Monday Poster Session
Category: Biliary/Pancreas
P2205 - Severity of Thrombocytopenia Appears to Correlate With Risk of Bacteremic Cholangitis: Results From a Single Center Retrospective Study
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ruchir Paladiya, MBBS
University of Connecticut School of Medicine
Farmington, CT
Presenting Author(s)
Ruchir Paladiya, MBBS1, Karthik Mathialagan, MD2, Murali Dharan, 3
1University of Connecticut School of Medicine, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Employed, Farmington, CT
Introduction: Bacteremic cholangitis (BC) has been associated with increased morbidity and mortality.1 Thrombocytopenia (TCP) appears to be an independent risk factor for bacteremia.1 However its prognostic significance in identifying bacteremia remains underexplored. We sought to characterize the relationship between platelet count and bacteremia among patients hospitalized with acute cholangitis (AC).
Methods: We performed a retrospective cohort analysis identifying all adult inpatients diagnosed with AC between May 2020 and May 2025 at our medical center. Patients were stratified by the lowest platelet count range during hospitalization: < 50, 50–99, 100–149, and ≥150 × 10⁹/L. The primary outcome was the presence of bacteremia, defined by positive blood culture during admission. The absolute risk, risk ratio (RR), odds ratio (OR), absolute risk difference, and number needed to harm (NNH) for bacteremia across platelet count thresholds were calculated and a CAT test for linear association was performed.
Results: Out of 459 patients diagnosed with AC, 181 (39.4%) had TCP (< 150) and 278 (60.6%) had normal platelet counts. Bacteremia was diagnosed in 29.8% of patients with TCP compared to 8.6% with normal platelet count (RR 3.46 [95% CI: 2.22–5.38]; OR 4.50 [95% CI: 2.66–7.61]). The comparative analysis of bacteremia risk across platelet thresholds is shown in Figure 1. The CAT test confirmed a significant linear association between severity of TCP and increased bacteremia risk (p < 0.00000001). Dose-response analysis demonstrated a marked increase in bacteremia rates with progressive TCP across all thresholds.
