Monday Poster Session
Category: Biliary/Pancreas
P2206 - Incidence of Acute Pancreatitis With GLP-1 Receptor Agonists (GLP-1 RA) Use Across Obesity and Type 2 Diabetes Phenotypes: A Multi-Center Analysis
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ruchir Paladiya, MBBS
University of Connecticut School of Medicine
Farmington, CT
Presenting Author(s)
Ruchir Paladiya, MBBS1, Himsikhar Khataniar, MD2, Karthik Mathialagan, MD3, Murali Dharan, 4
1University of Connecticut School of Medicine, Farmington, CT; 2Allegheny General Hospital, Pittsburgh, PA; 3University of Connecticut, Farmington, CT; 4Employed, Farmington, CT
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs), approved for obesity and type 2 diabetes mellitus (T2DM) treatment, have been linked to acute pancreatitis (AP). We evaluated whether AP risk with GLP-1 RA therapy differs among patients with obesity alone, T2DM alone, or both.
Methods: A retrospective cohort study was performed using TriNetX data base to compare 730-day AP risk in adults (≥ 18 y) newly prescribed GLP-1 RAs with obesity only, T2DM only, or both. The primary aim was to determine if combined obesity and T2DM modified AP risk versus either condition alone. We excluded patients with prior AP (ICD-10 K85.x) or missing demographics. Two pairwise, one-to-one propensity score–matched comparisons— (1) obesity + GLP-1 RA versus obesity + T2DM + GLP-1 RA and (2) T2DM + GLP-1 RA versus obesity + T2DM + GLP-1 RA—balanced 34 baseline covariates (demographics; BMI; HbA1c; gallstone disease; alcohol use disorder; hypertriglyceridemia; chronic kidney disease; hypertension; hyperlipidemia; pancreatitis-associated medications), yielding matched cohorts of 35 099 and 66 880 patients, respectively. Incident AP risk was expressed as adjusted odds ratios (aORs) with 95% confidence intervals (CIs) via conditional logistic regression and time-to-event risk as adjusted hazard ratios (aHRs) with 95% CIs via Cox models with Kaplan–Meier/log-rank analyses.
Results: In the obesity comparison, AP incidence was 0.3% in each cohort; the aOR was 0.76 (95% CI, 0.58–1.00) and the aHR 0.87 (95% CI, 0.67–1.12), with 730-day pancreatitis-free survival of 99.64% versus 99.58% (log-rank p = 0.28). In the T2DM comparison, incidence was 0.5% versus 0.4%; the aOR was 1.14 (95% CI, 0.97–1.35) and the aHR 1.13 (95% CI, 0.96–1.34), with survival of 99.50% versus 99.56% (p = 0.14). No comparison reached statistical significance.
Discussion: Our study limitations include retrospective design, possibility of misclassification bias and confounding by other causes of AP. Despite this, our study did not show any significant difference in incidence of AP across metabolic phenotypes. The data appears to suggest that the causal mechanisms for AP may be independent of the phenotypes. Future studies perhaps with longer follow up are required to corroborate our findings and clarify if GLP1 RA dose and duration, pre-existent cholelithiasis and other factors can predict risk of AP.
