7Fr x 12cm plastic biliary stent traversing the CHD injury into the right posterior duct (arrow). Another 7Fr x 12cm plastic biliary stent was successfully placed into the left main hepatic duct, traversing the CHD injury (arrow).
Disclosures:
Samia Nadeem indicated no relevant financial relationships.
Syed Hamza Sohail indicated no relevant financial relationships.
Hamza Khalid indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Samia Nadeem, MD1, Syed Hamza Sohail, MD2, Hamza Khalid, MD3, Nha Duong, DO2. P2376 - Avoiding the Scalpel: Endoscopic and Percutaneous Management of Iatrogenic Common Hepatic Duct Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Massachusetts Chan Medical School-Baystate Medical Center, Broad Brook, CT; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3Shifa College of Medicine, Broad Brook, CT
Introduction: Bile duct injury is a rare but serious complication of laparoscopic cholecystectomy, with an estimated 0.3-0.6% of cases. However, these injuries are associated with substantial morbidity and often necessitate hepaticojejunostomy. We present a case in which a multidisciplinary approach combining advanced endoscopic techniques successfully managed an iatrogenic common hepatic duct (CHD) injury, avoiding the need for major surgery.
Case Description/
Methods: A 73-year-old male with right upper quadrant pain was diagnosed with acute cholecystitis from a gallstone at the gallbladder neck. He underwent laparoscopic cholecystectomy, complicated by cystic duct avulsion and bile leak, managed intraoperatively with ERCP and placement of a transpapillary biliary stent and JP drain.
Persistent high-output bilious drainage over the next few days prompted a repeat ERCP, which raised concerns for a bile duct avulsion injury, as the right hepatic duct could not be visualized. The stent was exchanged for a double-pigtail stent, which was placed into the suspected bile leak cavity. A percutaneous transhepatic cholangiogram (PTC) was attempted but failed due to minimally dilated ducts, and biliary access could not be achieved. The patient remained stable and was discharged with a drain in place for outpatient follow-up.
He was readmitted within a month for syncope due to volume loss from high-output biliary drainage. A PTC was attempted again and achieved biliary cannulation, but placement of an internal or external drain was unsuccessful due to interference from the existing transpapillary stent. A subsequent rendezvous procedure was undertaken with IR. The transpapillary stent was removed, and a cholangioscope was advanced through the CHD injury into the right hepatic duct with an IR cholangiogram serving as a guide. The surgical drain was visible at the CHD injury. Using a wire, we were able to place a straight plastic biliary stent into the right hepatic duct with bile flow noted, hence bridging the injured portion of the CHD. The same process was repeated for the left hepatic duct. The percutaneous biliary drain was removed, and the surgical drain was clamped and ultimately removed. A follow-up ERCP showed no bile leak, and the stents were replaced successfully.
Discussion: This case highlights that a multidisciplinary approach combining percutaneous and endoscopic approach may provide a non-surgical alternative for serious bile duct injuries, potentially avoiding highly morbid anatomy-altering procedures.
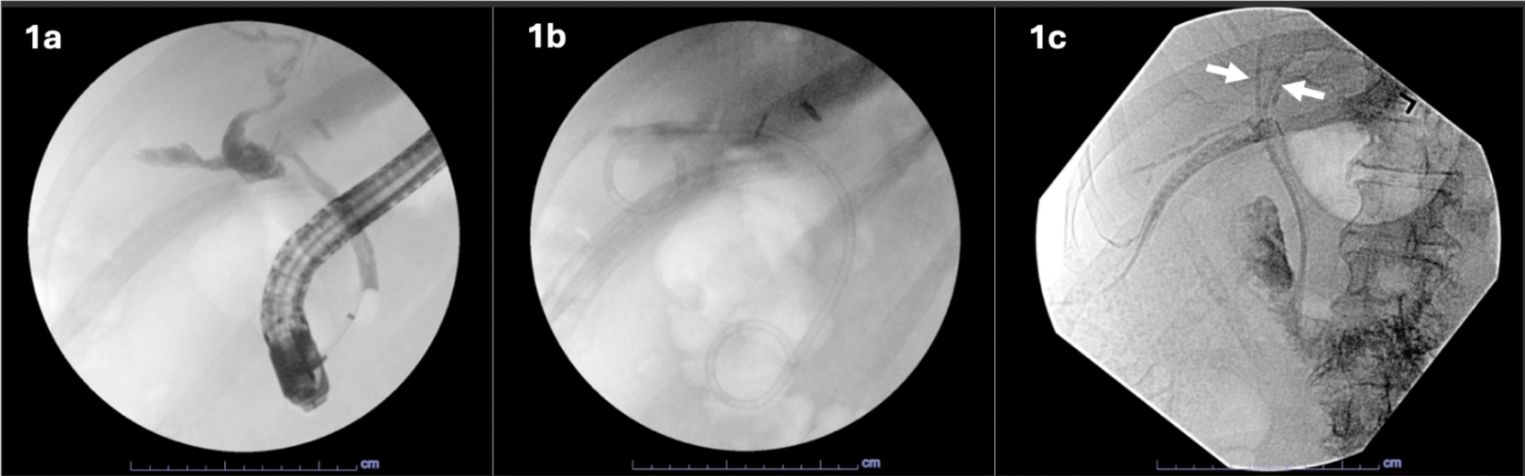
Figure: Figure 1 a) Extensive bile leak from cystic duct avulsion noted on initial ERCP b) A 10Fr x 10 cm double pigtail stent placed into suspected bile leak cavity with distal portion draining transpapillary c) Successful placement of a 7Fr x 12cm plastic biliary stent traversing the CHD injury into the right posterior duct (arrow). Another 7Fr x 12cm plastic biliary stent was successfully placed into the left main hepatic duct, traversing the CHD injury (arrow).
Disclosures:
Samia Nadeem indicated no relevant financial relationships.
Syed Hamza Sohail indicated no relevant financial relationships.
Hamza Khalid indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Samia Nadeem, MD1, Syed Hamza Sohail, MD2, Hamza Khalid, MD3, Nha Duong, DO2. P2376 - Avoiding the Scalpel: Endoscopic and Percutaneous Management of Iatrogenic Common Hepatic Duct Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