Discussion: Limitations of our study include retrospective design and inability to adjust for confounding factors that can be associated with TCP. Despite these limitations, our study appears to suggest a linear correlation between severity of TCP and risk of BC. As blood cultures usually take up to 48 hours to result, down trending platelet counts could be an important prognostic indicator to assess the risk of BC and drive clinical decision-making regarding the timing of intervention, especially as studies having shown that timing of ERCP impacts outcomes in BC. 2
References:
1. Ruchir Paladiya, Murali Dharan. Clinical Predictors of Bacteremic Cholangitis patients: Results from a NIS data (2016 - 2020) based study. ACG 2024
2. Ruchir Paladiya, Murali Dharan. Timing of ERCP impacts outcomes in Bacteremic Cholangitis (BC) - Results from a Nationwide Analysis. DDW 2025
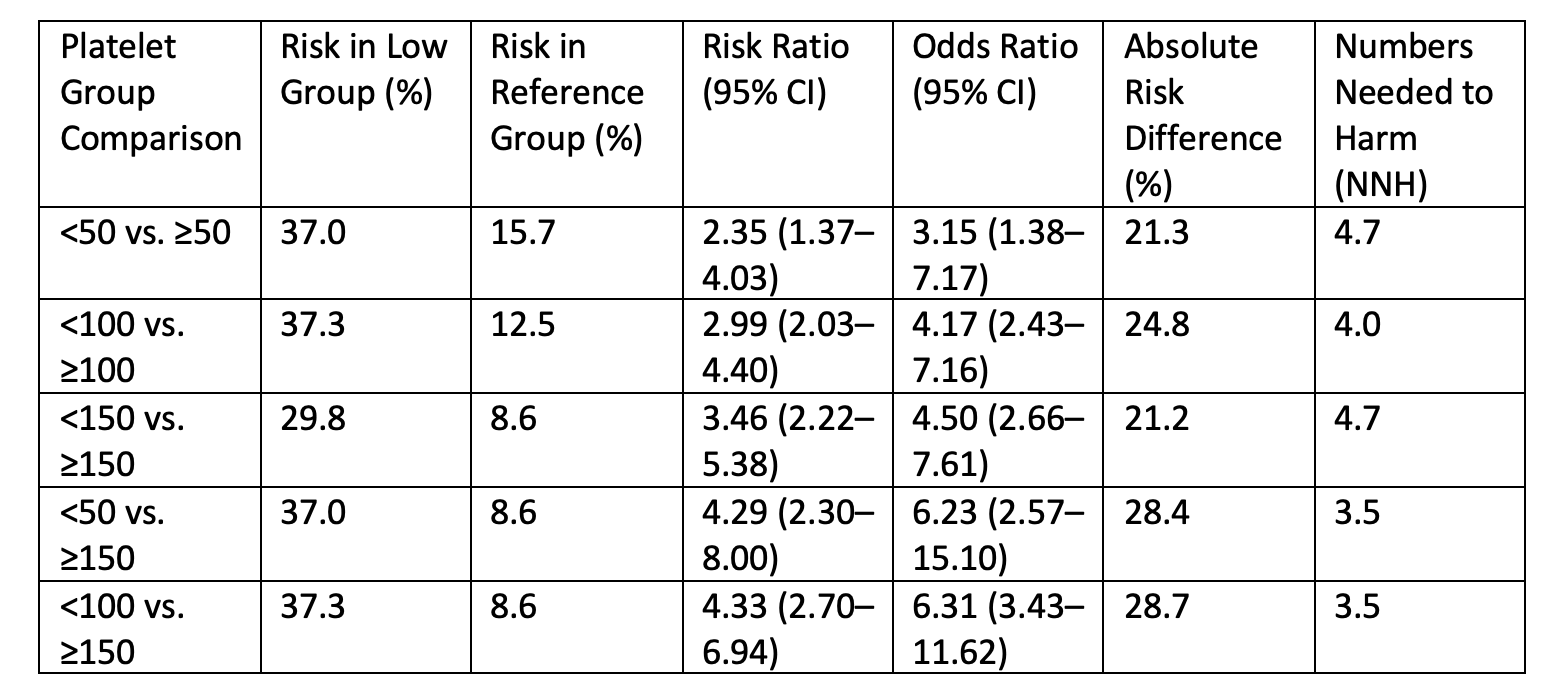
Figure: Figure 1. Comparative analysis of bacteremia risk across platelet thresholds in patients with acute cholangitis.
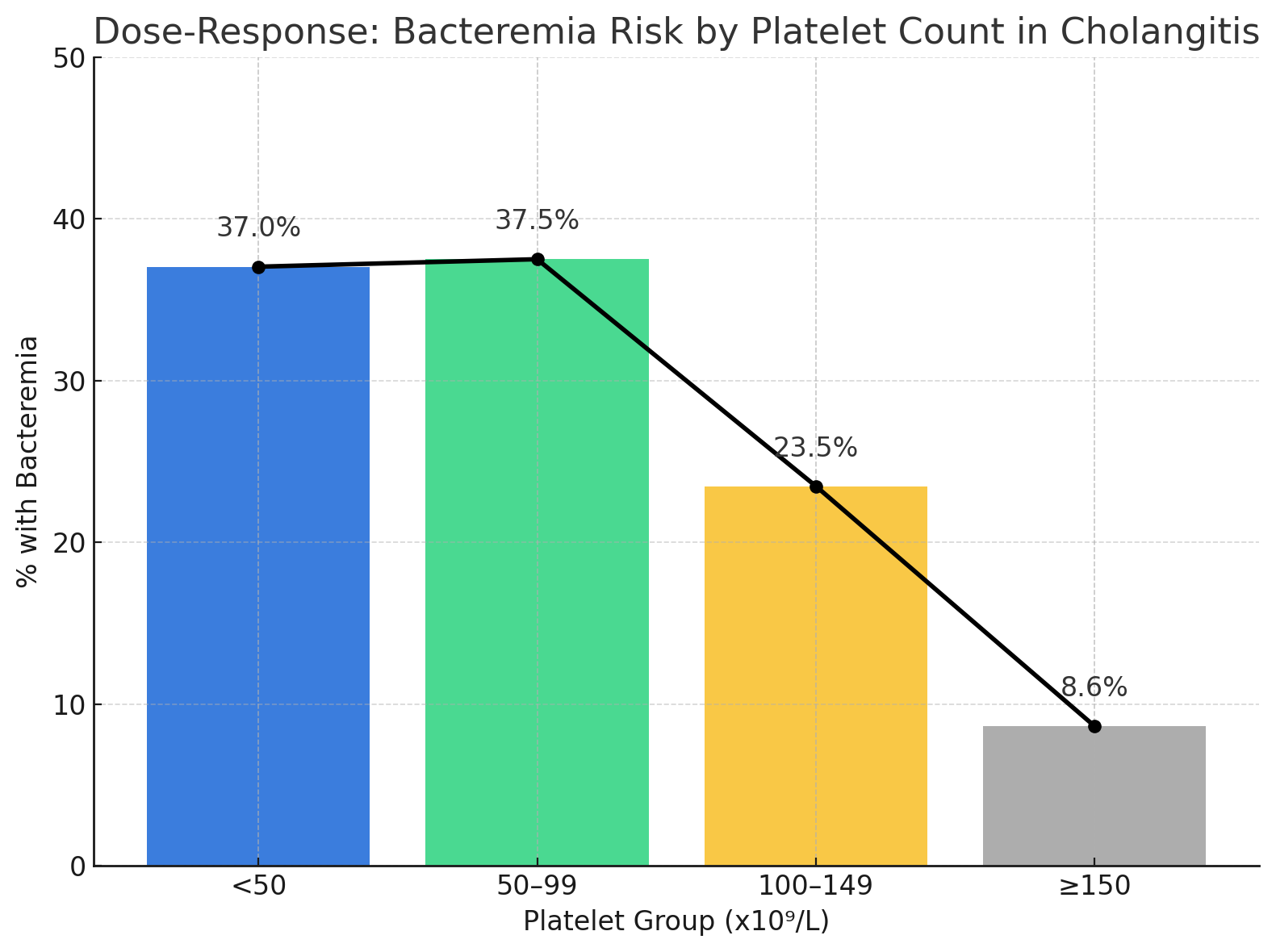
Figure: Figure 2. Dose-response relationship between platelet count and risk of bacteremia among patients hospitalized with acute cholangitis. The plot displays the percentage of patients with bacteremia within each platelet group: <50, 50–99, 100–149, and ≥150 × 10⁹/L. A marked increase in bacteremia risk was observed with progressively lower platelet counts, demonstrating a clear dose-response effect. Bar heights represent observed proportions, and data labels indicate the exact percentages for each group.
Disclosures:
Ruchir Paladiya indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Murali Dharan indicated no relevant financial relationships.
