Monday Poster Session
Category: Biliary/Pancreas
P2312 - Myxedema Coma-Induced Severe Acute Pancreatitis: The Thyroid-Pancreas Connection
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yazan Abboud, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Rita Kamoua, BA1, Mahinaz Mohsen, MD2, Olga Sarah, MD2, Yazan Abboud, MD2
1Wright State University Boonshoft School of Medicine, Dayton, OH; 2Rutgers New Jersey Medical School, Newark, NJ
Introduction: Acute pancreatitis (AP) most common risk factors include gallstones, alcohol, and hypertriglyceridemia. While hypothyroidism can elevate serum cholesterol and triglycerides and may precipitate AP through this mechanism, the development of AP in the context of uncontrolled hypothyroidism with a normal lipid panel does not have a clear mechanism. We present a rare case of severe AP in a patient with myxedema coma, occurring in the absence of hyperlipidemia or other identifiable risk factors for AP.
Case Description/
Methods: A 76-year-old female with a history of remote hemodialysis, with no current medical care, was found unresponsive at home. In the ED, she was hypothermic (79.7°F), hypotensive (BP 53/36 mmHg), and bradycardic (HR 49 bpm). Labs showed severe hypothyroidism, metabolic acidosis, AKI, and elevated lipase (Table 1). She was intubated and admitted to the ICU for myxedema coma and suspected AP. Vasopressors, IV fluids, stress dose steroids, high-dose IV levothyroxine, and empiric antibiotics were started. CT Abdomen/Pelvis revealed peripancreatic stranding consistent with AP and multifocal pneumonia (Figure 1). RUQ ultrasound showed gallbladder wall edema, though cholecystitis was deemed unlikely per general surgery and gastroenterology evaluation. Total cholesterol and triglyceride levels were within normal limits, thyroid peroxidase antibodies were elevated, and autoimmune workup was otherwise negative (Table 1). Patient had no history of smoking or alcohol use. Cultures grew Enterobacter, Klebsiella, and MSSA. Liothyronine was added to her regimen with gradual improvement in thyroid function. By hospital day 9, she was off vasopressors, electrolytes stabilized, and kidney function improved. She was extubated and returned to baseline mental status and denied any abdominal pain. She was discharged to a rehabilitation facility.
Discussion: To our knowledge, this is the first case of AP occurring in the setting of myxedema coma with normal serum lipid levels. No well-established mechanisms currently explain how uncontrolled hypothyroidism could precipitate AP in the absence of hyperlipidemia. However, based on findings from animal studies, severe hypothyroidism in our patient may have triggered local metabolic disturbances in the pancreas, leading to intracellular cholesterol and triglyceride accumulation despite a normal serum lipid profile, contributing to the development of AP. Future studies are warranted to elucidate the mechanism of myxedema coma-induced AP.
