Monday Poster Session
Category: Biliary/Pancreas
P2203 - Optimizing Emergency Department Discharge for Acute Pancreatitis Using Machine Learning
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Cameron M. Quon, MD
University of Southern California
Los Angeles, CA
Presenting Author(s)
Cameron M. Quon, MD1, Daniel Wang, MD2, Paul Yoon, MD1, Helen Lee, FNP1, Sunil Sheth, MD3, James L. Buxbaum, MD1
1University of Southern California, Los Angeles, CA; 2University of Southern California, Torrance, CA; 3Beth Israel Deaconess Medical Center, Harvard Medical School, Bostom, MA
Introduction: Acute pancreatitis is a leading cause of admission for gastrointestinal disease and is increasing in incidence.1 While one-third of patients suffer considerable morbidity, the majority have uneventful courses with rapid recovery.1 There are clinical tools to stratify disease severity like the Ranson score, Bedside Index for Severity in Acute Pancreatitis (BISAP), and Revised Atlanta Classification (RAC).2 However, few models address emergency room disposition.
A recent study showed early safe emergency department (ED) discharge for mild acute pancreatitis patients with age < 50, a Charlson Comorbidity Index < 2, and idiopathic etiology.3
The goal of this study is to build upon these safe discharge criteria using a machine learning model to identify additional optimal predictors.
Methods: We analyzed an extensively characterized cohort of 896 patients who presented to an urban safety-net teaching hospital between 2015 to 2022.
First, we validated the original model using our cohort where a safe discharge was defined as meeting the criteria from the original study.
Next, we trained a gradient-boosted machine learning model (XGBoost) using 76 predictors including demographics, comorbidities, initial lab values, triage vitals, and etiology. We evaluated performance with stratified 5-fold cross-validation. Predictive performance was assessed using area under the receiver operating characteristic curve (AUC). The top ten influential predictors were identified using Shapley Additive exPlanations (SHAP).
