Monday Poster Session
Category: Biliary/Pancreas
P2211 - The Prevalence of Metabolic Syndrome and Its Association With Cardiovascular Outcomes in Hospitalized Patients with Exocrine Pancreatic Insufficiency
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Toni Habib, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Toni Habib, MD1, Chloe Lahoud, MD1, Daniel Kallta, DO1, Chapman Wei, MD1, Razan Dankar, MD1, Elie Moussa, MD1, Bivin George, DO, PharmD2, Malek Kreidieh, MD3, Youssef El Douaihy, MD1, Jean Chalhoub, MD1, Sherif Andrawes, MD1
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Staten Island University Hospital, Northwell Health, New York City, NY; 3Staten Island University Hospital, Staten Island, NY
Introduction: Exocrine pancreatic insufficiency (EPI) disrupts the digestion and absorption of nutrients, leading to significant health issues including potential cardiovascular consequences. While metabolic syndrome (MetS) is known to exacerbate cardiovascular risks, its prevalence and impact on cardiovascular health in EPI patients remain insufficiently explored. Understanding this association could unveil critical insights for managing cardiovascular outcomes in this population.
Methods: This study includes data from the Nationwide Inpatient Sample (NIS) database, which encompasses 24,925,252 individuals, 19,402 of whom had EPI using International Classification of Diseases, 10th Edition (ICD-10) codes. MetS prevalence was assessed using a Calculated Metabolic Score (CMS). Multivariate binary logistic regressions were performed to examine the associations between MetS components (obesity, type II diabetes mellitus [DM], dyslipidemia [DLD], and hypertension [HTN]) and cardiovascular outcomes such as acute coronary syndrome (ACS), coronary artery disease (CAD), heart failure (HF), cerebrovascular accidents (CVAs), peripheral vascular disease (PVD), and transient ischemic attacks (TIAs).
Results: EPI patients exhibited lower odds of MetS compared to non-EPI patients, with a prevalence of MetS at 2.75% versus 3.83% in non-EPI individuals. Obesity and HTN were found to be less prevalent in patients with EPI while DM was significantly more prevalent in this population. EPI was significantly associated with lower odds of ACS, CAD, HF, CVA, and TIA. However, metabolic syndrome components like HTN, DM, and DLD still posed increased cardiovascular risks when present.
