Monday Poster Session
Category: Biliary/Pancreas
P2313 - Intrahepatic Biliary Ductal Dilatation Secondary to High-Grade Small Bowel Obstruction
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Naveena Chittineedi, MD
Northwell Health
Manhasset, NY
Presenting Author(s)
Naveena Chittineedi, MD, Jang Kim, MD, Bryan Taylor, MD, Alvin Htut, MD
Northwell Health, Manhasset, NY
Introduction: Intrahepatic biliary ductal dilatation is most commonly associated with intrinsic biliary pathology such as choledocholithiasis, strictures, or malignancy. However, extrinsic factors, particularly mechanical obstruction caused by postoperative anatomy can also produce significant biliary abnormalities. In this case, we describe a rare presentation of mild-to-moderate intrahepatic biliary ductal dilatation secondary to a high-grade small bowel obstruction (SBO) at the site of a prior hepaticojejunal anastomosis. Recognition of this etiology is essential to avoid unnecessary invasive biliary interventions.
Case Description/
Methods: We present a 67-year-old male with a complex hepatopancreatobiliary history including autoimmune pancreatitis, autoimmune hepatitis, prior cholecystectomy, prior partial pancreatoduodenectomy and a hepaticojejunostomy who presented with nausea, vomiting, and diffuse abdominal pain. Initial labs showed leukocytosis and a cholestatic liver injury pattern, however infectious work-up was negative. CT imaging revealed a high-grade SBO involving the jejunal limb of the hepaticojejunostomy. MRCP demonstrated worsening intrahepatic biliary dilatation without intrinsic biliary obstruction. Despite initial conservative management of the SBO, his clinical status worsened, prompting robot-assisted laparoscopic lysis of adhesions. Postoperatively, his symptoms and liver function tests improved.
Discussion: This case illustrates how post-surgical biliary anatomy, particularly in patients with a hepaticojejunostomy, can become susceptible to rare but significant complications such as kinking of the anastomosis causing a high-grade SBO and leading to intrahepatic biliary dilation and cholestatic liver injury pattern. The resolution of both symptoms and elevated liver function tests following lysis of adhesions supports the diagnosis of SBO-induced biliary obstruction. Recognizing this uncommon etiology is essential, as misattribution to intrinsic biliary disease may lead to unnecessary and invasive interventions such as ERCP or stent placement. In conclusion, this case highlights the importance of correlating imaging findings with surgical anatomy and adds to the limited literature on SBO-induced cholestatic liver injury. Awareness of this phenomenon can guide clinicians toward timely surgical management and help avoid delays or mismanagement in similar clinical scenarios.
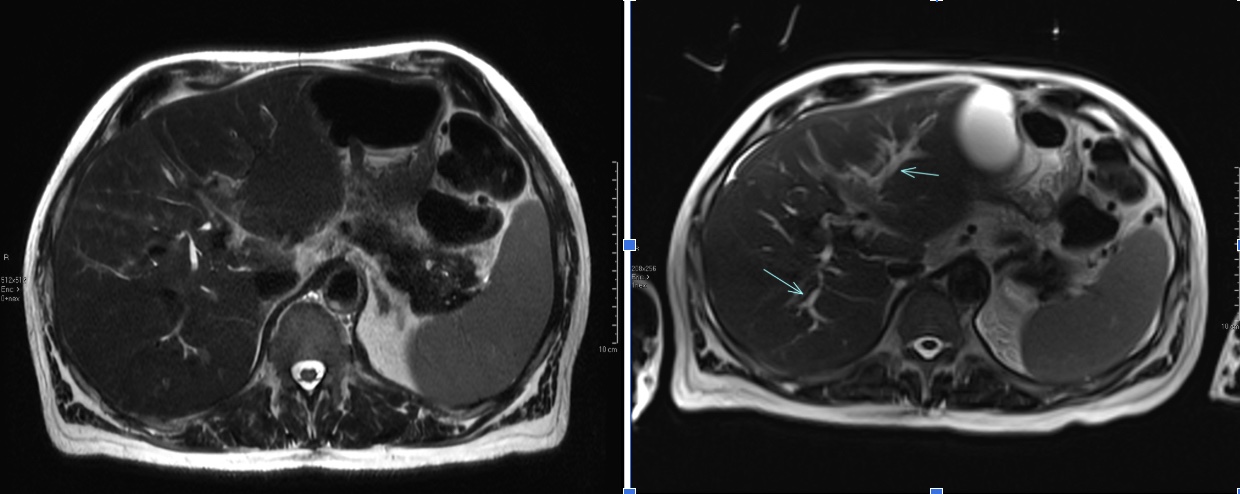
Figure: MR Abdomen Axial Cut: Baseline (Left) and SBO with Intrahepatic Ductal Dilatation (Right)

Figure: MR Abdomen Coronal Cut: Baseline (Left) and SBO with Intrahepatic Ductal Dilatation (Right)
Disclosures:
Naveena Chittineedi indicated no relevant financial relationships.
Jang Kim indicated no relevant financial relationships.
Bryan Taylor indicated no relevant financial relationships.
Alvin Htut indicated no relevant financial relationships.
