Monday Poster Session
Category: Biliary/Pancreas
P2311 - Extramedullary Plasmacytoma Masquerading as a Pancreatic and Duodenal Mass: A Rare Case
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SO
Somtochukwu Onwuzo, MD
Allegheny Center for Digestive Health
Pittsburgh, PA
Presenting Author(s)
Somtochukwu Onwuzo, MD1, Chidera Onwuzo, MBBS2, Rashid Abdel-Razeq, MD3, Kojo-Frimpong B. Awuah, MD4, Antoine Boustany, MD5, Abhijit Kulkarni, MD6
1Allegheny Center for Digestive Health, Pittsburgh, PA; 2SUNY Upstate Medical University Hospital, Syracuse, NY; 3Cleveland Clinic Foundation, Cleveland, OH; 4Allegheny Health Network, Pittsburgh, PA; 5University of Florida College of Medicine, Jacksonville, FL; 6Allegheny General Hospital, Pittsburgh, PA
Introduction: Plasmacytomas are rare plasma cell neoplasms with monoclonal proliferation outside the bone marrow. They are classified as solitary bone plasmacytomas (SBP) or extramedullary plasmacytomas (EMP), the latter comprising < 5% of plasma cell malignancies. EMPs may arise de novo or alongside systemic multiple myeloma, often signaling aggressive disease. While most affect the head, neck, or lungs, gastrointestinal (GI) involvement is rare and can mimic adenocarcinoma, lymphoma, or neuroendocrine tumors. We present a patient with multiple myeloma and progression to EMPs involving the pancreas and duodenum.
Case Description/
Methods: A 63-year-old male with immunoglobulin A (IgA) lambda light chain MM presented with several weeks of worsening lethargy. He was diagnosed three years prior, with bone marrow biopsy showing 23% clonal plasma cells expressing CD138 and lambda light chain restriction. Cytogenetics revealed immunoglobulin heavy chain (IGH) fusion, fibroblast growth factor receptor 2 (FGFR2) loss (chromosome 4), and tumor protein 53 (TP53) deletion (chromosome 17). He initially received bortezomib-based therapy, followed by four cycles of daratumumab, lenalidomide, bortezomib, and dexamethasone (DRVD), then underwent autologous stem cell transplant with daratumumab maintenance. Six months later, PET showed new lytic lesions, prompting initiation of daratumumab, pomalidomide, and dexamethasone (DPd). On admission, labs included: WBC 5.3, hemoglobin 12.6, platelets 366, ALT 124, ALP 139, bilirubin 1.3. CT revealed bilateral lung nodules and a 4.7 cm pancreatic head mass abutting the superior mesenteric vessels. Brain MRI showed calvarial enhancement. EUS demonstrated a 3.7 cm irregular pancreatic mass; EGD revealed duodenal nodules. Biopsies from both confirmed EMP with CD138-positive, lambda light chain–restricted plasma cells. He was started on bortezomib, dexamethasone, cisplatin, doxorubicin, cyclophosphamide, and etoposide (VD-PACE).
Discussion: GI EMPs are rare and often misdiagnosed due to nonspecific symptoms and imaging overlap with adenocarcinomas. Mechanisms include hematogenous spread or direct extension; loss of CD56 may facilitate dissemination. TP53 deletion correlates with poor prognosis. Diagnosis relies on biopsy and immunohistochemistry. Treatment is typically systemic, though localized EMPs may benefit from radiation. This case highlights the importance of considering GI EMPs in MM patients presenting with new GI symptoms.