Discussion: The study underscores unique pathophysiological mechanisms in EPI patients that could influence metabolic stress and inflammatory pathways, potentially offering protective effects against certain cardiovascular events. This highlights the potential need for tailored cardiovascular risk assessment and management in the EPI population. Prospective research is required to further understand these relationships and refine management strategies for EPI patients.
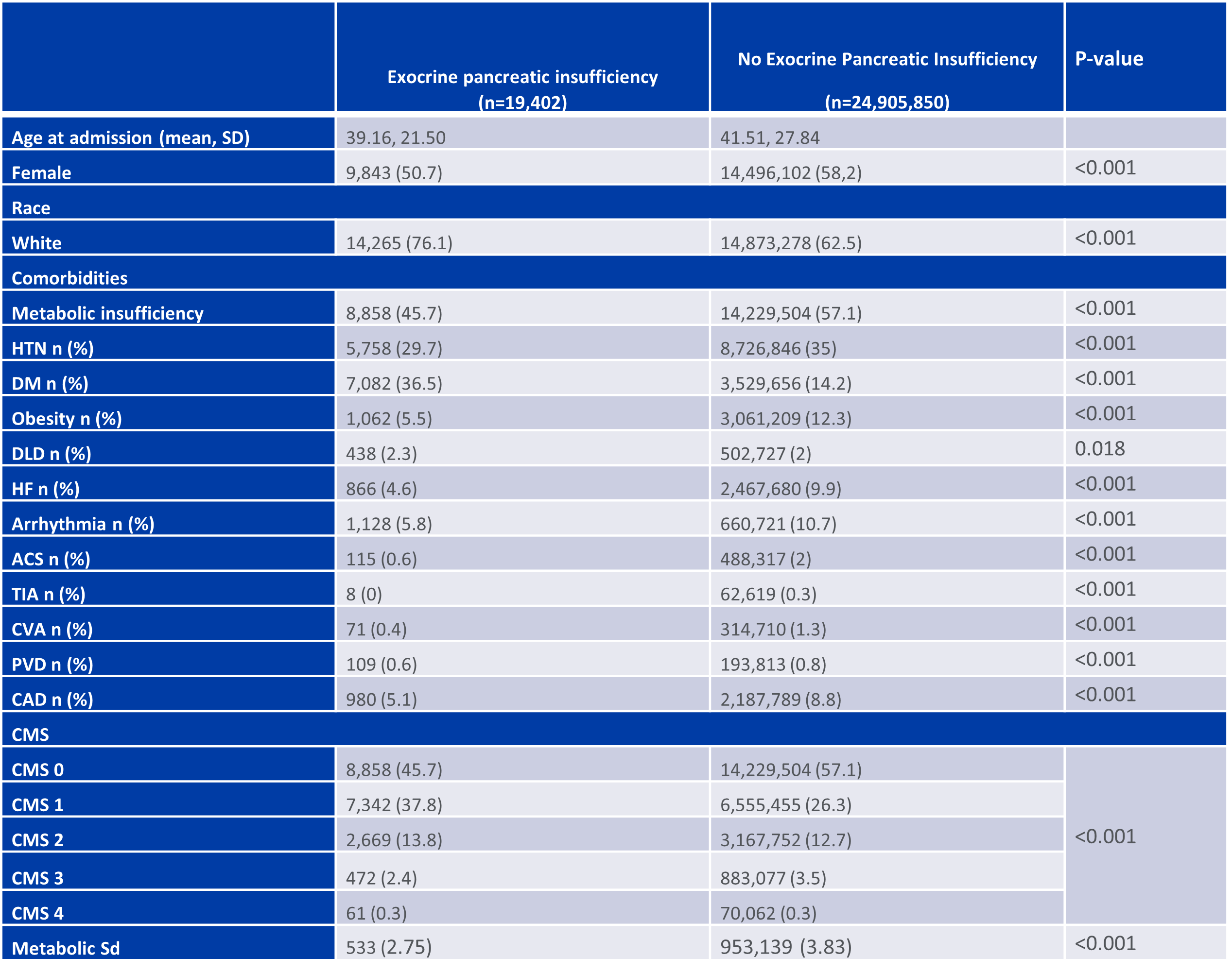
Figure: Demographic and Clinical Characteristics of Exocrine Pancreatic Insufficiency Versus Non-Exocrine Pancreatic Insufficiency Patients.
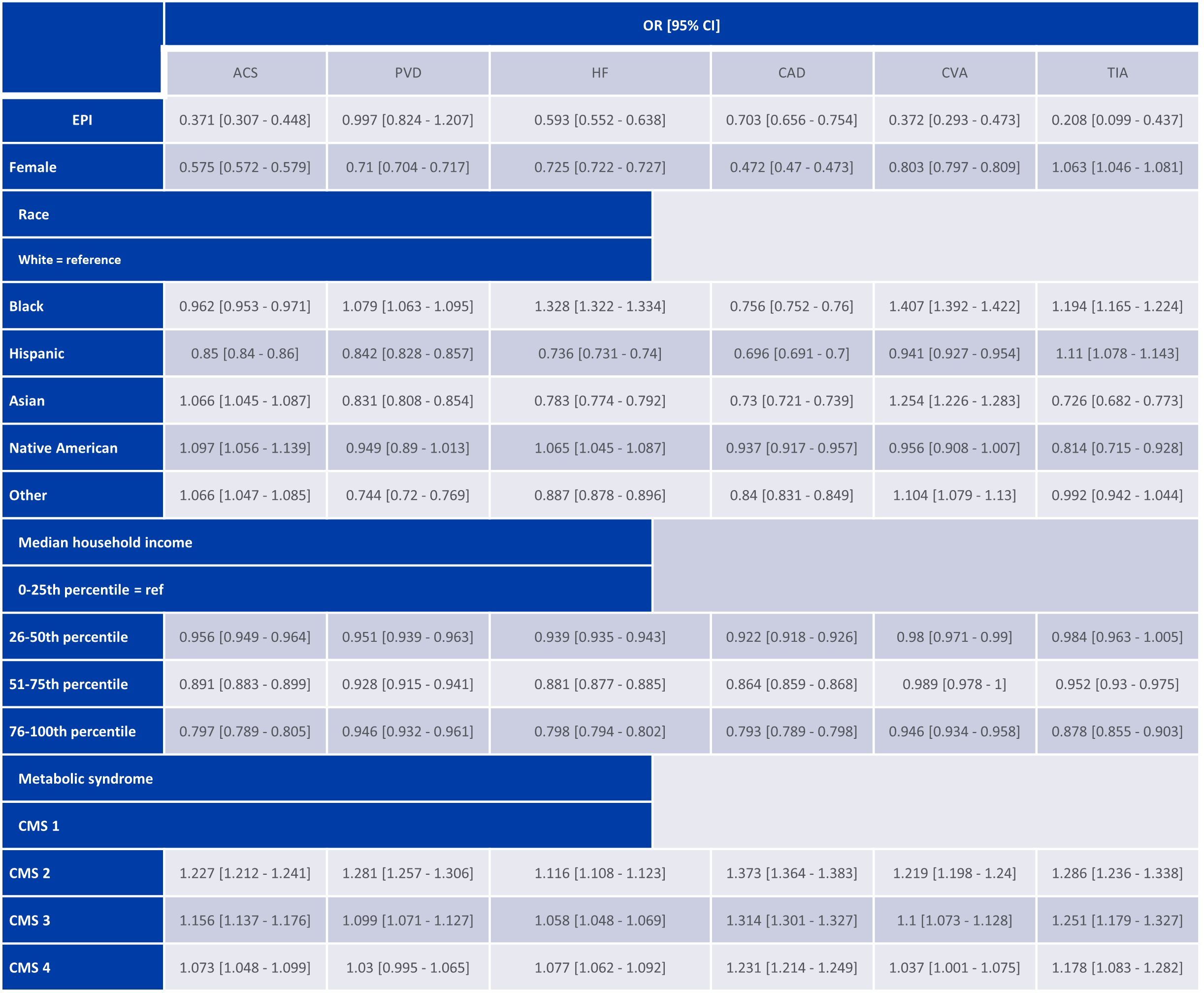
Figure: Association of metabolic syndrome with cardiovascular outcomes of interests in patients with Exocrine Pancreatic Insufficiency.
Disclosures:
Toni Habib indicated no relevant financial relationships.
Chloe Lahoud indicated no relevant financial relationships.
Daniel Kallta indicated no relevant financial relationships.
Chapman Wei indicated no relevant financial relationships.
Razan Dankar indicated no relevant financial relationships.
Elie Moussa indicated no relevant financial relationships.
Bivin George indicated no relevant financial relationships.
Malek Kreidieh indicated no relevant financial relationships.
Youssef El Douaihy indicated no relevant financial relationships.
Jean Chalhoub indicated no relevant financial relationships.
Sherif Andrawes indicated no relevant financial relationships.
Toni Habib, MD1, Chloe Lahoud, MD1, Daniel Kallta, DO1, Chapman Wei, MD1, Razan Dankar, MD1, Elie Moussa, MD1, Bivin George, DO, PharmD2, Malek Kreidieh, MD3, Youssef El Douaihy, MD1, Jean Chalhoub, MD1, Sherif Andrawes, MD1. P2211 - The Prevalence of Metabolic Syndrome and Its Association With Cardiovascular Outcomes in Hospitalized Patients with Exocrine Pancreatic Insufficiency, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Staten Island University Hospital, Northwell Health, Staten Island, NY; 2Staten Island University Hospital, Northwell Health, New York City, NY; 3Staten Island University Hospital, Staten Island, NY
