Monday Poster Session
Category: Biliary/Pancreas
P2197 - Trends and Outcomes of Alcoholic Acute Pancreatitis in Patients With Alcohol Use Disorder Treated With Naltrexone in the United States: Before and After the COVID-19 Pandemic
Monday, October 27, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Alexander Malik, MD
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Thai Hau Koo, MD1, Alexander Malik, MD2, Mohamed Zayed Sheriff, MD3, Rishi Chowdhary, MD2, Adrian Lindsey, MD4
1University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3Cleveland VA Hospital Systems, Cleveland, OH; 4MetroHealth Medical Center, Cleveland, OH
Introduction: Alcohol use disorder (AUD) is a well-established risk factor for alcoholic acute pancreatitis (AAP). While medication for AUD (MAUD) use has been used for alcohol-associated liver disease, its application in AAP remains unclear. We aimed to assess the temporal trends in AAP incidence and the impact of naltrexone use on clinical outcomes in AUD patients.
Methods: We conducted a retrospective cohort study using de-identified patient data from the TriNetX database, including all adults (≥18 years) diagnosed with AUD. AAP patients were then identified and stratified by naltrexone exposure. The incidence and prevalence of AAP in AUD patients were assessed pre- (March 2015-2019) and post-COVID-19 (March 2020-2025). Baseline characteristics were compared between patients treated and those not treated with naltrexone. Propensity score matching (PSM) was performed to adjust for confounders. The primary outcomes included mortality, chronic pancreatitis, alcoholic hepatitis, cirrhosis, hospital readmission, and emergency department (ED) visits at 1, 6, and 12 months.
Results: Among 1,331,338 adults with AUD, 33,561 (2.52%) developed AAP. The incidence of AAPs increased significantly following the COVID-19 pandemic (1.42% pre-pandemic vs. 1.98% post-pandemic), with the largest relative rise among younger adults (18–34 years), women, and racial minorities. Of those with AAP, 1,871 (5.6%) received naltrexone. Compared with patients with AAP not treated with naltrexone, those receiving naltrexone were younger (46.1 vs. 50.8 years, p< 0.0001), more likely to be Hispanic (14% vs. 9%, p< 0.0001), and had higher rates of coexisting anxiety (66% vs. 44%) and mood disorders (63% vs. 43%, both p< 0.0001). Following PSM, naltrexone use was associated with significantly lower odds of mortality at 1 (OR 0.274, 95% CI, 0.136–0.554; p< 0.0001) and 6 months (OR 0.571, p=0.005), with a non-significant trend at 12 months (OR 0.785, p=0.141). Reduced odds were also observed for alcoholic hepatitis at one month (OR 0.561, p< 0.0001) and hospital readmissions across all time points (ORs 0.304–0.488, all p< 0.0001). Surprisingly, naltrexone use was associated with an increased risk of ED visits after matching.
Discussion: Naltrexone use has been associated with improved short-term mortality and lower risk of hospital readmission. These findings support expanding MAUD use in AAP population, a group that may benefit from the therapeutic and harm reduction benefits of MAUD treatment.
