Monday Poster Session
Category: Biliary/Pancreas
P2318 - Pancreaticopleural Fistula Unveiled: An Unusual Respiratory Manifestation of Chronic Pancreatitis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nader Al Souky, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Nader Al Souky, MD1, Mahmoud Mahdi, MD1, Hasan Jaber, MD1, Kevin J. Kadado, DO1, Daly Al-Hadeethi, MD2, William J.. Salyers, MD, MPH3
1University of Kansas School of Medicine, Wichita, KS; 2Wichita-KUMC, Wichita, KS; 3University of Kansas School of Medicine - Wichita, Wichita, KS
Introduction: Pancreaticopleural fistula (PPF) is a rare complication of pancreatitis, resulting from pancreatic duct disruption and leading to massive, recurrent pleural effusions. Due to its atypical presentation, diagnosis is often delayed. Prompt recognition through imaging and pleural fluid analysis is essential to guide effective medical, endoscopic, or surgical management.
Case Description/
Methods: A 32-year-old male with chronic pancreatitis due to alcohol use, hepatic steatosis, and gastritis presented with shortness of breath and was found to have a large right-sided pleural effusion. He was hypotensive on admission, with mildly elevated liver enzymes and lipase (496 U/L). A CT scan of the abdomen and pelvis revealed peripancreatic inflammation. Thoracentesis drained 6 liters of fluid, and a right-sided pigtail catheter was placed. Despite initial management, pleural output remained high (600 mL/day), and serial chest X-rays showed reaccumulation of effusion, prompting second thoracentesis and placement of an additional drain. Fluid analysis revealed markedly elevated amylase ( >3200 U/L) and lipase ( >1200 U/L), raising suspicion for PPF. Gastroenterology consultation was obtained and MRCP confirmed a fistulous connection between the pancreatic duct and right pleural cavity (Figures 1 and 2). The patient was made NPO, started on octreotide, and received nutritional support via TPN, later transitioned to orogastric feeding. Chest tube output gradually decreased, allowing removal within seven days. Follow-up serial chest X-rays confirmed resolution of the effusion.
Discussion: PPF is a rare complication of pancreatitis, resulting in recurrent, enzyme-rich effusions. Unlike classic pancreatitis symptoms, its atypical respiratory presentation, including dyspnea, cough, and chest pain, often delays diagnosis. Recognition hinges on markedly elevated pleural fluid amylase (typically > 1000 U/L), and confirmation via MRCP. Initial management includes bowel rest, octreotide to suppress pancreatic secretions, and nutritional support. If conservative management fails, endoscopic therapy with ERCP and pancreatic duct stenting may promote fistula closure. Refractory cases may require surgical intervention to correct underlying ductal pathology and achieve definitive closure. Early diagnosis and targeted treatment are critical to avoid prolonged hospitalization and morbidity. This case highlights the importance of considering PPF in patients with pancreatitis presenting with unexplained pleural effusions.
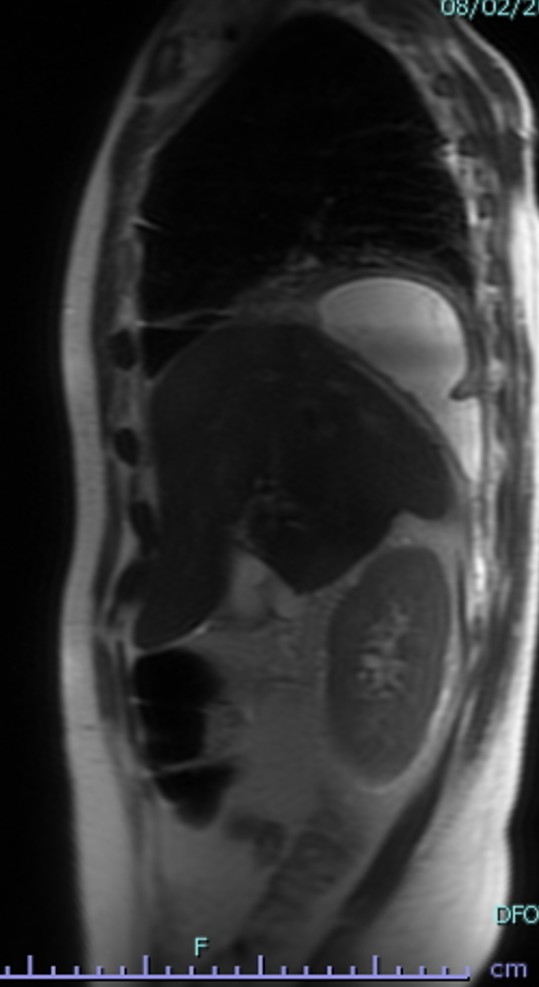
Figure: Figure 1: MRCP with pancreatic protocol that reveals a fistula track extending from the pancreatic cyst to the lower lobes of the right lung where the pleural effusion collects (blue start).