Ruchir Paladiya, MBBS1, Karthik Mathialagan, MD2, Murali Dharan, 3. P2205 - Severity of Thrombocytopenia Appears to Correlate With Risk of Bacteremic Cholangitis: Results From a Single Center Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut School of Medicine, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Employed, Farmington, CT
Introduction: Bacteremic cholangitis (BC) has been associated with increased morbidity and mortality.1 Thrombocytopenia (TCP) appears to be an independent risk factor for bacteremia.1 However its prognostic significance in identifying bacteremia remains underexplored. We sought to characterize the relationship between platelet count and bacteremia among patients hospitalized with acute cholangitis (AC).
Methods: We performed a retrospective cohort analysis identifying all adult inpatients diagnosed with AC between May 2020 and May 2025 at our medical center. Patients were stratified by the lowest platelet count range during hospitalization: < 50, 50–99, 100–149, and ≥150 × 10⁹/L. The primary outcome was the presence of bacteremia, defined by positive blood culture during admission. The absolute risk, risk ratio (RR), odds ratio (OR), absolute risk difference, and number needed to harm (NNH) for bacteremia across platelet count thresholds were calculated and a CAT test for linear association was performed.
Results: Out of 459 patients diagnosed with AC, 181 (39.4%) had TCP (< 150) and 278 (60.6%) had normal platelet counts. Bacteremia was diagnosed in 29.8% of patients with TCP compared to 8.6% with normal platelet count (RR 3.46 [95% CI: 2.22–5.38]; OR 4.50 [95% CI: 2.66–7.61]). The comparative analysis of bacteremia risk across platelet thresholds is shown in Figure 1. The CAT test confirmed a significant linear association between severity of TCP and increased bacteremia risk (p < 0.00000001). Dose-response analysis demonstrated a marked increase in bacteremia rates with progressive TCP across all thresholds.