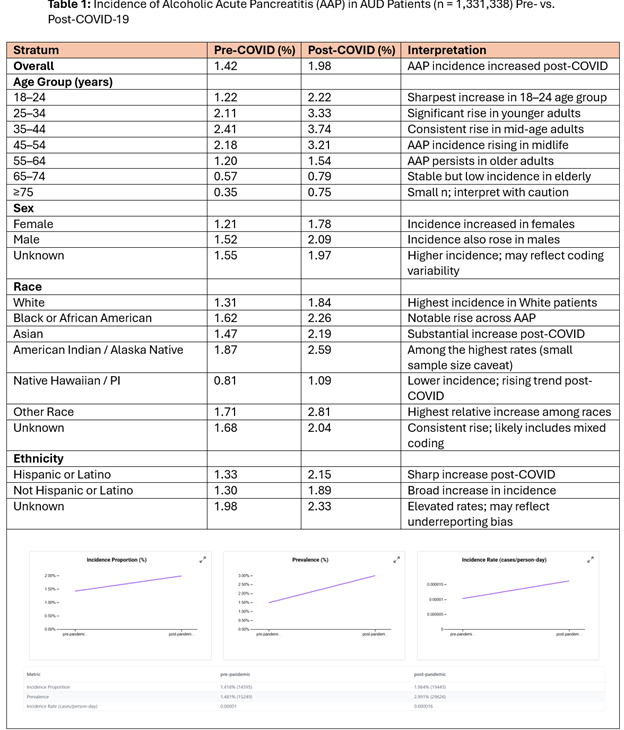
Figure: Table 1: Incidence of Alcoholic Acute Pancreatitis (AAP) in AUD Patients (n = 1,331,338) Pre- vs. Post-COVID-19
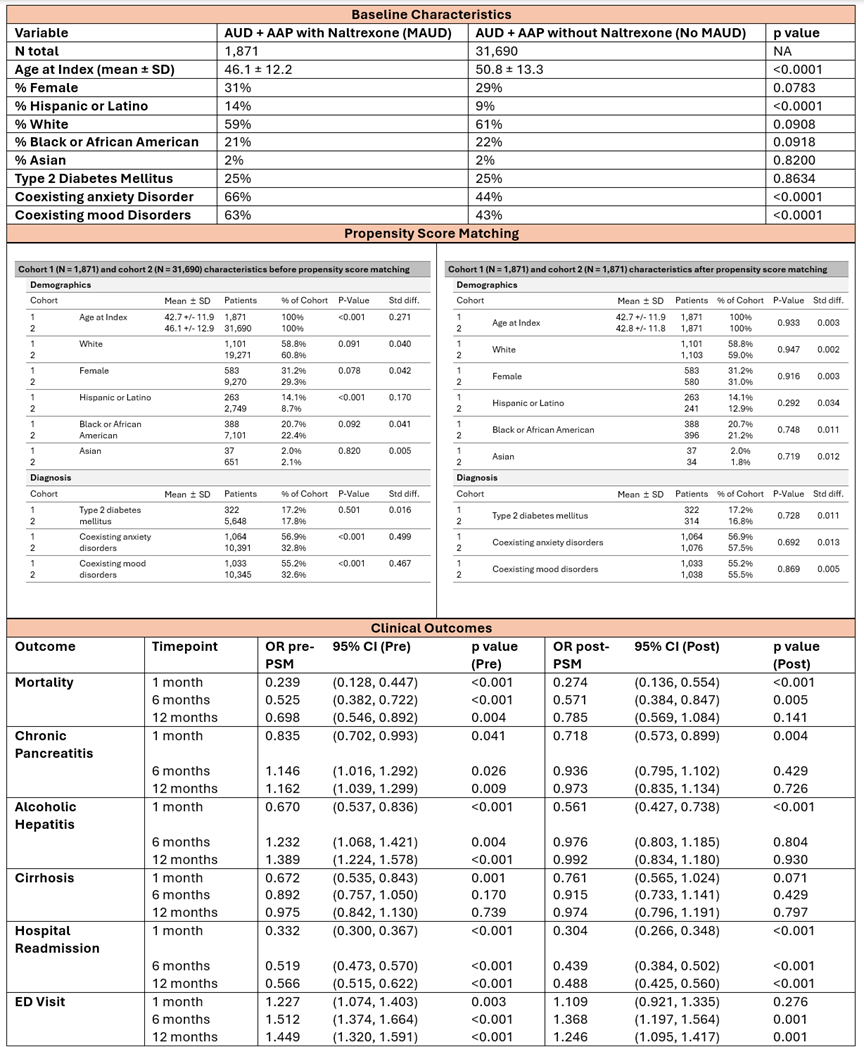
Figure: Table 2: Baseline characteristics, propensity score matching, and clinical outcomes of AUD Patients with AAP — With vs. Without Naltrexone (MAUD)
Disclosures:
Thai Hau Koo indicated no relevant financial relationships.
Alexander Malik indicated no relevant financial relationships.
Mohamed Zayed Sheriff indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Adrian Lindsey indicated no relevant financial relationships.
