Monday Poster Session
Category: Biliary/Pancreas
P2221 - Predictors of Early-Onset Pancreatic Cancer: A Population-Based Case-Control Study in the United States
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Omar Abureesh, MD (he/him/his)
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Omar Abureesh, MD1, Ahmad Abdulraheem, MD2, Abdellatif Ismail, MD3, Mohammed Al-Aquily, MD4, Toni Habib, MD1, Mohammed Aloqaily, MD5, Youssef El Douaihy, MD1, Sherif Andrawes, MD1, Jean Chalhoub, MD1
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2MedStar Washington Hospital Center-Georgetown University, Washington, DC; 3University of Maryland, Baltimore, MD; 4Norwalk Hospital/Yale University, Norwalk, CT; 5University of Maryland Medical Center Midtown Campus, Baltimore, MD
Introduction: Early-onset pancreatic cancer (EOPC), defined as pancreatic cancer diagnosed before the age of 50, accounts for 8-10% of all pancreatic cancer cases and presents unique challenges due to delayed diagnosis and the absence of screening guidelines. Understanding risk factors specific to this population is essential for improving early detection and outcomes.
Methods: We conducted a retrospective case-control study using TriNetX, a global database of de-identified electronic health records. Adults aged 18–50 diagnosed with exocrine pancreatic cancer between May 2005 and May 2025 were identified as cases. Individuals without pancreatic cancer served as controls. We excluded all patients with neuroendocrine tumors based on ICD-10 codes. We compared demographic, comorbidities, and genetic mutations between both groups. A P-value < 0.05 was considered statistically significant.
Results: A total of 16,375 cases and 4,544,188 controls were analysed. Demographic distribution of both groups is shown in figure 1. Caucasians had a higher prevalence of EOPC compared to other racial groups. A history of acute pancreatitis (8.6% vs. 0.6%; OR: 15.13; 95% CI: 14.31–15.99), chronic pancreatitis (7.9% vs. 0.2%; OR: 46.72; 95% CI: 