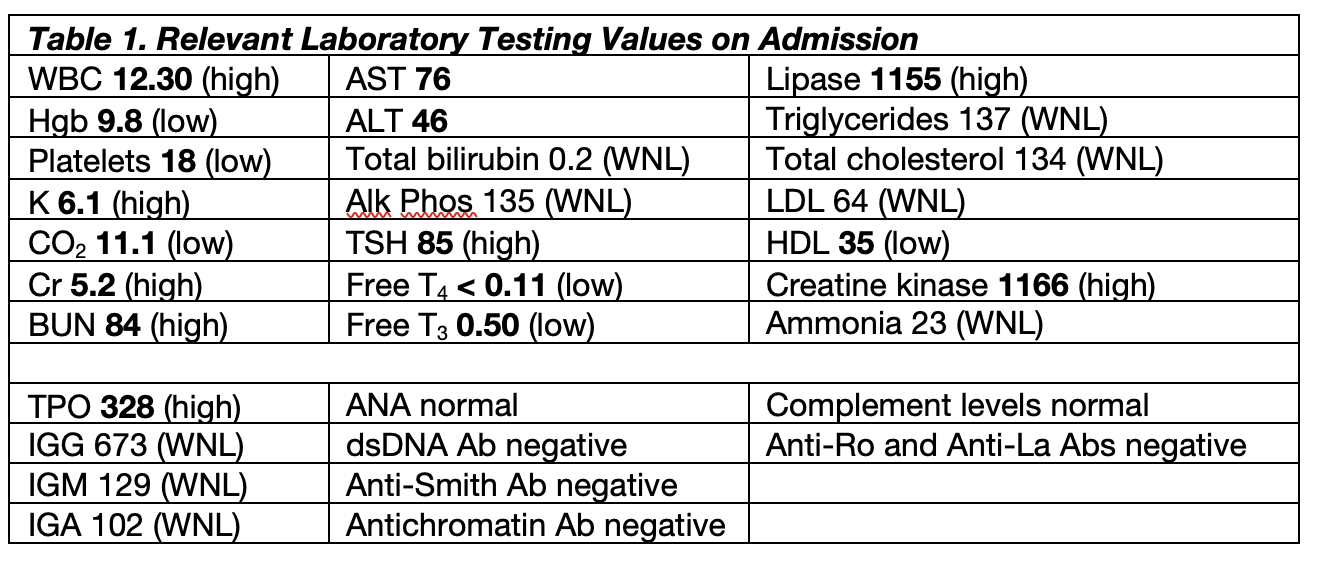
Figure: Table 1: Relevant Laboratory Testing Values on Admission
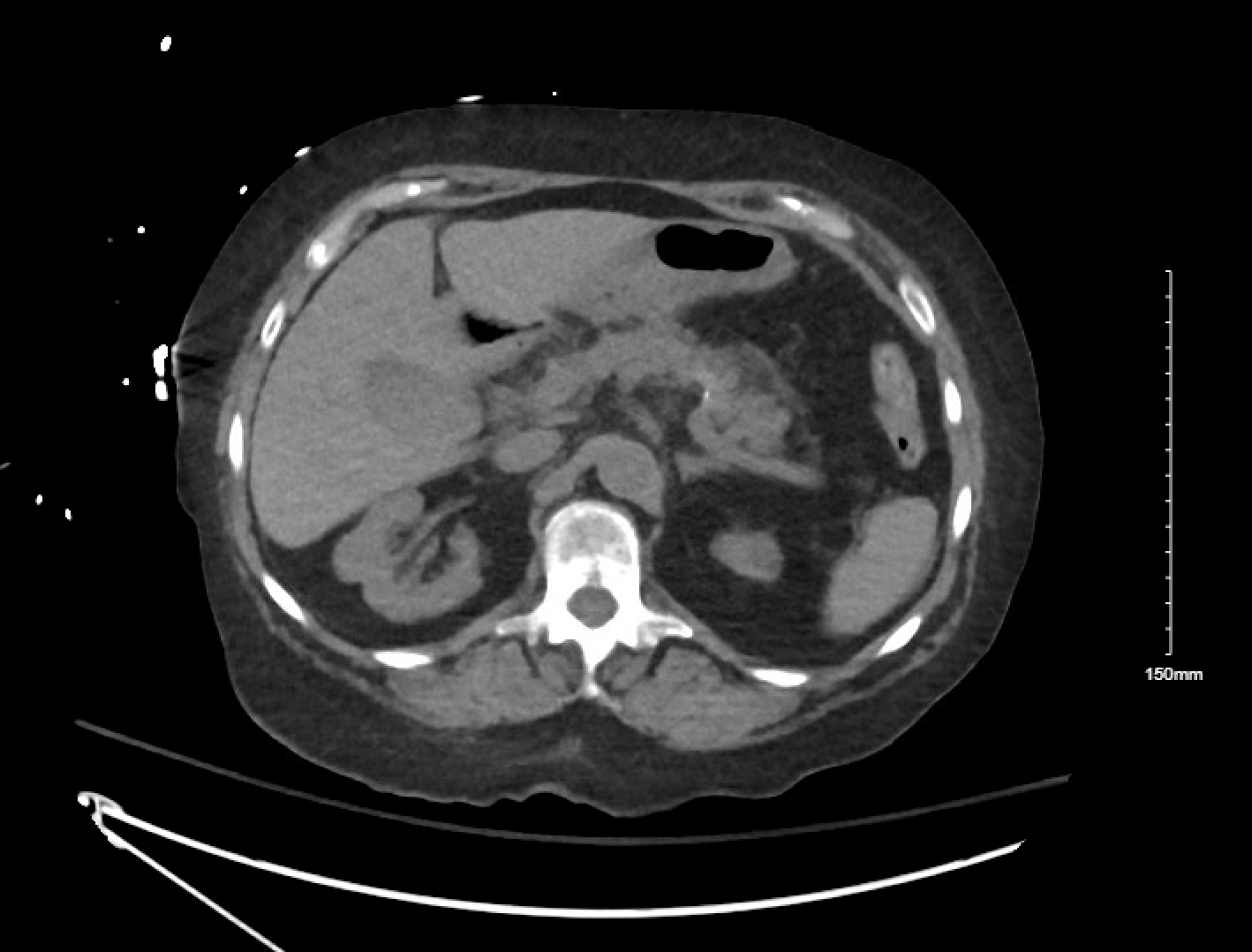
Figure: Figure 1: Computed Tomography Imaging of the Abdomen and Pelvis showing mild peripancreatic stranding at the distal body/tail suggestive of acute pancreatitis, moderate right and small left pleural effusion, and moderate bilateral lower lobes and moderate right upper lobe consolidations with air bronchograms compatible with infiltrate/pneumonia.
Disclosures:
Rita Kamoua indicated no relevant financial relationships.
Mahinaz Mohsen indicated no relevant financial relationships.
Olga Sarah indicated no relevant financial relationships.
Yazan Abboud indicated no relevant financial relationships.
Rita Kamoua, BA1, Mahinaz Mohsen, MD2, Olga Sarah, MD2, Yazan Abboud, MD2. P2312 - Myxedema Coma-Induced Severe Acute Pancreatitis: The Thyroid-Pancreas Connection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wright State University Boonshoft School of Medicine, Dayton, OH; 2Rutgers New Jersey Medical School, Newark, NJ
Introduction: Acute pancreatitis (AP) most common risk factors include gallstones, alcohol, and hypertriglyceridemia. While hypothyroidism can elevate serum cholesterol and triglycerides and may precipitate AP through this mechanism, the development of AP in the context of uncontrolled hypothyroidism with a normal lipid panel does not have a clear mechanism. We present a rare case of severe AP in a patient with myxedema coma, occurring in the absence of hyperlipidemia or other identifiable risk factors for AP.