Thai Hau Koo, MD1, Alexander Malik, MD2, Mohamed Zayed Sheriff, MD3, Rishi Chowdhary, MD2, Adrian Lindsey, MD4. P2197 - Trends and Outcomes of Alcoholic Acute Pancreatitis in Patients With Alcohol Use Disorder Treated With Naltrexone in the United States: Before and After the COVID-19 Pandemic, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 2Case Western Reserve University / MetroHealth, Cleveland, OH; 3Cleveland VA Hospital Systems, Cleveland, OH; 4MetroHealth Medical Center, Cleveland, OH
Introduction: Alcohol use disorder (AUD) is a well-established risk factor for alcoholic acute pancreatitis (AAP). While medication for AUD (MAUD) use has been used for alcohol-associated liver disease, its application in AAP remains unclear. We aimed to assess the temporal trends in AAP incidence and the impact of naltrexone use on clinical outcomes in AUD patients.
Methods: We conducted a retrospective cohort study using de-identified patient data from the TriNetX database, including all adults (≥18 years) diagnosed with AUD. AAP patients were then identified and stratified by naltrexone exposure. The incidence and prevalence of AAP in AUD patients were assessed pre- (March 2015-2019) and post-COVID-19 (March 2020-2025). Baseline characteristics were compared between patients treated and those not treated with naltrexone. Propensity score matching (PSM) was performed to adjust for confounders. The primary outcomes included mortality, chronic pancreatitis, alcoholic hepatitis, cirrhosis, hospital readmission, and emergency department (ED) visits at 1, 6, and 12 months.
Results: Among 1,331,338 adults with AUD, 33,561 (2.52%) developed AAP. The incidence of AAPs increased significantly following the COVID-19 pandemic (1.42% pre-pandemic vs. 1.98% post-pandemic), with the largest relative rise among younger adults (18–34 years), women, and racial minorities. Of those with AAP, 1,871 (5.6%) received naltrexone. Compared with patients with AAP not treated with naltrexone, those