43.97–49.64), nicotine dependence (10.5% vs. 9.6%; OR: 1.11; 95% CI: 1.05–1.16) and alcohol-related disorders (3.8% vs. 2.8%; OR: 1.35; 95% CI: 1.24–1.46) were more prevalent in cases of pancreatic cancer compared to controls. Interestingly, while previous studies reported an association between overweight/obesity and pancreatic cancer, our data showed a decreased prevalence of EOPC these patients (10.6% vs. 15.4%; OR: 0.65; 95% CI: 0.62–0.69). KRAS mutations were more frequently reported in cases (0.1% vs. 0.0%). Other germline mutations were infrequently tested and not statistically significant in this dataset.
Discussion: Pancreatitis, smoking, alcohol use, racial patterns, and genetic predisposition showed an association with EOPC. This study highlights the need for further research evaluating the specific predictors of EOPC, which could guide targeted screening and prevention strategies.
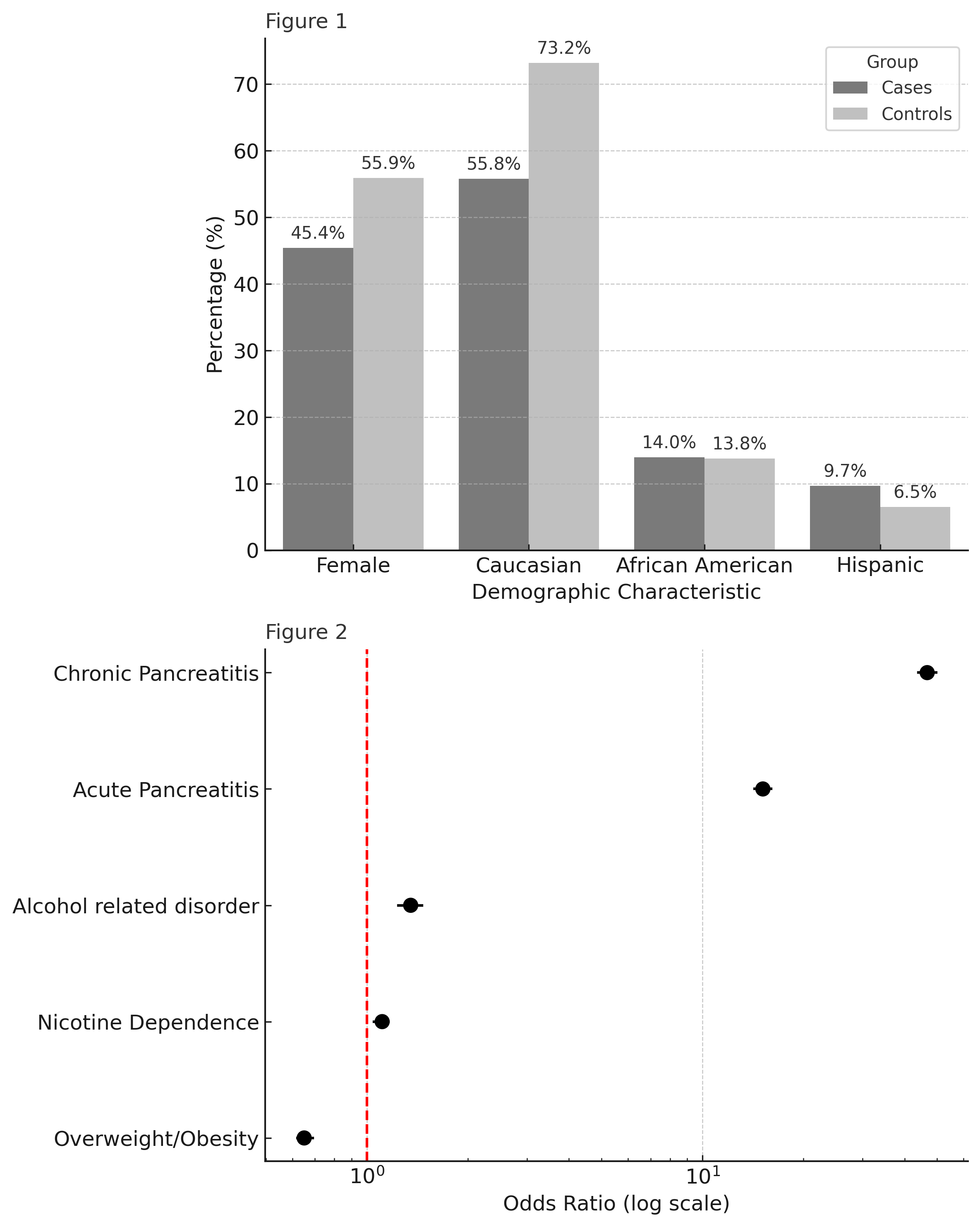
Figure: Table 1: Baseline characteristics and predictors of early-onset pancreatic cancer cases vs controls
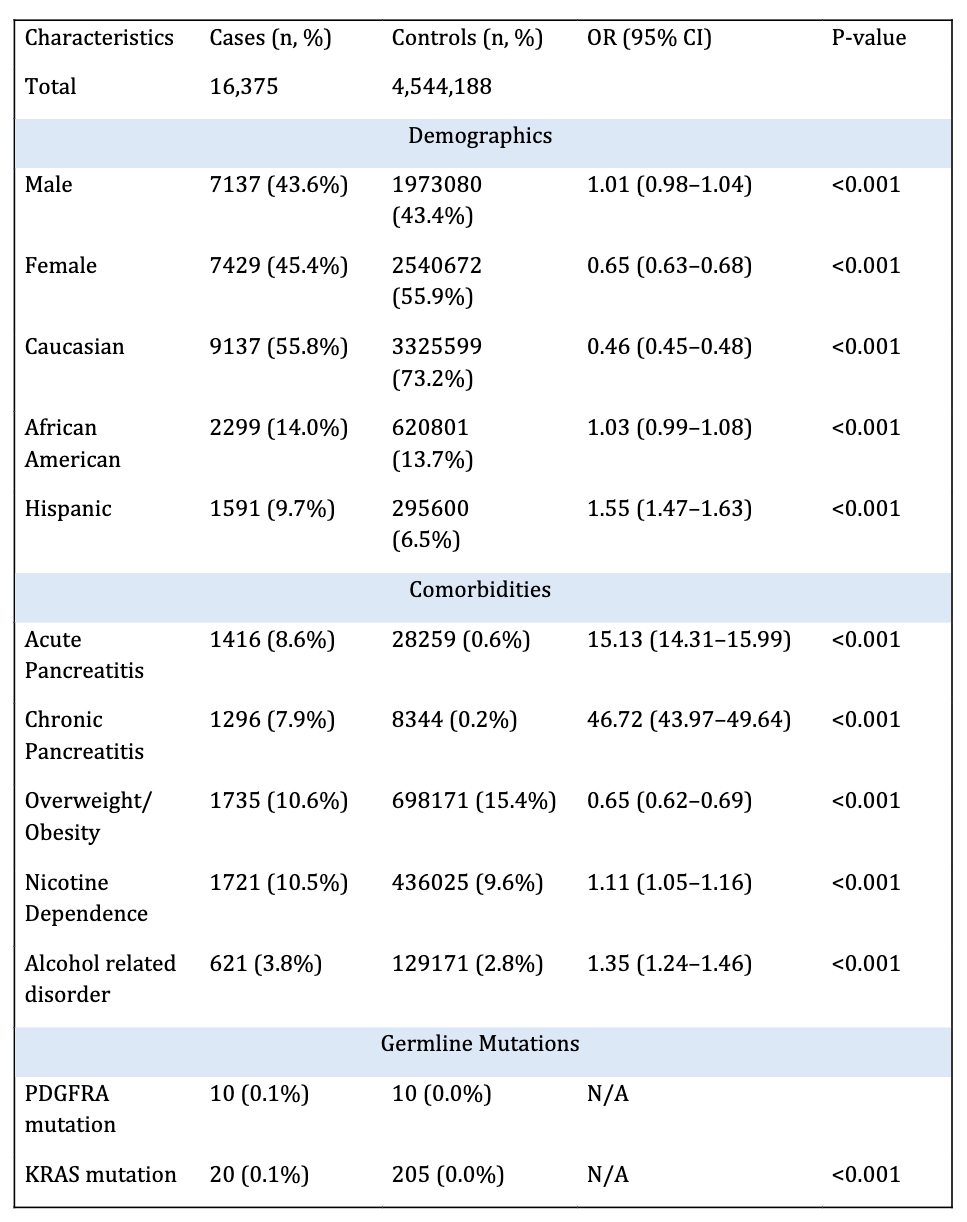
Figure: Figure 1: Demographic characteristics of cases vs. controls.
Figure 2: Forest plot of non-genetic predictors of early-onset pancreatic cancer.
Disclosures:
Omar Abureesh indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Toni Habib indicated no relevant financial relationships.
Mohammed Aloqaily indicated no relevant financial relationships.
Youssef El Douaihy indicated no relevant financial relationships.
Sherif Andrawes indicated no relevant financial relationships.
Jean Chalhoub indicated no relevant financial relationships.
Omar Abureesh, MD1, Ahmad Abdulraheem, MD2, Abdellatif Ismail, MD3, Mohammed Al-Aquily, MD4, Toni Habib, MD1, Mohammed Aloqaily, MD5, Youssef El Douaihy, MD1, Sherif Andrawes, MD1, Jean Chalhoub, MD1. P2221 - Predictors of Early-Onset Pancreatic Cancer: A Population-Based Case-Control Study in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2MedStar Washington Hospital Center-Georgetown University, Washington, DC; 3University of Maryland, Baltimore, MD; 4Norwalk Hospital/Yale University, Norwalk, CT; 5University of Maryland Medical Center Midtown Campus, Baltimore, MD