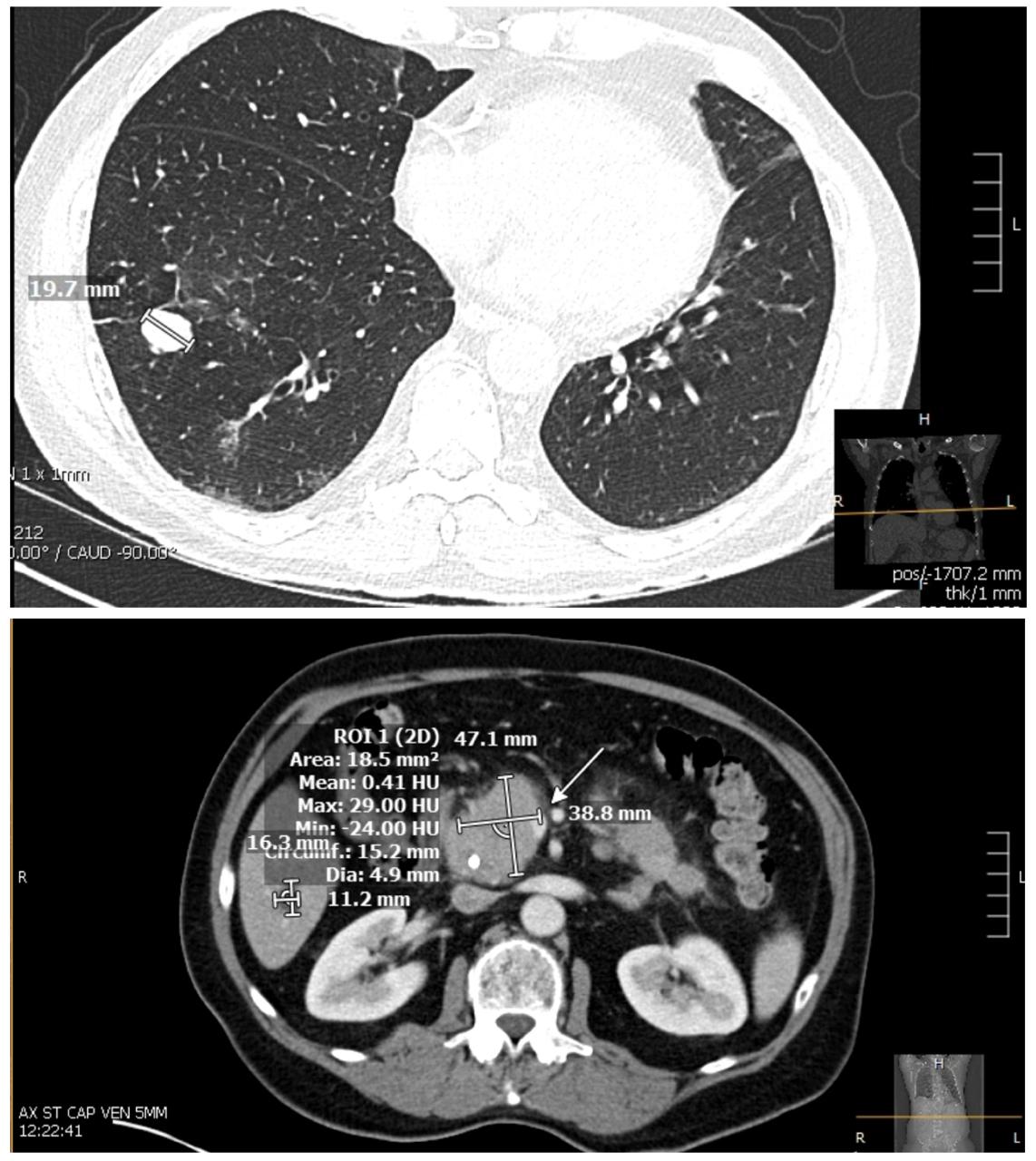
Figure: Image 1: CT chest showing pulmonary nodule and multifocal mass like thickening of the pancreas most notably in the pancreatic head.