Introduction: Exocrine pancreatic insufficiency (EPI) disrupts the digestion and absorption of nutrients, leading to significant health issues including potential cardiovascular consequences. While metabolic syndrome (MetS) is known to exacerbate cardiovascular risks, its prevalence and impact on cardiovascular health in EPI patients remain insufficiently explored. Understanding this association could unveil critical insights for managing cardiovascular outcomes in this population.
Methods: This study includes data from the Nationwide Inpatient Sample (NIS) database, which encompasses 24,925,252 individuals, 19,402 of whom had EPI using International Classification of Diseases, 10th Edition (ICD-10) codes. MetS prevalence was assessed using a Calculated Metabolic Score (CMS). Multivariate binary logistic regressions were performed to examine the associations between MetS components (obesity, type II diabetes mellitus [DM], dyslipidemia [DLD], and hypertension [HTN]) and cardiovascular outcomes such as acute coronary syndrome (ACS), coronary artery disease (CAD), heart failure (HF), cerebrovascular accidents (CVAs), peripheral vascular disease (PVD), and transient ischemic attacks (TIAs).
Results: EPI patients exhibited lower odds of MetS compared to non-EPI patients, with a prevalence of MetS at 2.75% versus 3.83% in non-EPI individuals. Obesity and HTN were found to be less prevalent in patients with EPI while DM was significantly more prevalent in this population. EPI was significantly associated with lower odds of ACS, CAD, HF, CVA, and TIA. However, metabolic syndrome components like HTN, DM, and DLD still posed increased cardiovascular risks when present.
Discussion: The study underscores unique pathophysiological mechanisms in EPI patients that could influence metabolic stress and inflammatory pathways, potentially offering protective effects against certain cardiovascular events. This highlights the potential need for tailored cardiovascular risk assessment and management in the EPI population. Prospective research is required to further understand these relationships and refine management strategies for EPI patients.