Introduction: Early-onset pancreatic cancer (EOPC), defined as pancreatic cancer diagnosed before the age of 50, accounts for 8-10% of all pancreatic cancer cases and presents unique challenges due to delayed diagnosis and the absence of screening guidelines. Understanding risk factors specific to this population is essential for improving early detection and outcomes.
Methods: We conducted a retrospective case-control study using TriNetX, a global database of de-identified electronic health records. Adults aged 18–50 diagnosed with exocrine pancreatic cancer between May 2005 and May 2025 were identified as cases. Individuals without pancreatic cancer served as controls. We excluded all patients with neuroendocrine tumors based on ICD-10 codes. We compared demographic, comorbidities, and genetic mutations between both groups. A P-value < 0.05 was considered statistically significant.
Results: A total of 16,375 cases and 4,544,188 controls were analysed. Demographic distribution of both groups is shown in figure 1. Caucasians had a higher prevalence of EOPC compared to other racial groups. A history of acute pancreatitis (8.6% vs. 0.6%; OR: 15.13; 95% CI: 14.31–15.99), chronic pancreatitis (7.9% vs. 0.2%; OR: 46.72; 95% CI: 43.97–49.64), nicotine dependence (10.5% vs. 9.6%; OR: 1.11; 95% CI: 1.05–1.16) and alcohol-related disorders (3.8% vs. 2.8%; OR: 1.35; 95% CI: 1.24–1.46) were more prevalent in cases of pancreatic cancer compared to controls. Interestingly, while previous studies reported an association between overweight/obesity and pancreatic cancer, our data showed a decreased prevalence of EOPC these patients (10.6% vs. 15.4%; OR: 0.65; 95% CI: 0.62–0.69). KRAS mutations were more frequently reported in cases (0.1% vs. 0.0%). Other germline mutations were infrequently tested and not statistically significant in this dataset.