receiving naltrexone were younger (46.1 vs. 50.8 years, p< 0.0001), more likely to be Hispanic (14% vs. 9%, p< 0.0001), and had higher rates of coexisting anxiety (66% vs. 44%) and mood disorders (63% vs. 43%, both p< 0.0001). Following PSM, naltrexone use was associated with significantly lower odds of mortality at 1 (OR 0.274, 95% CI, 0.136–0.554; p< 0.0001) and 6 months (OR 0.571, p=0.005), with a non-significant trend at 12 months (OR 0.785, p=0.141). Reduced odds were also observed for alcoholic hepatitis at one month (OR 0.561, p< 0.0001) and hospital readmissions across all time points (ORs 0.304–0.488, all p< 0.0001). Surprisingly, naltrexone use was associated with an increased risk of ED visits after matching.
Discussion: Naltrexone use has been associated with improved short-term mortality and lower risk of hospital readmission. These findings support expanding MAUD use in AAP population, a group that may benefit from the therapeutic and harm reduction benefits of MAUD treatment.
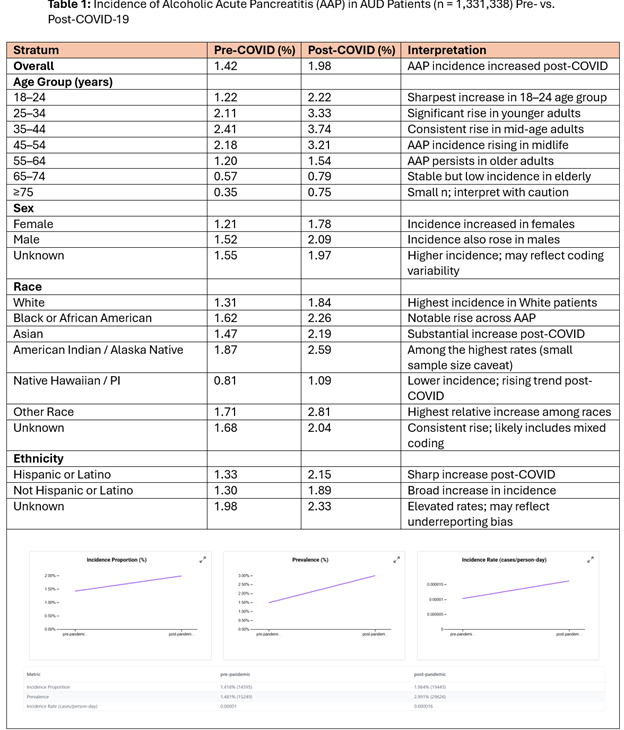
Figure: Table 1: Incidence of Alcoholic Acute Pancreatitis (AAP) in AUD Patients (n = 1,331,338) Pre- vs. Post-COVID-19
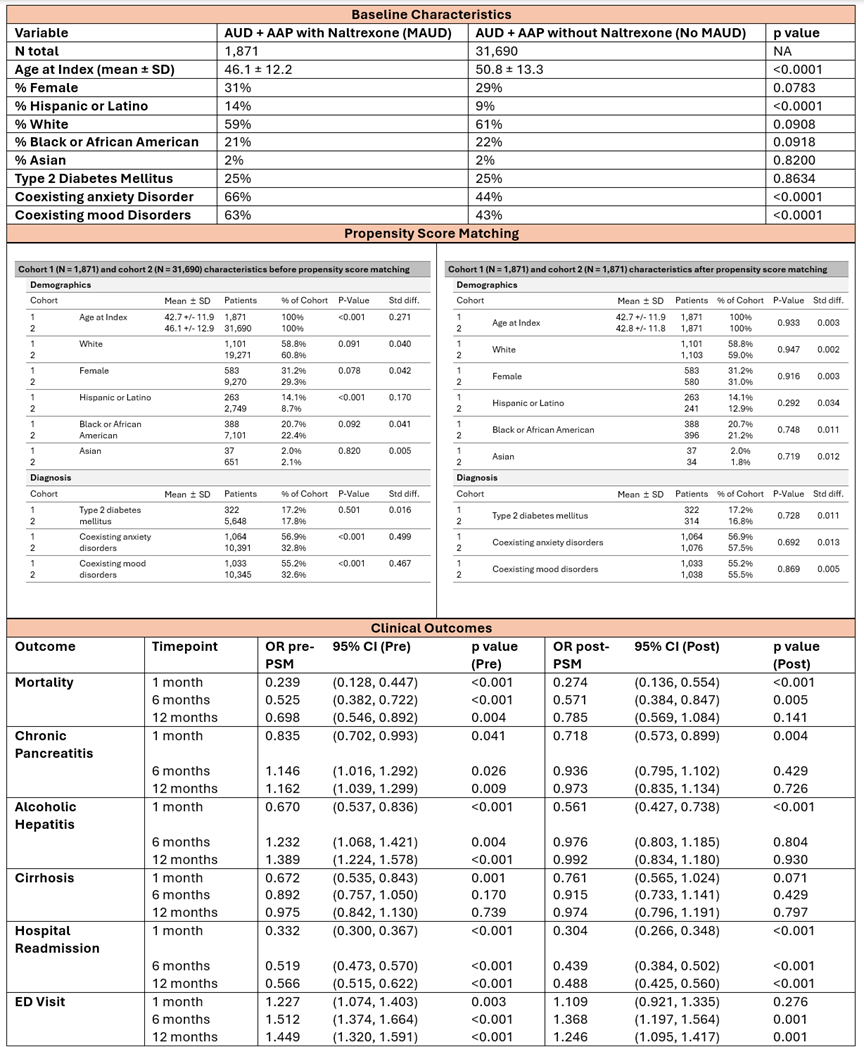
Figure: Table 2: Baseline characteristics, propensity score matching, and clinical outcomes of AUD Patients with AAP — With vs. Without Naltrexone (MAUD)
Disclosures:
Thai Hau Koo indicated no relevant financial relationships.
Alexander Malik indicated no relevant financial relationships.
Mohamed Zayed Sheriff indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Adrian Lindsey indicated no relevant financial relationships.
Thai Hau Koo, MD1, Alexander Malik, MD2, Mohamed Zayed Sheriff, MD3, Rishi Chowdhary, MD2, Adrian Lindsey, MD4. P2197 - Trends and Outcomes of Alcoholic Acute Pancreatitis in Patients With Alcohol Use Disorder Treated With Naltrexone in the United States: Before and After the COVID-19 Pandemic, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