Naveena Chittineedi, MD, Jang Kim, MD, Bryan Taylor, MD, Alvin Htut, MD. P2313 - Intrahepatic Biliary Ductal Dilatation Secondary to High-Grade Small Bowel Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Northwell Health, Manhasset, NY
Introduction: Intrahepatic biliary ductal dilatation is most commonly associated with intrinsic biliary pathology such as choledocholithiasis, strictures, or malignancy. However, extrinsic factors, particularly mechanical obstruction caused by postoperative anatomy can also produce significant biliary abnormalities. In this case, we describe a rare presentation of mild-to-moderate intrahepatic biliary ductal dilatation secondary to a high-grade small bowel obstruction (SBO) at the site of a prior hepaticojejunal anastomosis. Recognition of this etiology is essential to avoid unnecessary invasive biliary interventions.
Case Description/
Methods: We present a 67-year-old male with a complex hepatopancreatobiliary history including autoimmune pancreatitis, autoimmune hepatitis, prior cholecystectomy, prior partial pancreatoduodenectomy and a hepaticojejunostomy who presented with nausea, vomiting, and diffuse abdominal pain. Initial labs showed leukocytosis and a cholestatic liver injury pattern, however infectious work-up was negative. CT imaging revealed a high-grade SBO involving the jejunal limb of the hepaticojejunostomy. MRCP demonstrated worsening intrahepatic biliary dilatation without intrinsic biliary obstruction. Despite initial conservative management of the SBO, his clinical status worsened, prompting robot-assisted laparoscopic lysis of adhesions. Postoperatively, his symptoms and liver function tests improved.
Discussion: This case illustrates how post-surgical biliary anatomy, particularly in patients with a hepaticojejunostomy, can become susceptible to rare but significant complications such as kinking of the anastomosis causing a high-grade SBO and leading to intrahepatic biliary dilation and cholestatic liver injury pattern. The resolution of both symptoms and elevated liver function tests following lysis of adhesions supports the diagnosis of SBO-induced biliary obstruction. Recognizing this uncommon etiology is essential, as misattribution to intrinsic biliary disease may lead to unnecessary and invasive interventions such as ERCP or stent placement. In conclusion, this case highlights the importance of correlating imaging findings with surgical anatomy and adds to the limited literature on SBO-induced cholestatic liver injury. Awareness of this phenomenon can guide clinicians toward timely surgical management and help avoid delays or mismanagement in similar clinical scenarios.
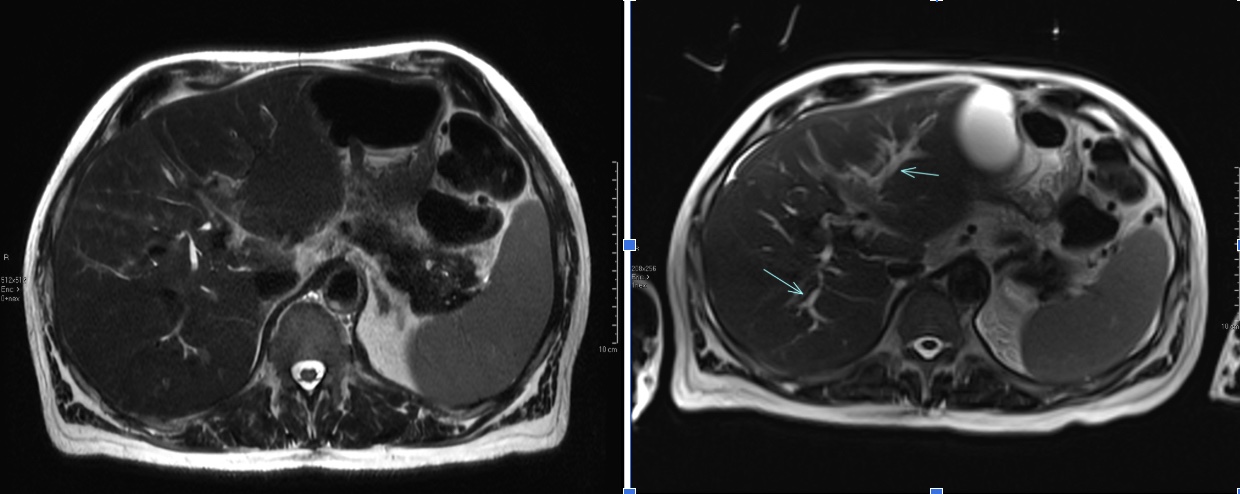
Figure: MR Abdomen Axial Cut: Baseline (Left) and SBO with Intrahepatic Ductal Dilatation (Right)

Figure: MR Abdomen Coronal Cut: Baseline (Left) and SBO with Intrahepatic Ductal Dilatation (Right)
Disclosures:
Naveena Chittineedi indicated no relevant financial relationships.
Jang Kim indicated no relevant financial relationships.
Bryan Taylor indicated no relevant financial relationships.
Alvin Htut indicated no relevant financial relationships.
Naveena Chittineedi, MD, Jang Kim, MD, Bryan Taylor, MD, Alvin Htut, MD. P2313 - Intrahepatic Biliary Ductal Dilatation Secondary to High-Grade Small Bowel Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