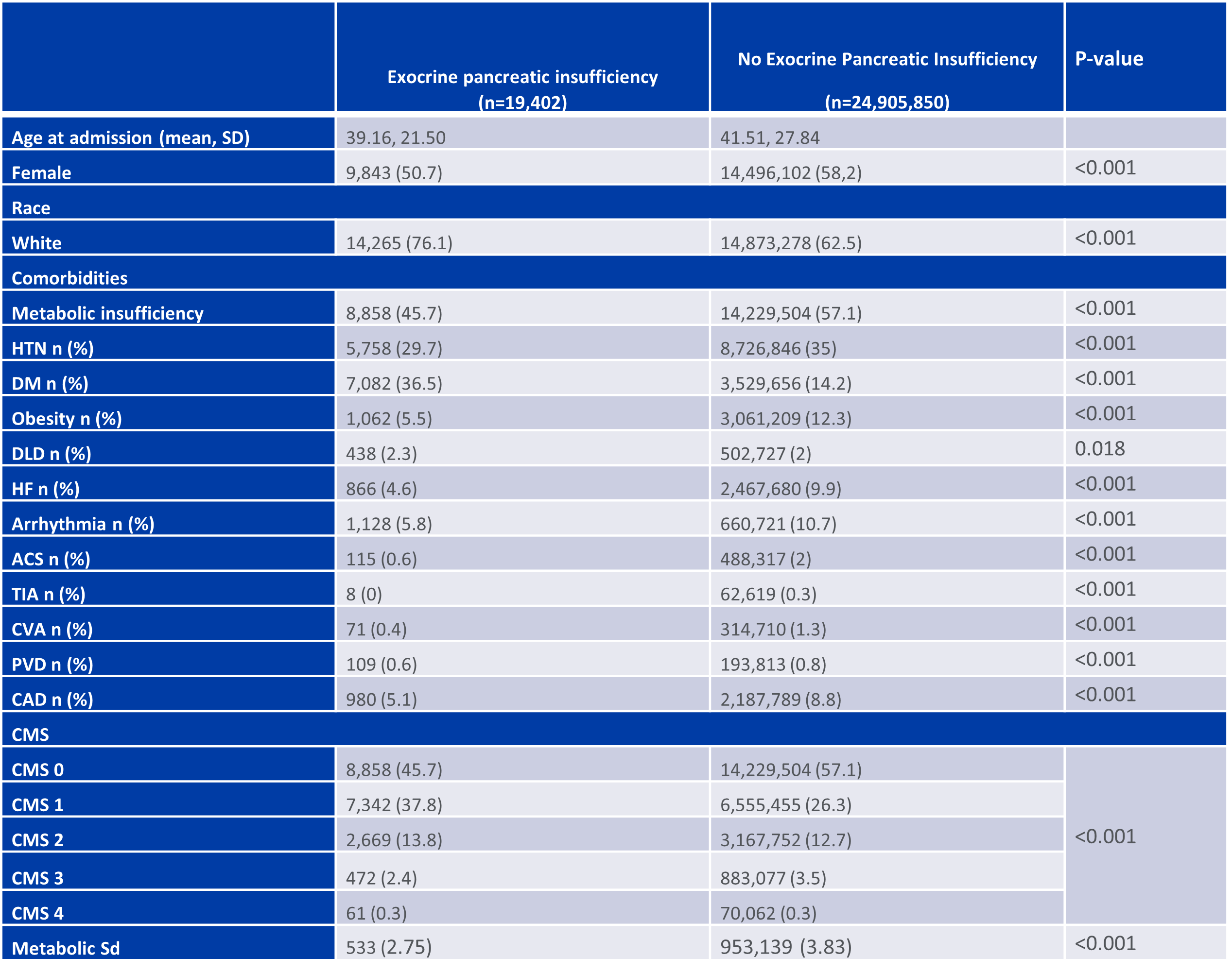
Figure: Demographic and Clinical Characteristics of Exocrine Pancreatic Insufficiency Versus Non-Exocrine Pancreatic Insufficiency Patients.