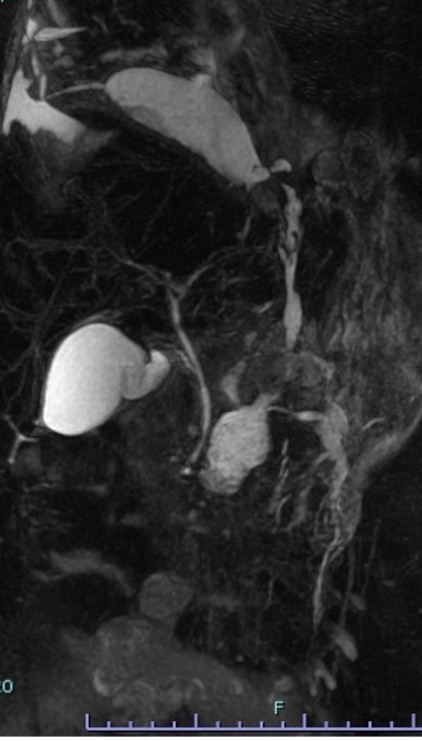
Figure: Figure 2: A sagittal MRI cut showing the fistulous tract (blue arrows) that connects the cysts from the pancreas to the pleural effusion pocket (blue star).
Disclosures:
Nader Al Souky indicated no relevant financial relationships.
Mahmoud Mahdi indicated no relevant financial relationships.
Hasan Jaber indicated no relevant financial relationships.
Kevin Kadado indicated no relevant financial relationships.
Daly Al-Hadeethi indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
Nader Al Souky, MD1, Mahmoud Mahdi, MD1, Hasan Jaber, MD1, Kevin J. Kadado, DO1, Daly Al-Hadeethi, MD2, William J.. Salyers, MD, MPH3. P2318 - Pancreaticopleural Fistula Unveiled: An Unusual Respiratory Manifestation of Chronic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2Wichita-KUMC, Wichita, KS; 3University of Kansas School of Medicine - Wichita, Wichita, KS
Introduction: Pancreaticopleural fistula (PPF) is a rare complication of pancreatitis, resulting from pancreatic duct disruption and leading to massive, recurrent pleural effusions. Due to its atypical presentation, diagnosis is often delayed. Prompt recognition through imaging and pleural fluid analysis is essential to guide effective medical, endoscopic, or surgical management.
Case Description/
Methods: A 32-year-old male with chronic pancreatitis due to alcohol use, hepatic steatosis, and gastritis presented with shortness of breath and was found to have a large right-sided pleural effusion. He was hypotensive on admission, with mildly elevated liver enzymes and lipase (496 U/L). A CT scan of the abdomen and pelvis revealed peripancreatic inflammation. Thoracentesis drained 6 liters of fluid, and a right-sided pigtail catheter was placed. Despite initial management, pleural output remained high (600 mL/day), and serial chest X-rays showed reaccumulation of effusion, prompting second thoracentesis and placement of an additional drain. Fluid analysis revealed markedly elevated amylase ( >3200 U/L) and lipase ( >1200 U/L), raising suspicion for PPF. Gastroenterology consultation was obtained and MRCP confirmed a fistulous connection between the pancreatic duct and right pleural cavity (Figures 1 and 2). The patient was made NPO, started on octreotide, and received nutritional support via TPN, later transitioned to orogastric feeding. Chest tube output gradually decreased, allowing removal within seven days. Follow-up serial chest X-rays confirmed resolution of the effusion.
