Monday Poster Session
Category: Biliary/Pancreas
P2374 - EUS-Guided Solutions for Tackling Complex Gastric and Biliary Obstructions in Advanced Cancer
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- NR
Navkiran Randhawa, DO
Augusta University
Augusta, GA
Presenting Author(s)
Navi Randhawa, DO1, Sajid Ali, MD2, Amit Hudgi, MD1, Ahamed Khalyfa, DO3, John Erikson Yap, MD, MBA, FACG4, Daniel Castresana, MD1, Viveksandeep Thoguluva Chandrasekar, MBBS5
1Augusta University, Augusta, GA; 2Aiken Regional Medical Centers, Aiken, SC; 3University of Iowa, Iowa City, IA; 4University of Utah Health, Salt Lake City, UT; 5Medical College of Georgia at Augusta University, Augusta, GA
Introduction:
Case Description/
Methods:
Discussion:
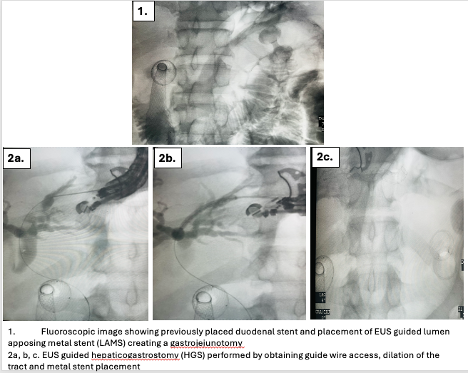
Figure: 1. Fluoroscopic image showing previously placed duodenal stent and placement of EUS guided lument apposing metal stent creating a gastrojejunotomy.
2a,b,c. EUS guided Hepaticogastrostomy performed by obtaining guide wire access, dilation of the tract and metal stent placement.
Disclosures:
Navi Randhawa indicated no relevant financial relationships.
Sajid Ali indicated no relevant financial relationships.
Amit Hudgi indicated no relevant financial relationships.
Ahamed Khalyfa indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Daniel Castresana indicated no relevant financial relationships.
Viveksandeep Thoguluva Chandrasekar indicated no relevant financial relationships.
Navi Randhawa, DO1, Sajid Ali, MD2, Amit Hudgi, MD1, Ahamed Khalyfa, DO3, John Erikson Yap, MD, MBA, FACG4, Daniel Castresana, MD1, Viveksandeep Thoguluva Chandrasekar, MBBS5. P2374 - EUS-Guided Solutions for Tackling Complex Gastric and Biliary Obstructions in Advanced Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Augusta University, Augusta, GA; 2Aiken Regional Medical Centers, Aiken, SC; 3University of Iowa, Iowa City, IA; 4University of Utah Health, Salt Lake City, UT; 5Medical College of Georgia at Augusta University, Augusta, GA
Introduction:
Gastric outlet obstruction (GOO) and biliary obstruction are serious complications encountered in advanced gastric and pancreaticobiliary malignancies. Traditionally management of surgery remains limitedin patients with metastatic disease or poor performance status. Recent advances in endoscopic ultrasound (EUS)-guided techniques, such as gastrojejunostomy (EUS-GJ) and hepaticogastrostomy (EUS-HGS), provide minimally invasive solutions for effective palliation in complex cases. We present a case of metastatic gastric adenocarcinoma requiring sequential EUS-GJ and HGS to address both gastric outlet and biliary obstructions, demonstrating the utility and adaptability of these advanced endoscopic procedures.
Case Description/
Methods:
A 59-year-old male with HTN, HLD, GERD presented with severe abdominal pain, vomiting and significant weight loss of over 30 pounds over 2 months. CT imaging revealed diffuse thickening of the greater curvature, multiple lymph nodes in porta hepatis and duodenal pancreatic groove along with a single enlarged left supraclavicular lymph node. Initial endoscopic evaluation revealed a high-grade, long malignant GOO in the antrum with biopsies revealing adenocarcinoma. EUS with endoscopic and fluoroscopic guidance revealed the stenosis extending into the duodenal bulb. A 22mm x 60mm duodenal stent was successfully deployed across the stricture.
Three days post-procedure, the patient continued to have emesis with per oral intake. A repeat EGD revealed a clogged duodenal stent and CT showed incompletely expanded stent due to tight stricture. EUS-GJ was performed using a lumen apposing metal stent, effectively bypassing the gastric obstruction. Although the patient was able to tolerate diet, he was noted to have rising liver enzymes. Imaging confirmed distal biliary obstruction. A week after GJ, EUS-HGS was successfully performed due to lack of ampullary or duodenal bulb access. Patient is clinically doing well with normalization of LFTs and receiving palliative chemotherapy.
Discussion:
This case illustrates the critical role of advanced EUS-guided interventions in managing multi-level malignant obstruction. EUS-GJ and EUS-HGS provided effective symptom relief and improved gastrointestinal function, enhancing patient’s quality of life. Our experience supports the expanding role of minimally invasive techniques as viable alternatives to traditional surgical methods, highlighting their potential to reshape palliative care for advanced gastrointestinal malignancies.
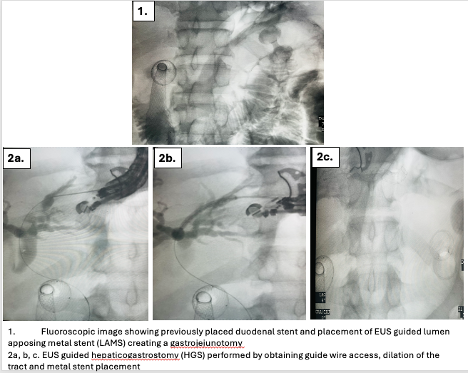
Figure: 1. Fluoroscopic image showing previously placed duodenal stent and placement of EUS guided lument apposing metal stent creating a gastrojejunotomy.
2a,b,c. EUS guided Hepaticogastrostomy performed by obtaining guide wire access, dilation of the tract and metal stent placement.
Disclosures:
Navi Randhawa indicated no relevant financial relationships.
Sajid Ali indicated no relevant financial relationships.
Amit Hudgi indicated no relevant financial relationships.
Ahamed Khalyfa indicated no relevant financial relationships.
John Erikson Yap: Phathom Pharmaceutical – Speakers Bureau. Steris – Consultant.
Daniel Castresana indicated no relevant financial relationships.
Viveksandeep Thoguluva Chandrasekar indicated no relevant financial relationships.
Navi Randhawa, DO1, Sajid Ali, MD2, Amit Hudgi, MD1, Ahamed Khalyfa, DO3, John Erikson Yap, MD, MBA, FACG4, Daniel Castresana, MD1, Viveksandeep Thoguluva Chandrasekar, MBBS5. P2374 - EUS-Guided Solutions for Tackling Complex Gastric and Biliary Obstructions in Advanced Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