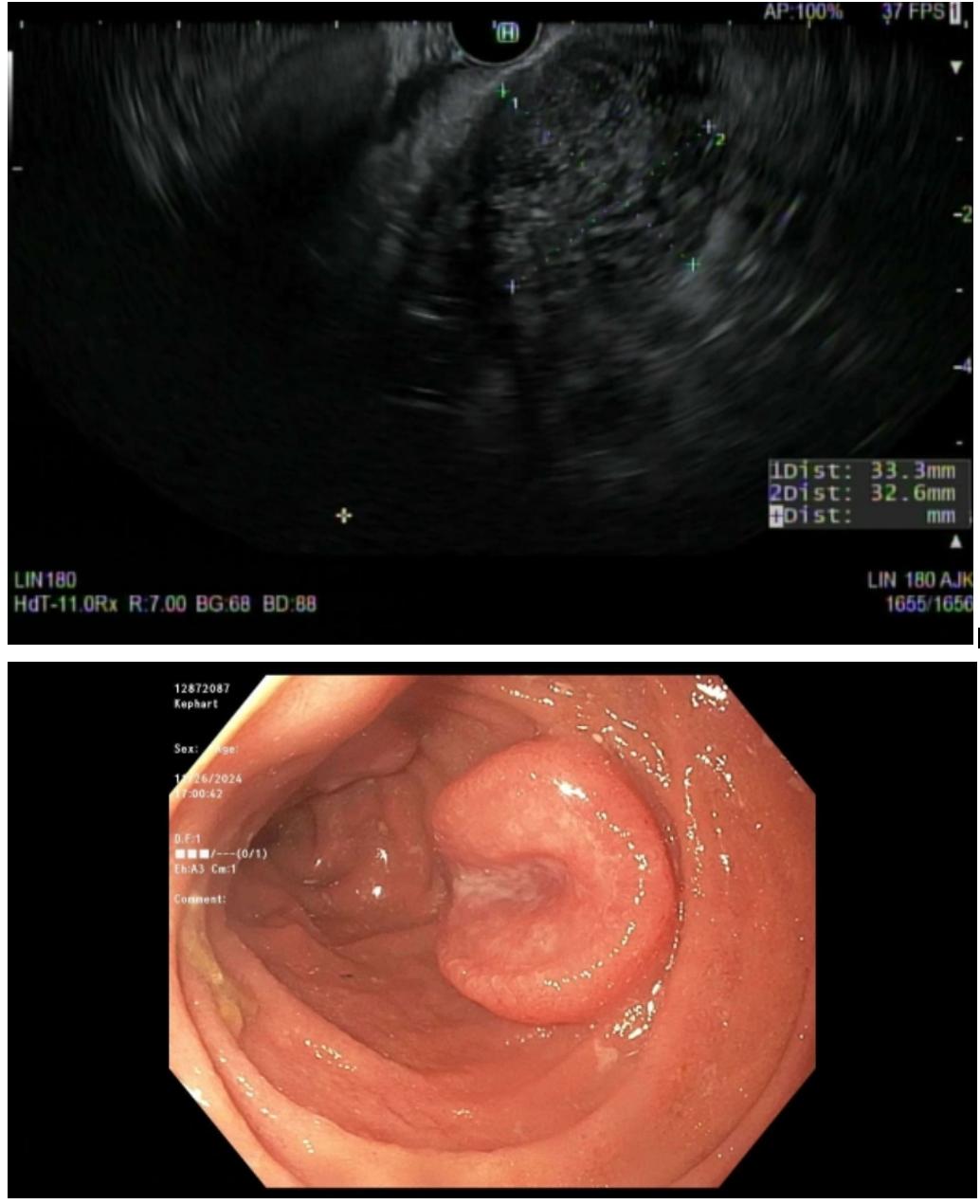
Figure: Image 2: Endoscopic ultrasound showing abnormal pancreatic parenchyma along the head & Duodenal nodule seen on Esophagogastroduodenoscopy
Disclosures:
Somtochukwu Onwuzo indicated no relevant financial relationships.
Chidera Onwuzo indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Abhijit Kulkarni indicated no relevant financial relationships.