Case Description/
Methods: A 76-year-old female with a history of remote hemodialysis, with no current medical care, was found unresponsive at home. In the ED, she was hypothermic (79.7°F), hypotensive (BP 53/36 mmHg), and bradycardic (HR 49 bpm). Labs showed severe hypothyroidism, metabolic acidosis, AKI, and elevated lipase (Table 1). She was intubated and admitted to the ICU for myxedema coma and suspected AP. Vasopressors, IV fluids, stress dose steroids, high-dose IV levothyroxine, and empiric antibiotics were started. CT Abdomen/Pelvis revealed peripancreatic stranding consistent with AP and multifocal pneumonia (Figure 1). RUQ ultrasound showed gallbladder wall edema, though cholecystitis was deemed unlikely per general surgery and gastroenterology evaluation. Total cholesterol and triglyceride levels were within normal limits, thyroid peroxidase antibodies were elevated, and autoimmune workup was otherwise negative (Table 1). Patient had no history of smoking or alcohol use. Cultures grew Enterobacter, Klebsiella, and MSSA. Liothyronine was added to her regimen with gradual improvement in thyroid function. By hospital day 9, she was off vasopressors, electrolytes stabilized, and kidney function improved. She was extubated and returned to baseline mental status and denied any abdominal pain. She was discharged to a rehabilitation facility.