Discussion: Pancreatitis, smoking, alcohol use, racial patterns, and genetic predisposition showed an association with EOPC. This study highlights the need for further research evaluating the specific predictors of EOPC, which could guide targeted screening and prevention strategies.
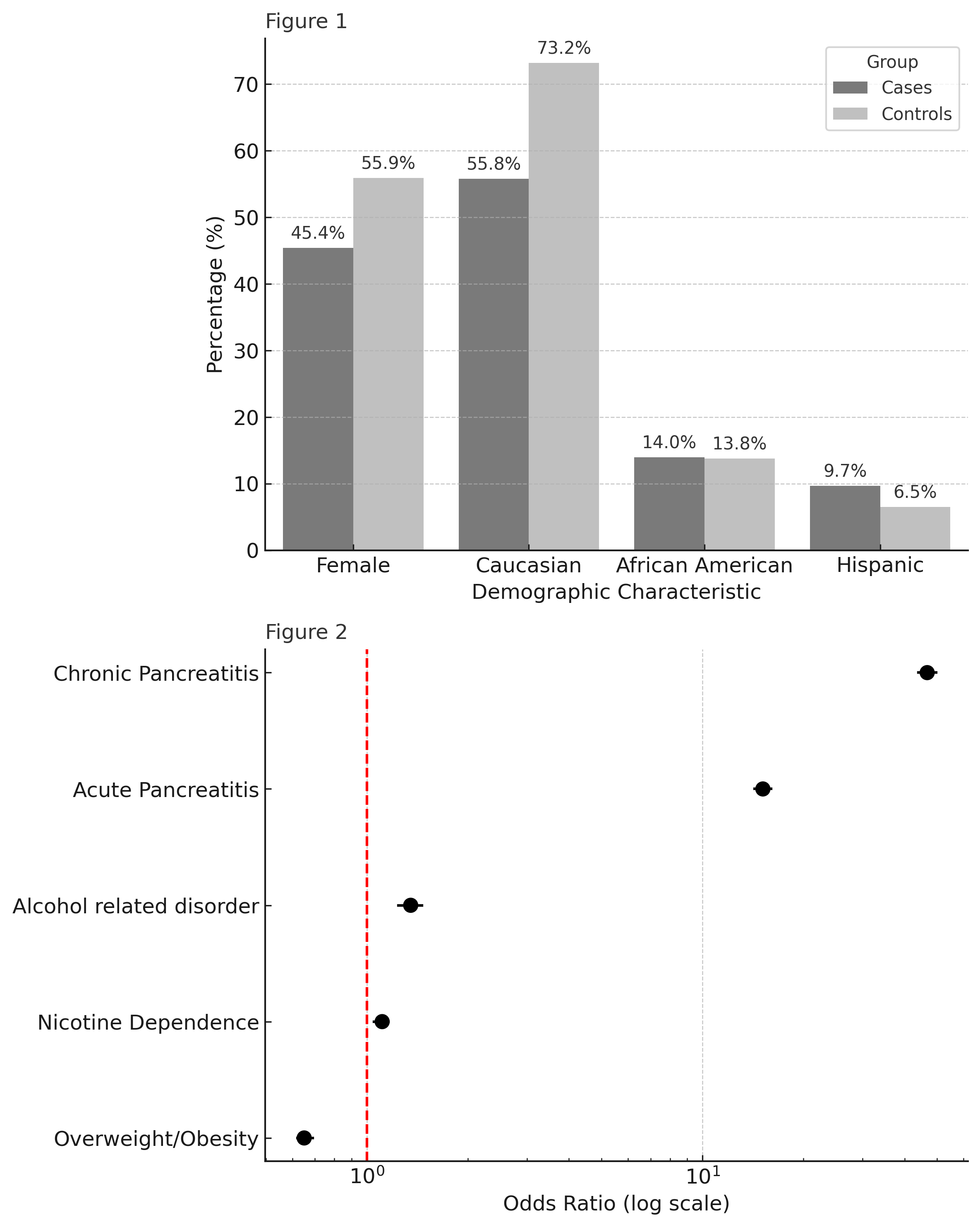
Figure: Table 1: Baseline characteristics and predictors of early-onset pancreatic cancer cases vs controls
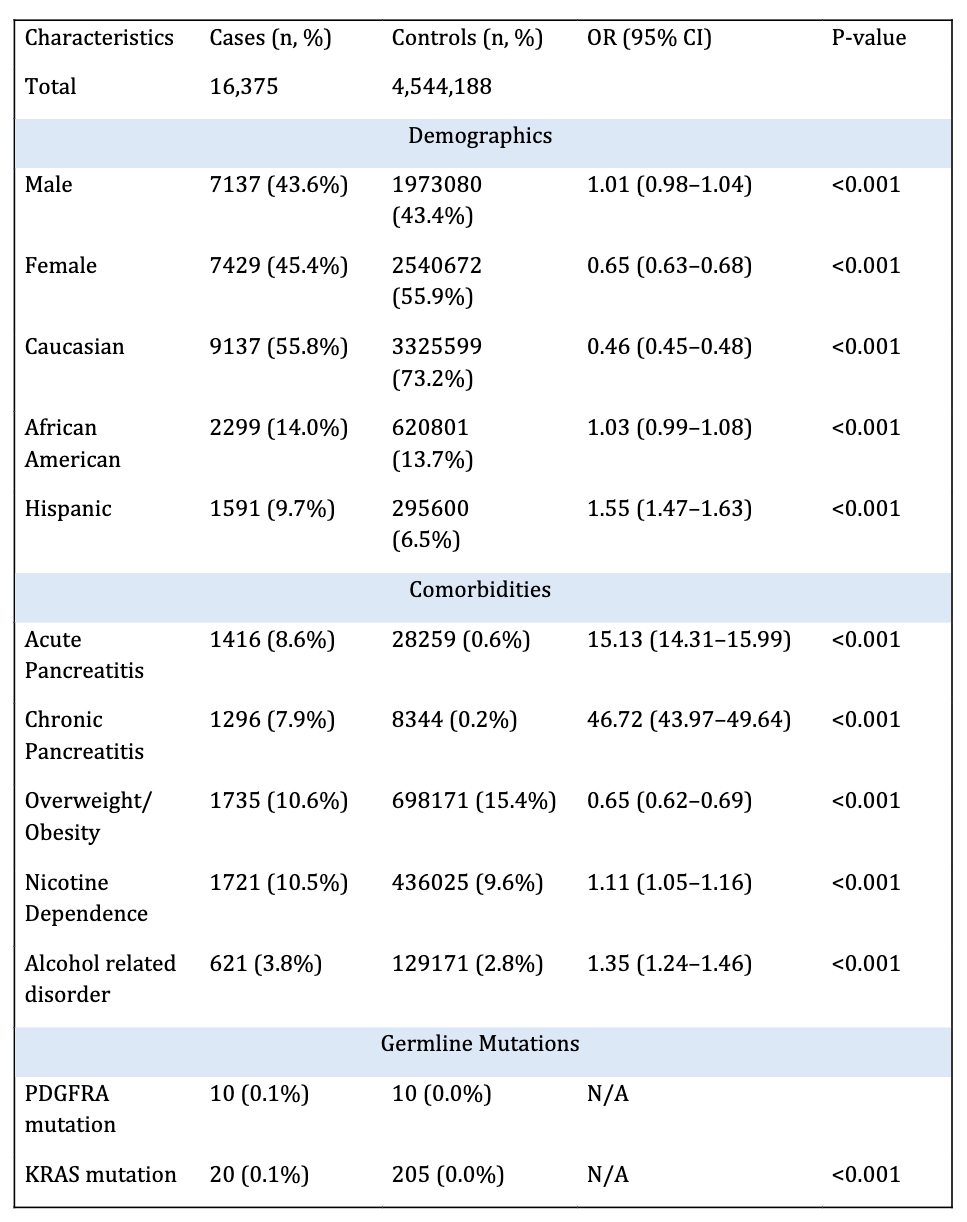
Figure: Figure 1: Demographic characteristics of cases vs. controls.
Figure 2: Forest plot of non-genetic predictors of early-onset pancreatic cancer.
Disclosures:
Omar Abureesh indicated no relevant financial relationships.
Ahmad Abdulraheem indicated no relevant financial relationships.
Abdellatif Ismail indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Toni Habib indicated no relevant financial relationships.
Mohammed Aloqaily indicated no relevant financial relationships.
Youssef El Douaihy indicated no relevant financial relationships.
Sherif Andrawes indicated no relevant financial relationships.
Jean Chalhoub indicated no relevant financial relationships.
Omar Abureesh, MD1, Ahmad Abdulraheem, MD2, Abdellatif Ismail, MD3, Mohammed Al-Aquily, MD4, Toni Habib, MD1, Mohammed Aloqaily, MD5, Youssef El Douaihy, MD1, Sherif Andrawes, MD1, Jean Chalhoub, MD1. P2221 - Predictors of Early-Onset Pancreatic Cancer: A Population-Based Case-Control Study in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