Results: Only 12.5% of patients in our cohort met eligibility compared to 26% in the original study (p < 0.0001). Those who met criteria had similar readmission rates (10.7% versus 12%, p=0.785). Those who did not meet criteria also had similar readmission rates (11.7% versus 13.3%, p=0.216).
Our machine learning model had high predictive accuracy (UAC ≈ 0.95) (Figure 1). The most influential features included age, etiology, triglycerides, white blood cell count, cholesterol, oral morphine equivalents, blood pressure, and glucose (Figure 2).
Discussion: Our revised model potentially improves existing discharge criteria from the ED for patients with acute pancreatitis. By identifying other high-yield predictors while maintaining safety, our model may further reduce unnecessary admissions.
References
1. Guilabert L, et al. Gastroenterol Clin North Am. 2025;54(1):21-36.
2. Capurso G, et al. United European Gastroenterol J. 2023;11(9):825-36.
3. Anderson K, et al. Pancreatology. 2023;23(3):299-305.
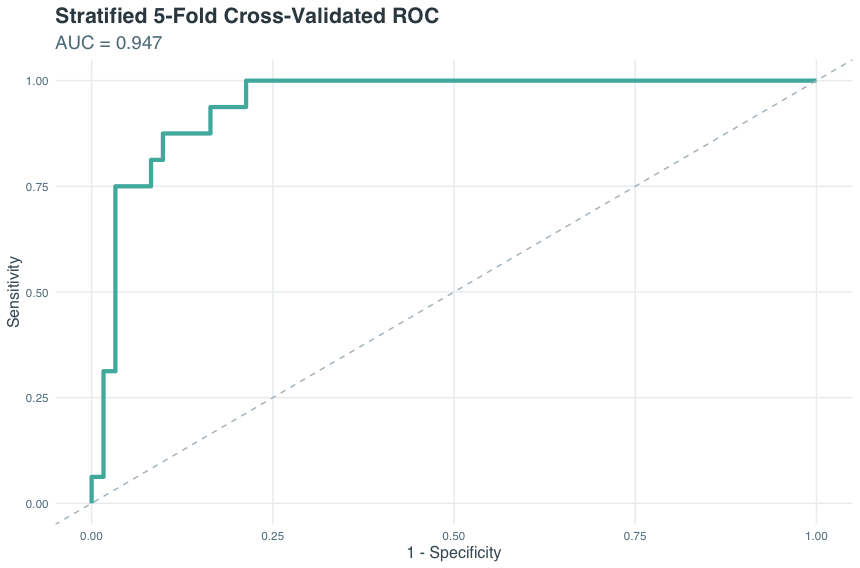
Figure: ROC curve from a stratified 5-fold cross-validated XGBoost model predicting safe discharge eligibility from the ED in acute pancreatitis with an AUC of 0.947
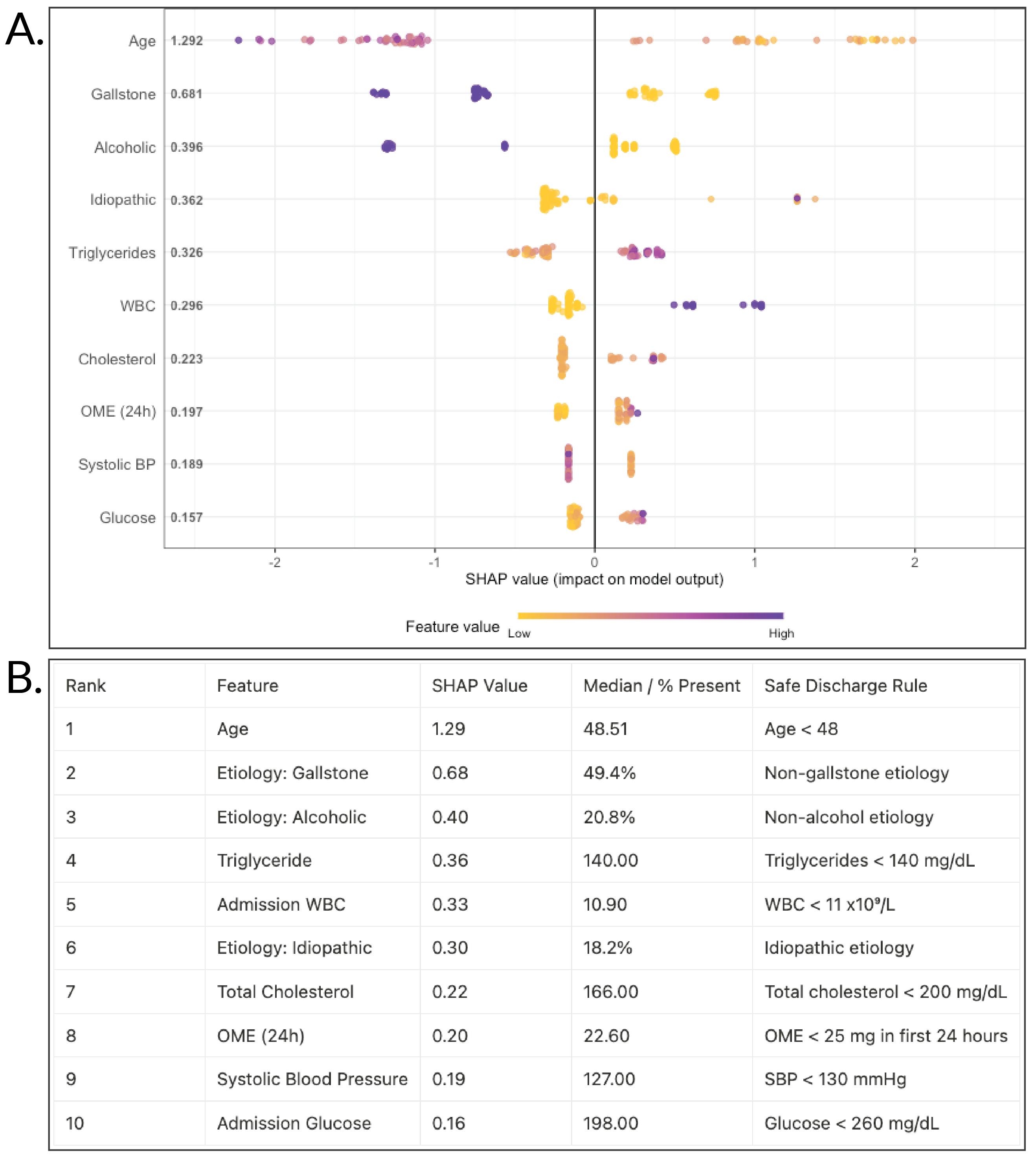
Figure: A. Top 10 predictors of safe discharge eligibility for acute pancreatitis based on SHAP values from the XGBoost model. B. Proposed clinical thresholds as discharge rules.
Disclosures:
Cameron Quon indicated no relevant financial relationships.
Daniel Wang indicated no relevant financial relationships.
Paul Yoon indicated no relevant financial relationships.
Helen Lee indicated no relevant financial relationships.