Somtochukwu Onwuzo, MD1, Chidera Onwuzo, MBBS2, Rashid Abdel-Razeq, MD3, Kojo-Frimpong B. Awuah, MD4, Antoine Boustany, MD5, Abhijit Kulkarni, MD6. P2311 - Extramedullary Plasmacytoma Masquerading as a Pancreatic and Duodenal Mass: A Rare Case, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Allegheny Center for Digestive Health, Pittsburgh, PA; 2SUNY Upstate Medical University Hospital, Syracuse, NY; 3Cleveland Clinic Foundation, Cleveland, OH; 4Allegheny Health Network, Pittsburgh, PA; 5University of Florida College of Medicine, Jacksonville, FL; 6Allegheny General Hospital, Pittsburgh, PA
Introduction: Plasmacytomas are rare plasma cell neoplasms with monoclonal proliferation outside the bone marrow. They are classified as solitary bone plasmacytomas (SBP) or extramedullary plasmacytomas (EMP), the latter comprising < 5% of plasma cell malignancies. EMPs may arise de novo or alongside systemic multiple myeloma, often signaling aggressive disease. While most affect the head, neck, or lungs, gastrointestinal (GI) involvement is rare and can mimic adenocarcinoma, lymphoma, or neuroendocrine tumors. We present a patient with multiple myeloma and progression to EMPs involving the pancreas and duodenum.
Case Description/
Methods: A 63-year-old male with immunoglobulin A (IgA) lambda light chain MM presented with several weeks of worsening lethargy. He was diagnosed three years prior, with bone marrow biopsy showing 23% clonal plasma cells expressing CD138 and lambda light chain restriction. Cytogenetics revealed immunoglobulin heavy chain (IGH) fusion, fibroblast growth factor receptor 2 (FGFR2) loss (chromosome 4), and tumor protein 53 (TP53) deletion (chromosome 17). He initially received bortezomib-based therapy, followed by four cycles of daratumumab, lenalidomide, bortezomib, and dexamethasone (DRVD), then underwent autologous stem cell transplant with daratumumab maintenance. Six months later, PET showed new lytic lesions, prompting initiation of daratumumab, pomalidomide, and dexamethasone (DPd). On admission, labs included: WBC 5.3, hemoglobin 12.6, platelets 366, ALT 124, ALP 139, bilirubin 1.3. CT revealed bilateral lung nodules and a 4.7 cm pancreatic head mass abutting the superior mesenteric vessels. Brain MRI showed calvarial enhancement. EUS demonstrated a 3.7 cm irregular pancreatic mass; EGD revealed duodenal nodules. Biopsies from both confirmed EMP with CD138-positive, lambda light chain–restricted plasma cells. He was started on bortezomib, dexamethasone, cisplatin, doxorubicin, cyclophosphamide, and etoposide (VD-PACE).
Discussion: GI EMPs are rare and often misdiagnosed due to nonspecific symptoms and imaging overlap with adenocarcinomas. Mechanisms include hematogenous spread or direct extension; loss of CD56 may facilitate dissemination. TP53 deletion correlates with poor prognosis. Diagnosis relies on biopsy and immunohistochemistry. Treatment is typically systemic, though localized EMPs may benefit from radiation. This case highlights the importance of considering GI EMPs in MM patients presenting with new GI symptoms.