Discussion: Limitations of our study include retrospective design and inability to adjust for confounding factors that can be associated with TCP. Despite these limitations, our study appears to suggest a linear correlation between severity of TCP and risk of BC. As blood cultures usually take up to 48 hours to result, down trending platelet counts could be an important prognostic indicator to assess the risk of BC and drive clinical decision-making regarding the timing of intervention, especially as studies having shown that timing of ERCP impacts outcomes in BC. 2
References:
1. Ruchir Paladiya, Murali Dharan. Clinical Predictors of Bacteremic Cholangitis patients: Results from a NIS data (2016 - 2020) based study. ACG 2024
2. Ruchir Paladiya, Murali Dharan. Timing of ERCP impacts outcomes in Bacteremic Cholangitis (BC) - Results from a Nationwide Analysis. DDW 2025
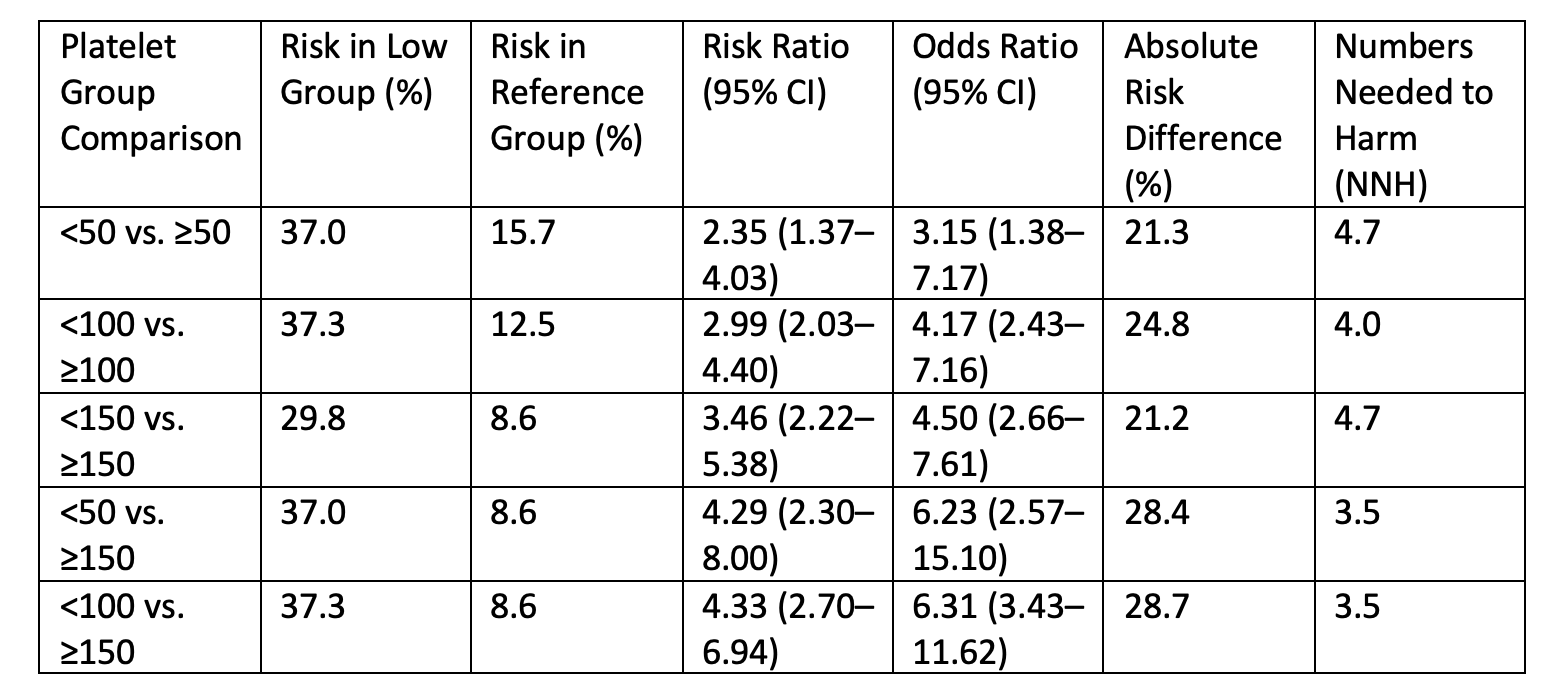
Figure: Figure 1. Comparative analysis of bacteremia risk across platelet thresholds in patients with acute cholangitis.