Sunil Sheth indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
Cameron M. Quon, MD1, Daniel Wang, MD2, Paul Yoon, MD1, Helen Lee, FNP1, Sunil Sheth, MD3, James L. Buxbaum, MD1. P2203 - Optimizing Emergency Department Discharge for Acute Pancreatitis Using Machine Learning, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Southern California, Los Angeles, CA; 2University of Southern California, Torrance, CA; 3Beth Israel Deaconess Medical Center, Harvard Medical School, Bostom, MA
Introduction: Acute pancreatitis is a leading cause of admission for gastrointestinal disease and is increasing in incidence.1 While one-third of patients suffer considerable morbidity, the majority have uneventful courses with rapid recovery.1 There are clinical tools to stratify disease severity like the Ranson score, Bedside Index for Severity in Acute Pancreatitis (BISAP), and Revised Atlanta Classification (RAC).2 However, few models address emergency room disposition.
A recent study showed early safe emergency department (ED) discharge for mild acute pancreatitis patients with age < 50, a Charlson Comorbidity Index < 2, and idiopathic etiology.3
The goal of this study is to build upon these safe discharge criteria using a machine learning model to identify additional optimal predictors.
Methods: We analyzed an extensively characterized cohort of 896 patients who presented to an urban safety-net teaching hospital between 2015 to 2022.
First, we validated the original model using our cohort where a safe discharge was defined as meeting the criteria from the original study.
Next, we trained a gradient-boosted machine learning model (XGBoost) using 76 predictors including demographics, comorbidities, initial lab values, triage vitals, and etiology. We evaluated performance with stratified 5-fold cross-validation. Predictive performance was assessed using area under the receiver operating characteristic curve (AUC). The top ten influential predictors were identified using Shapley Additive exPlanations (SHAP).