Discussion: PPF is a rare complication of pancreatitis, resulting in recurrent, enzyme-rich effusions. Unlike classic pancreatitis symptoms, its atypical respiratory presentation, including dyspnea, cough, and chest pain, often delays diagnosis. Recognition hinges on markedly elevated pleural fluid amylase (typically > 1000 U/L), and confirmation via MRCP. Initial management includes bowel rest, octreotide to suppress pancreatic secretions, and nutritional support. If conservative management fails, endoscopic therapy with ERCP and pancreatic duct stenting may promote fistula closure. Refractory cases may require surgical intervention to correct underlying ductal pathology and achieve definitive closure. Early diagnosis and targeted treatment are critical to avoid prolonged hospitalization and morbidity. This case highlights the importance of considering PPF in patients with pancreatitis presenting with unexplained pleural effusions.
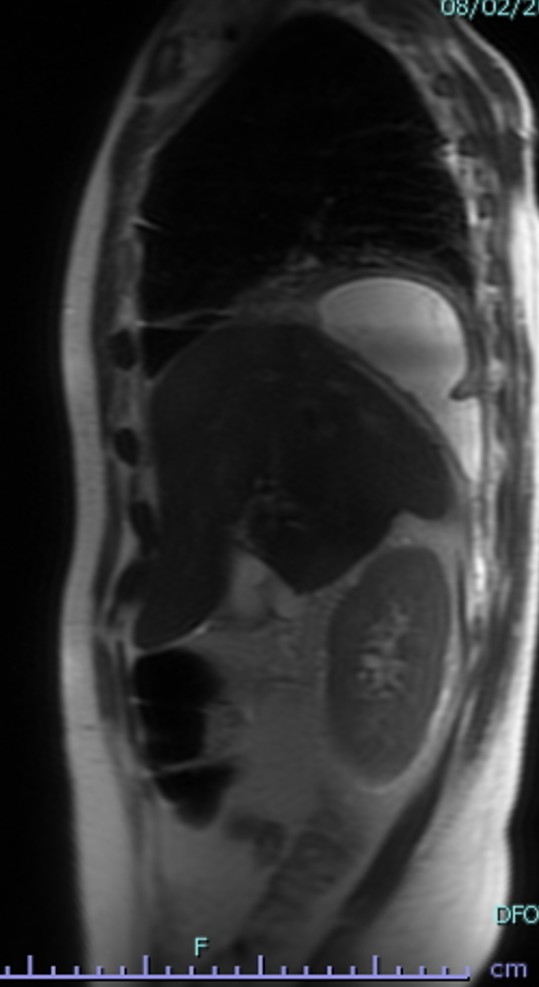
Figure: Figure 1: MRCP with pancreatic protocol that reveals a fistula track extending from the pancreatic cyst to the lower lobes of the right lung where the pleural effusion collects (blue start).
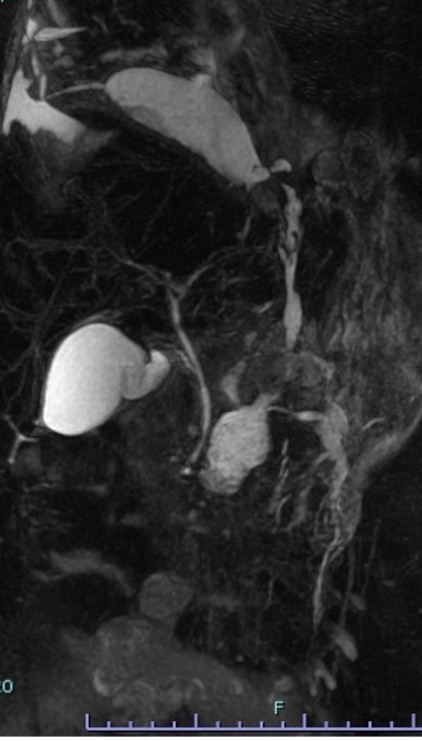
Figure: Figure 2: A sagittal MRI cut showing the fistulous tract (blue arrows) that connects the cysts from the pancreas to the pleural effusion pocket (blue star).
Disclosures:
Nader Al Souky indicated no relevant financial relationships.
Mahmoud Mahdi indicated no relevant financial relationships.
Hasan Jaber indicated no relevant financial relationships.
Kevin Kadado indicated no relevant financial relationships.
Daly Al-Hadeethi indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
Nader Al Souky, MD1, Mahmoud Mahdi, MD1, Hasan Jaber, MD1, Kevin J. Kadado, DO1, Daly Al-Hadeethi, MD2, William J.. Salyers, MD, MPH3. P2318 - Pancreaticopleural Fistula Unveiled: An Unusual Respiratory Manifestation of Chronic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