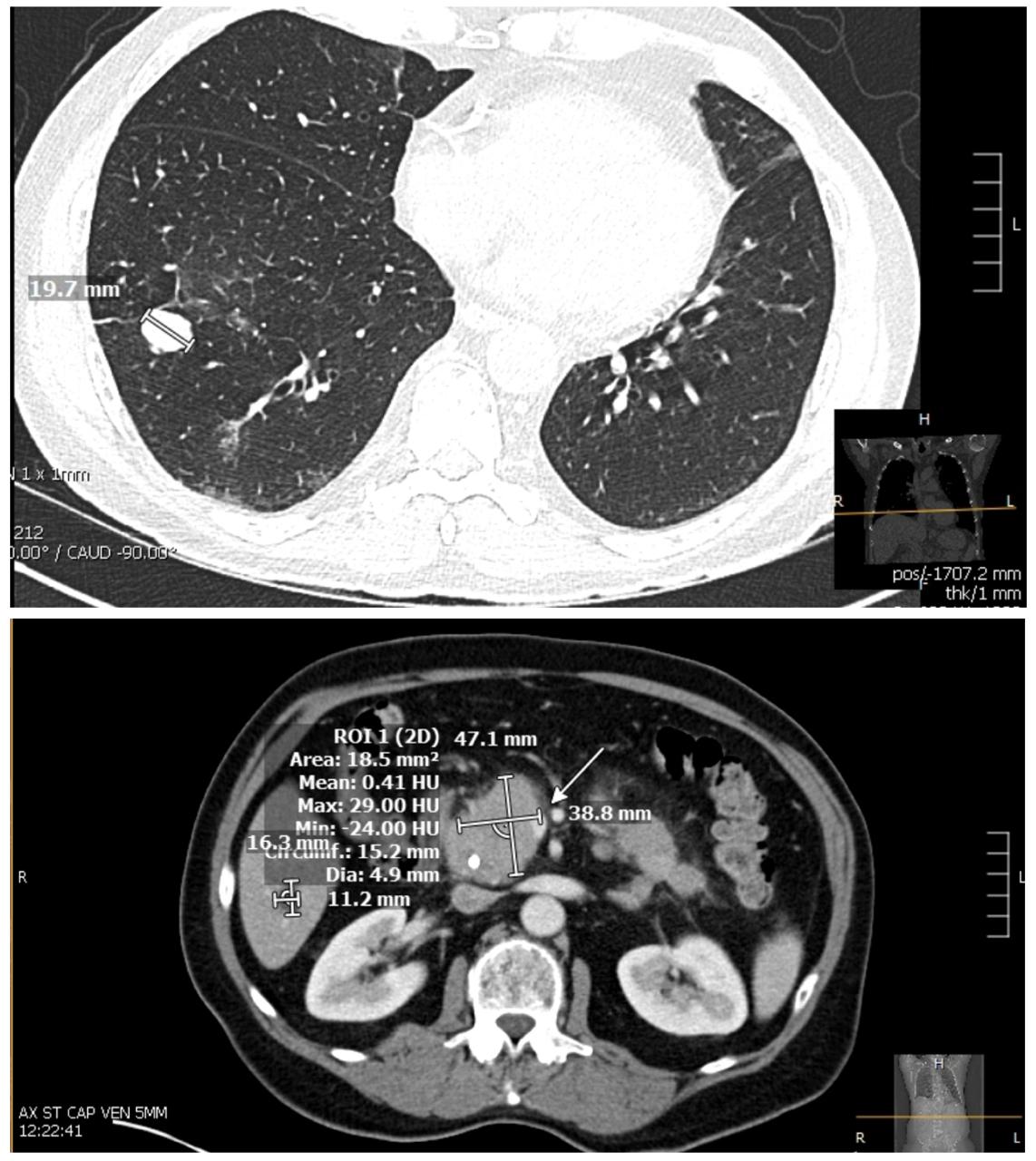
Figure: Image 1: CT chest showing pulmonary nodule and multifocal mass like thickening of the pancreas most notably in the pancreatic head.