Results: Only 12.5% of patients in our cohort met eligibility compared to 26% in the original study (p < 0.0001). Those who met criteria had similar readmission rates (10.7% versus 12%, p=0.785). Those who did not meet criteria also had similar readmission rates (11.7% versus 13.3%, p=0.216).
Our machine learning model had high predictive accuracy (UAC ≈ 0.95) (Figure 1). The most influential features included age, etiology, triglycerides, white blood cell count, cholesterol, oral morphine equivalents, blood pressure, and glucose (Figure 2).
Discussion: Our revised model potentially improves existing discharge criteria from the ED for patients with acute pancreatitis. By identifying other high-yield predictors while maintaining safety, our model may further reduce unnecessary admissions.
References
1. Guilabert L, et al. Gastroenterol Clin North Am. 2025;54(1):21-36.
2. Capurso G, et al. United European Gastroenterol J. 2023;11(9):825-36.
3. Anderson K, et al. Pancreatology. 2023;23(3):299-305.
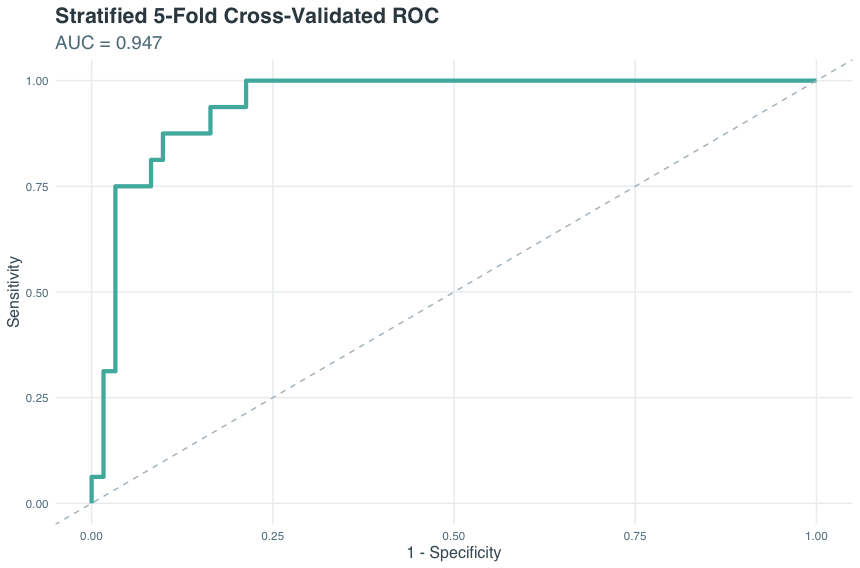
Figure: ROC curve from a stratified 5-fold cross-validated XGBoost model predicting safe discharge eligibility from the ED in acute pancreatitis with an AUC of 0.947
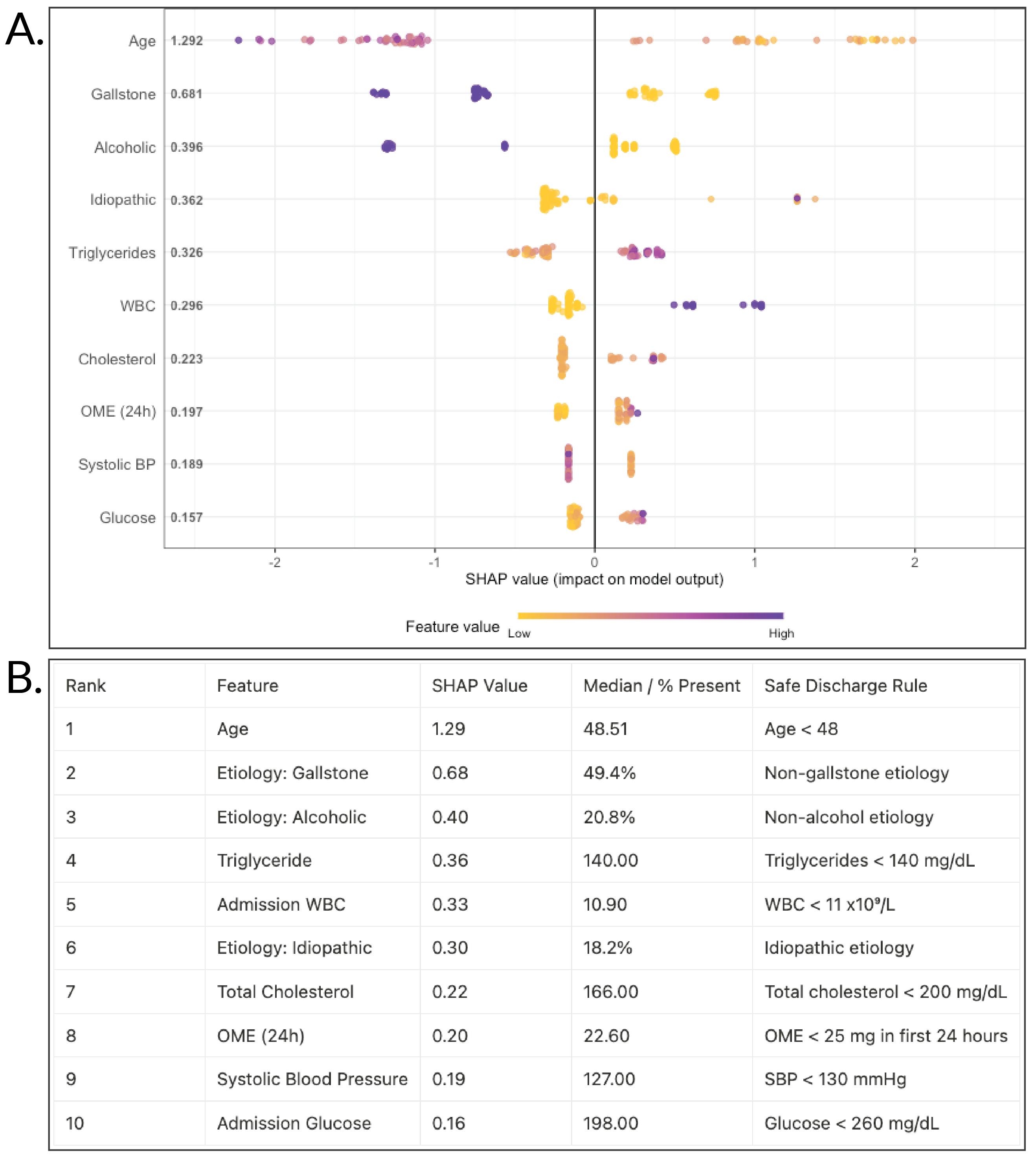
Figure: A. Top 10 predictors of safe discharge eligibility for acute pancreatitis based on SHAP values from the XGBoost model. B. Proposed clinical thresholds as discharge rules.
Disclosures:
Cameron Quon indicated no relevant financial relationships.
Daniel Wang indicated no relevant financial relationships.
Paul Yoon indicated no relevant financial relationships.
Helen Lee indicated no relevant financial relationships.
Sunil Sheth indicated no relevant financial relationships.
James Buxbaum: Boston Scientific – Consultant. Olympus – Consultant.
Cameron M. Quon, MD1, Daniel Wang, MD2, Paul Yoon, MD1, Helen Lee, FNP1, Sunil Sheth, MD3, James L. Buxbaum, MD1. P2203 - Optimizing Emergency Department Discharge for Acute Pancreatitis Using Machine Learning, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