Discussion: To our knowledge, this is the first case of AP occurring in the setting of myxedema coma with normal serum lipid levels. No well-established mechanisms currently explain how uncontrolled hypothyroidism could precipitate AP in the absence of hyperlipidemia. However, based on findings from animal studies, severe hypothyroidism in our patient may have triggered local metabolic disturbances in the pancreas, leading to intracellular cholesterol and triglyceride accumulation despite a normal serum lipid profile, contributing to the development of AP. Future studies are warranted to elucidate the mechanism of myxedema coma-induced AP.
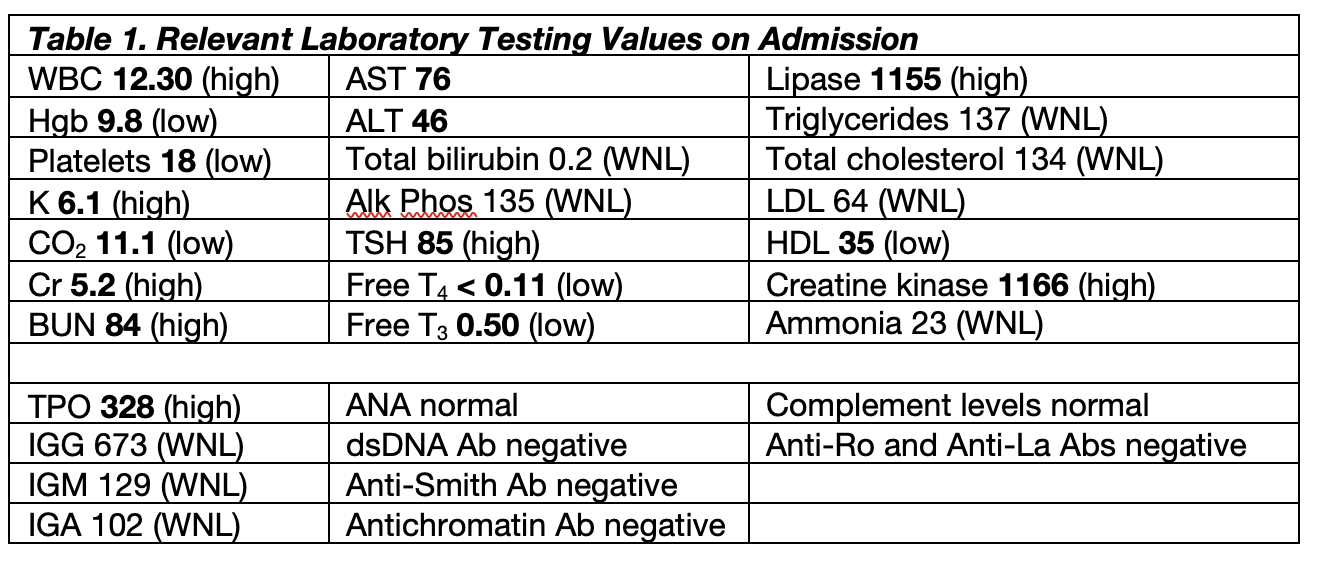
Figure: Table 1: Relevant Laboratory Testing Values on Admission
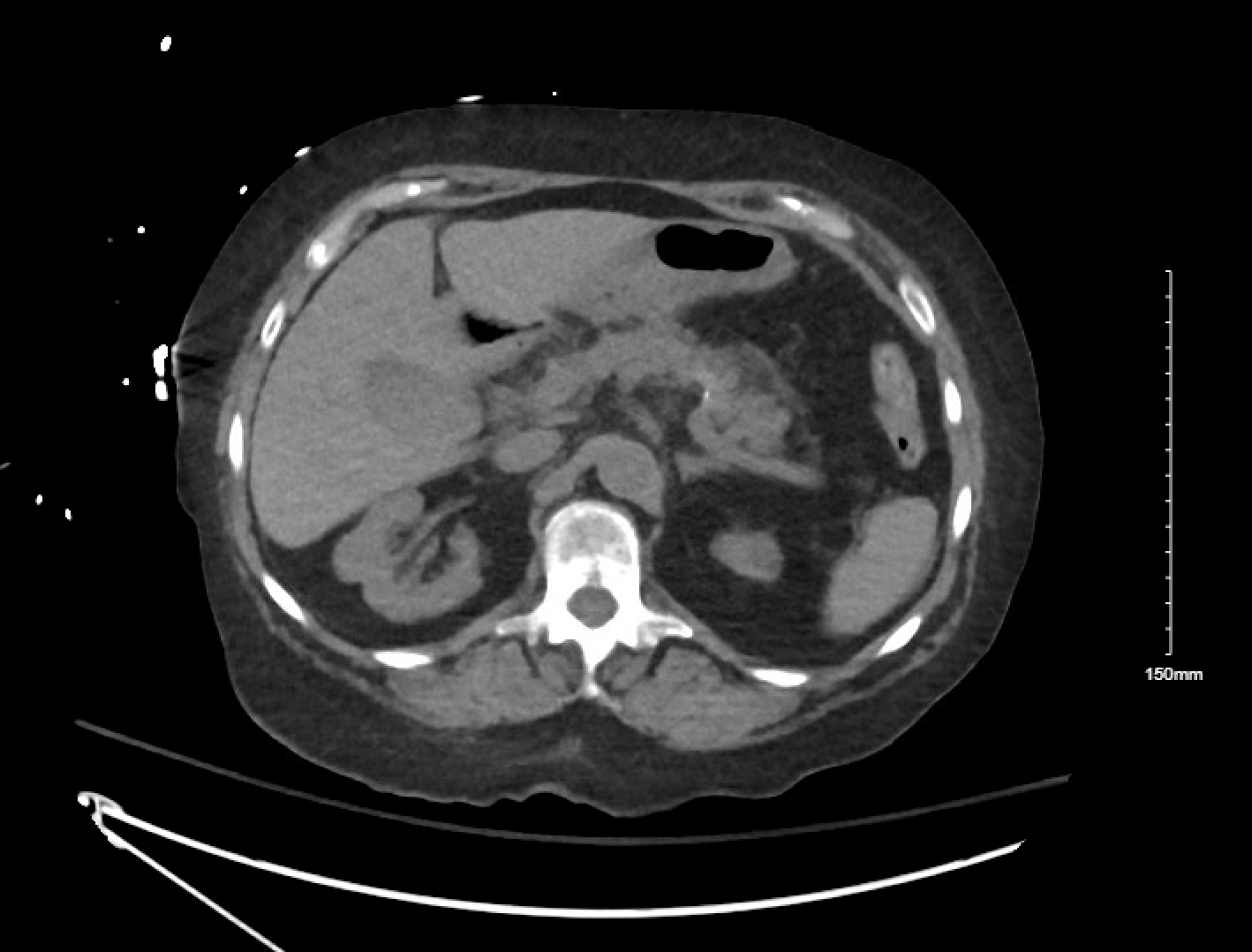
Figure: Figure 1: Computed Tomography Imaging of the Abdomen and Pelvis showing mild peripancreatic stranding at the distal body/tail suggestive of acute pancreatitis, moderate right and small left pleural effusion, and moderate bilateral lower lobes and moderate right upper lobe consolidations with air bronchograms compatible with infiltrate/pneumonia.
Disclosures:
Rita Kamoua indicated no relevant financial relationships.
Mahinaz Mohsen indicated no relevant financial relationships.
Olga Sarah indicated no relevant financial relationships.
Yazan Abboud indicated no relevant financial relationships.
Rita Kamoua, BA1, Mahinaz Mohsen, MD2, Olga Sarah, MD2, Yazan Abboud, MD2. P2312 - Myxedema Coma-Induced Severe Acute Pancreatitis: The Thyroid-Pancreas Connection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