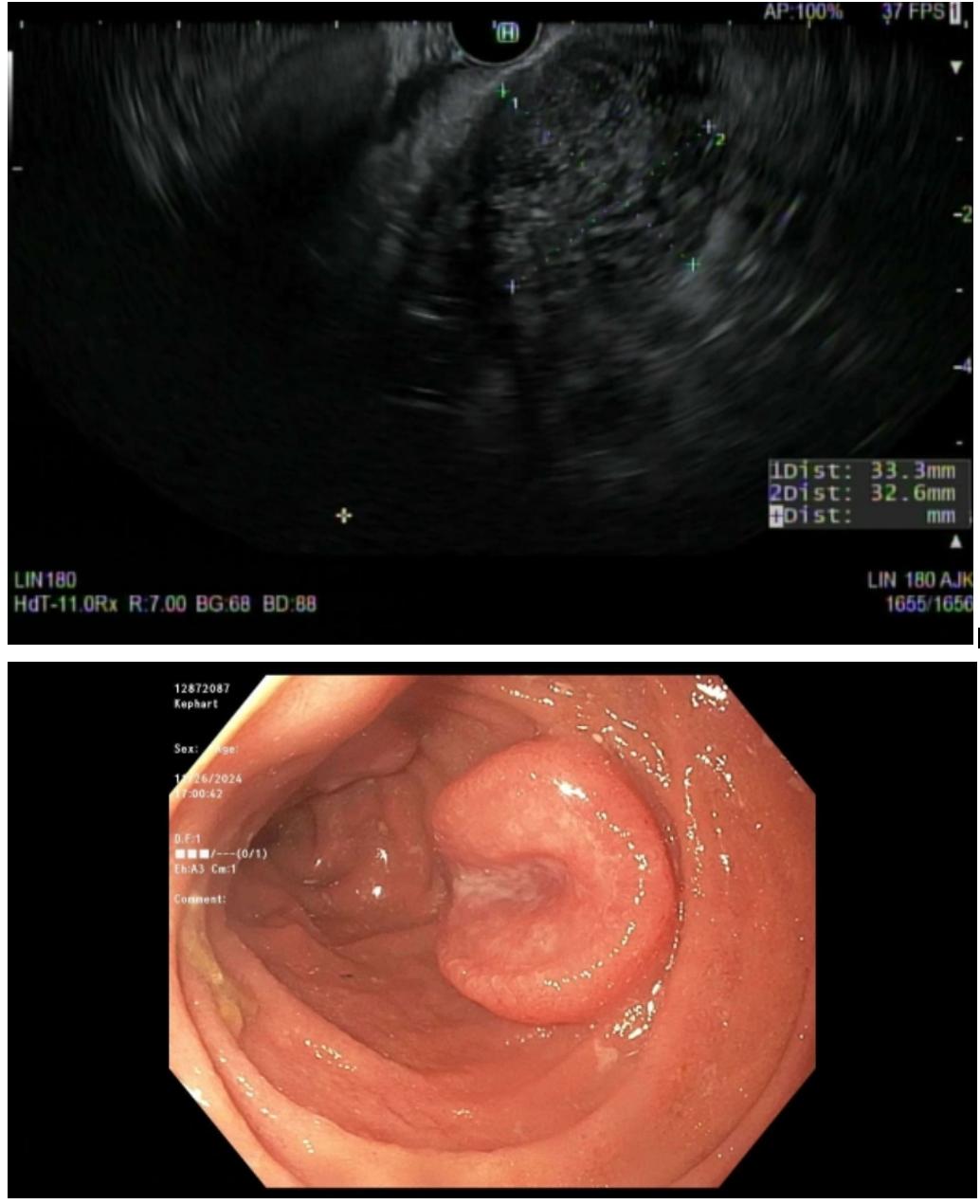
Figure: Image 2: Endoscopic ultrasound showing abnormal pancreatic parenchyma along the head & Duodenal nodule seen on Esophagogastroduodenoscopy
Disclosures:
Somtochukwu Onwuzo indicated no relevant financial relationships.
Chidera Onwuzo indicated no relevant financial relationships.
Rashid Abdel-Razeq indicated no relevant financial relationships.
Kojo-Frimpong B. Awuah indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Abhijit Kulkarni indicated no relevant financial relationships.
Somtochukwu Onwuzo, MD1, Chidera Onwuzo, MBBS2, Rashid Abdel-Razeq, MD3, Kojo-Frimpong B. Awuah, MD4, Antoine Boustany, MD5, Abhijit Kulkarni, MD6. P2311 - Extramedullary Plasmacytoma Masquerading as a Pancreatic and Duodenal Mass: A Rare Case, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