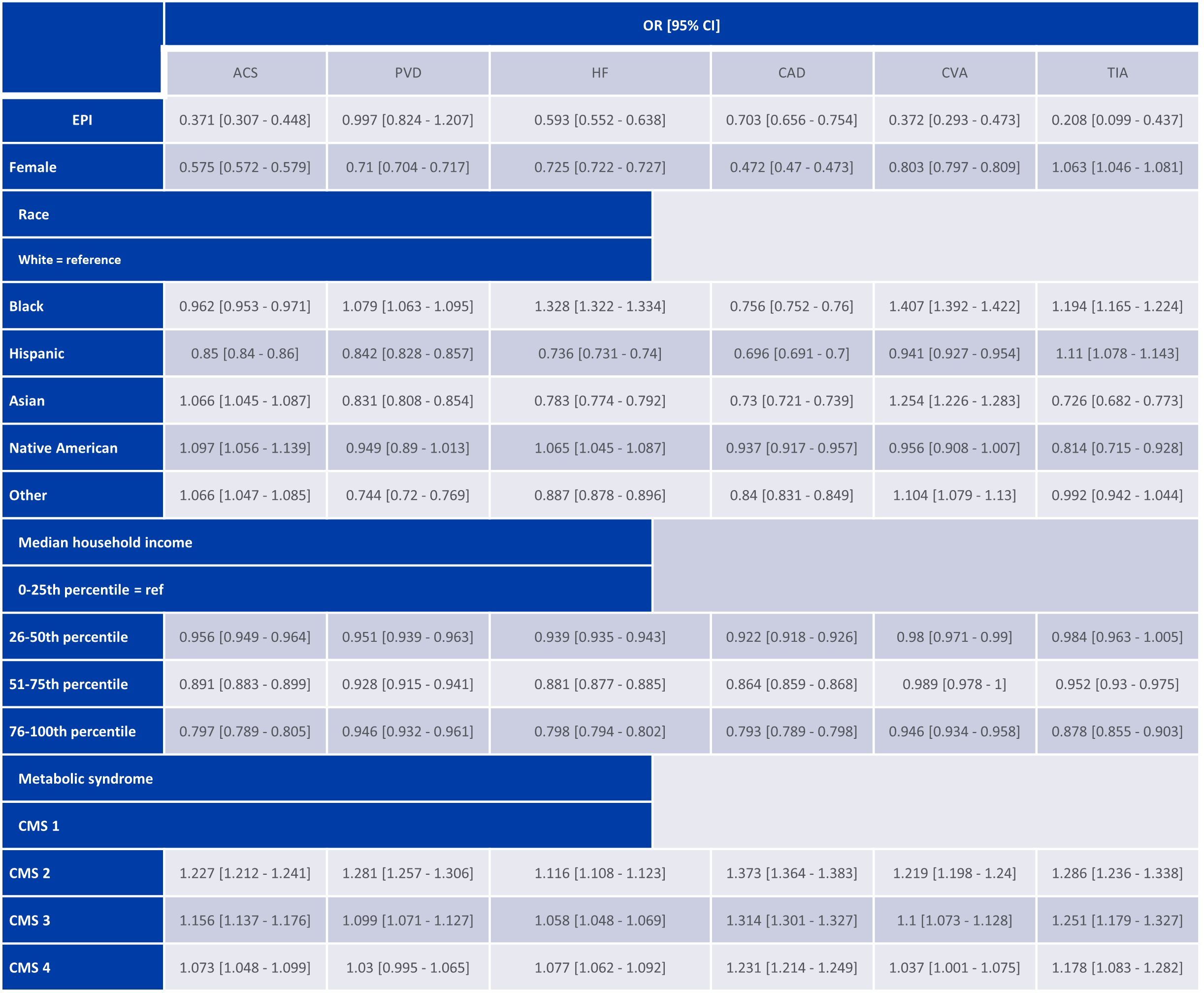
Figure: Association of metabolic syndrome with cardiovascular outcomes of interests in patients with Exocrine Pancreatic Insufficiency.
Disclosures:
Toni Habib indicated no relevant financial relationships.
Chloe Lahoud indicated no relevant financial relationships.
Daniel Kallta indicated no relevant financial relationships.
Chapman Wei indicated no relevant financial relationships.
Razan Dankar indicated no relevant financial relationships.
Elie Moussa indicated no relevant financial relationships.
Bivin George indicated no relevant financial relationships.
Malek Kreidieh indicated no relevant financial relationships.
Youssef El Douaihy indicated no relevant financial relationships.
Jean Chalhoub indicated no relevant financial relationships.
Sherif Andrawes indicated no relevant financial relationships.
Toni Habib, MD1, Chloe Lahoud, MD1, Daniel Kallta, DO1, Chapman Wei, MD1, Razan Dankar, MD1, Elie Moussa, MD1, Bivin George, DO, PharmD2, Malek Kreidieh, MD3, Youssef El Douaihy, MD1, Jean Chalhoub, MD1, Sherif Andrawes, MD1. P2211 - The Prevalence of Metabolic Syndrome and Its Association With Cardiovascular Outcomes in Hospitalized Patients with Exocrine Pancreatic Insufficiency, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