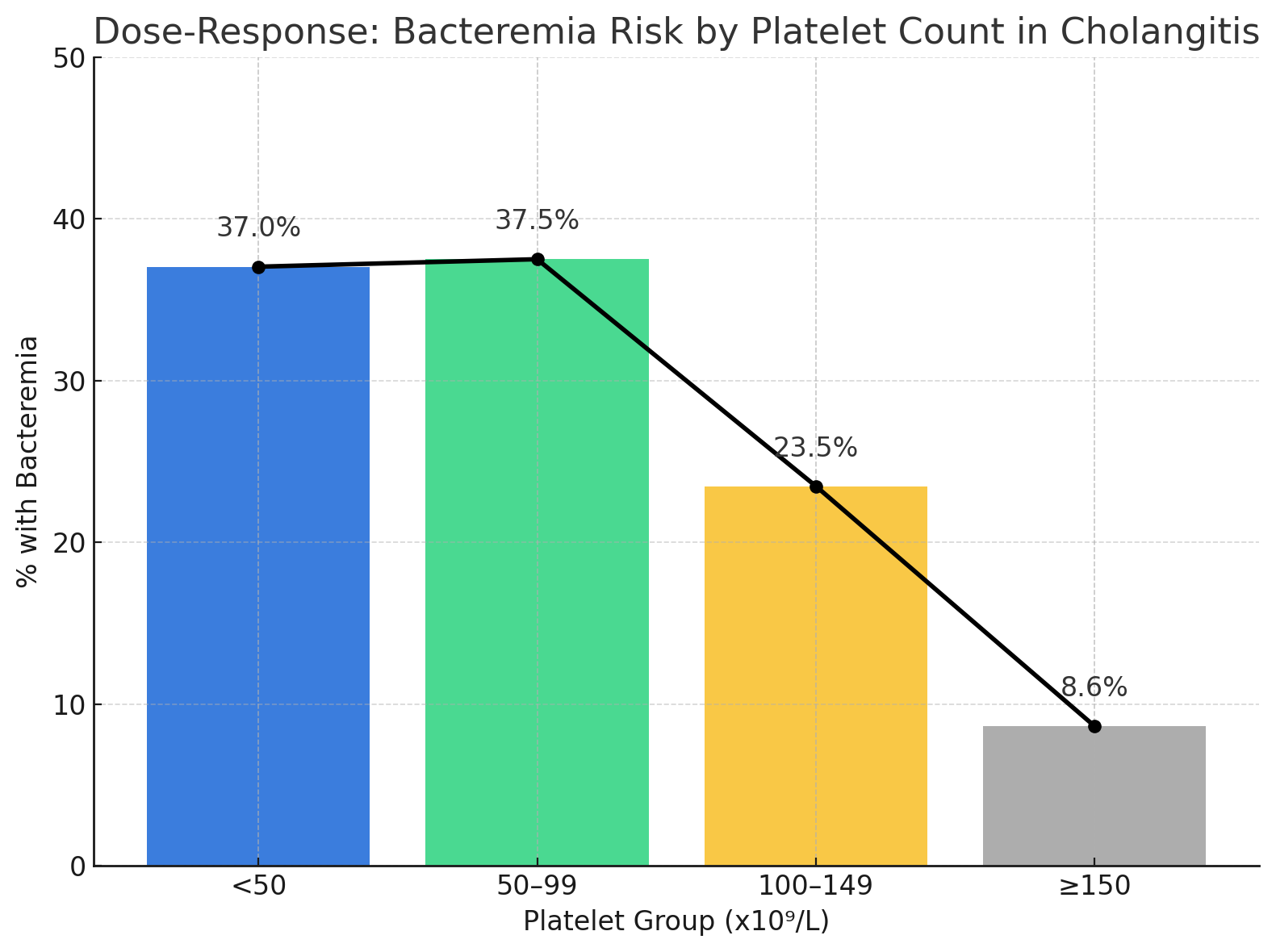
Figure: Figure 2. Dose-response relationship between platelet count and risk of bacteremia among patients hospitalized with acute cholangitis. The plot displays the percentage of patients with bacteremia within each platelet group: <50, 50–99, 100–149, and ≥150 × 10⁹/L. A marked increase in bacteremia risk was observed with progressively lower platelet counts, demonstrating a clear dose-response effect. Bar heights represent observed proportions, and data labels indicate the exact percentages for each group.
Disclosures:
Ruchir Paladiya indicated no relevant financial relationships.
Karthik Mathialagan indicated no relevant financial relationships.
Murali Dharan indicated no relevant financial relationships.
Ruchir Paladiya, MBBS1, Karthik Mathialagan, MD2, Murali Dharan, 3. P2205 - Severity of Thrombocytopenia Appears to Correlate With Risk of Bacteremic Cholangitis: Results From a Single Center Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