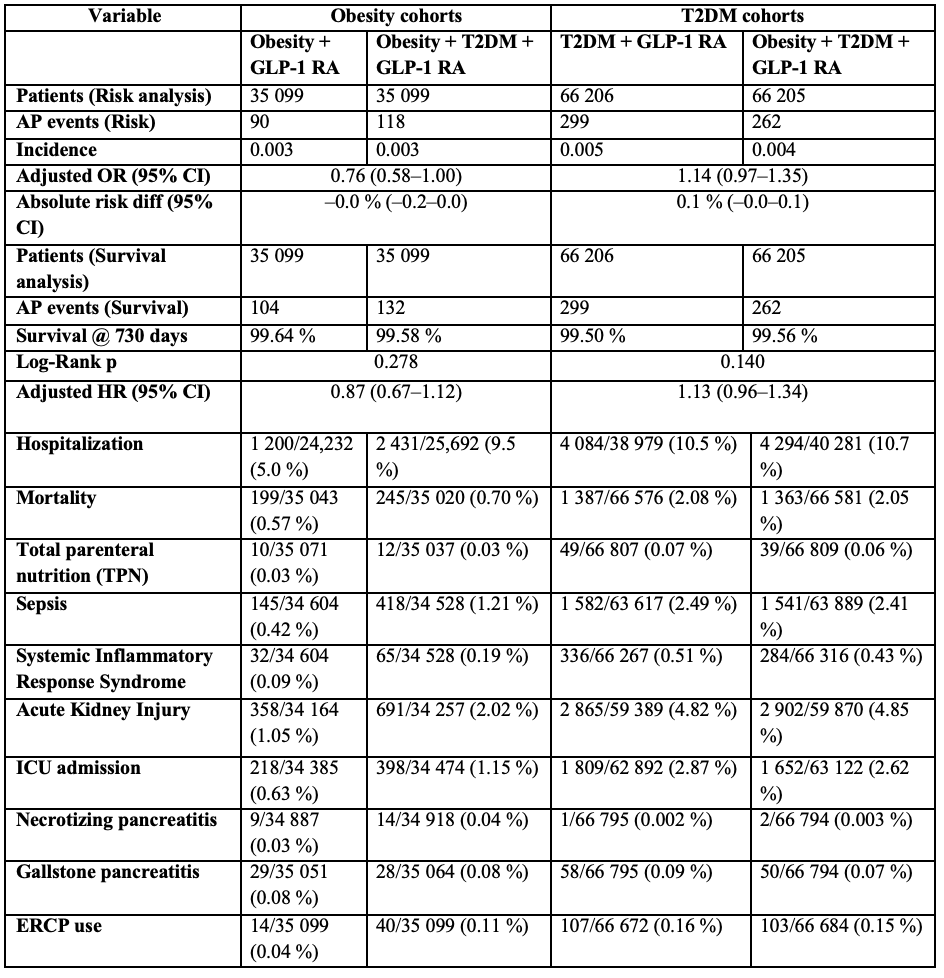
Figure: Table 1. Incidence and adjusted risk of acute pancreatitis and other complications within 730 days of GLP-1 RA initiation across four propensity-matched cohorts (obesity alone, obesity + T2DM, T2DM alone, and obesity + T2DM). Data are presented as n/N (%) for each outcome, with adjusted odds ratios (ORs) and hazard ratios (HRs) with 95% confidence intervals for acute pancreatitis.
Disclosures:
Ruchir Paladiya indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Murali Dharan indicated no relevant financial relationships.
Ruchir Paladiya, MBBS1, Himsikhar Khataniar, MD2, Karthik Mathialagan, MD3, Murali Dharan, 4. P2206 - Incidence of Acute Pancreatitis With GLP-1 Receptor Agonists (GLP-1 RA) Use Across Obesity and Type 2 Diabetes Phenotypes: A Multi-Center Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut School of Medicine, Farmington, CT; 2Allegheny General Hospital, Pittsburgh, PA; 3University of Connecticut, Farmington, CT; 4Employed, Farmington, CT
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RAs), approved for obesity and type 2 diabetes mellitus (T2DM) treatment, have been linked to acute pancreatitis (AP). We evaluated whether AP risk with GLP-1 RA therapy differs among patients with obesity alone, T2DM alone, or both.
Methods: A retrospective cohort study was performed using TriNetX data base to compare 730-day AP risk in adults (≥ 18 y) newly prescribed GLP-1 RAs with obesity only, T2DM only, or both. The primary aim was to determine if combined obesity and T2DM modified AP risk versus either condition alone. We excluded patients with prior AP (ICD-10 K85.x) or missing demographics. Two pairwise, one-to-one propensity score–matched comparisons— (1) obesity + GLP-1 RA versus obesity + T2DM + GLP-1 RA and (2) T2DM + GLP-1 RA versus obesity + T2DM + GLP-1 RA—balanced 34 baseline covariates (demographics; BMI; HbA1c; gallstone disease; alcohol use disorder; hypertriglyceridemia; chronic kidney disease; hypertension; hyperlipidemia; pancreatitis-associated medications), yielding matched cohorts of 35 099 and 66 880 patients, respectively. Incident AP risk was expressed as adjusted odds ratios (aORs) with 95% confidence intervals (CIs) via conditional logistic regression and time-to-event risk as adjusted hazard ratios (aHRs) with 95% CIs via Cox models with Kaplan–Meier/log-rank analyses.
Results: In the obesity comparison, AP incidence was 0.3% in each cohort; the aOR was 0.76 (95% CI, 0.58–1.00) and the aHR 0.87 (95% CI, 0.67–1.12), with 730-day pancreatitis-free survival of 99.64% versus 99.58% (log-rank p = 0.28). In the T2DM comparison, incidence was 0.5% versus 0.4%; the aOR was 1.14 (95% CI, 0.97–1.35) and the aHR 1.13 (95% CI, 0.96–1.34), with survival of 99.50% versus 99.56% (p = 0.14). No comparison reached statistical significance.
Discussion: Our study limitations include retrospective design, possibility of misclassification bias and confounding by other causes of AP. Despite this, our study did not show any significant difference in incidence of AP across metabolic phenotypes. The data appears to suggest that the causal mechanisms for AP may be independent of the phenotypes. Future studies perhaps with longer follow up are required to corroborate our findings and clarify if GLP1 RA dose and duration, pre-existent cholelithiasis and other factors can predict risk of AP.
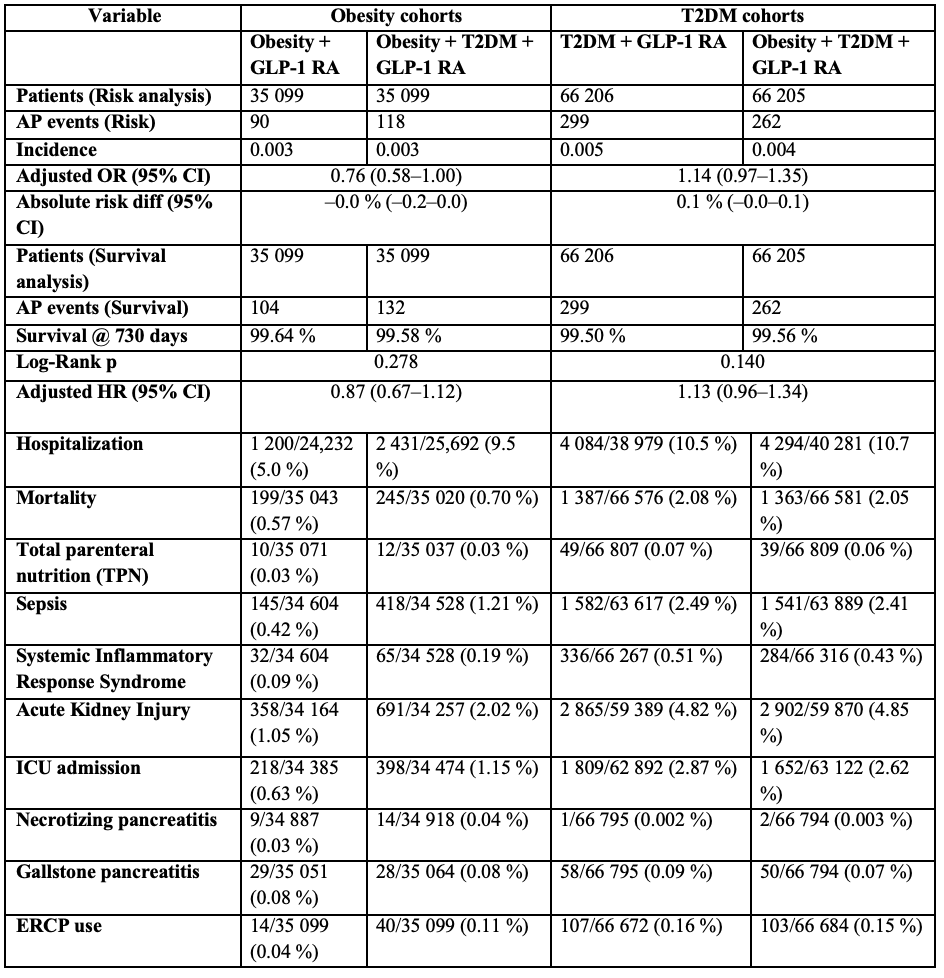
Figure: Table 1. Incidence and adjusted risk of acute pancreatitis and other complications within 730 days of GLP-1 RA initiation across four propensity-matched cohorts (obesity alone, obesity + T2DM, T2DM alone, and obesity + T2DM). Data are presented as n/N (%) for each outcome, with adjusted odds ratios (ORs) and hazard ratios (HRs) with 95% confidence intervals for acute pancreatitis.
Disclosures:
Ruchir Paladiya indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Murali Dharan indicated no relevant financial relationships.
Ruchir Paladiya, MBBS1, Himsikhar Khataniar, MD2, Karthik Mathialagan, MD3, Murali Dharan, 4. P2206 - Incidence of Acute Pancreatitis With GLP-1 Receptor Agonists (GLP-1 RA) Use Across Obesity and Type 2 Diabetes Phenotypes: A Multi-Center Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
