Tuesday Poster Session
Category: Colon
P4584 - Outcomes of Preoperative Stenting for Right-Sided Malignant Colonic Obstruction: A Nationwide Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Khalid Ahmed, MD (he/him/his)
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Khalid Ahmed, MD1, Zachary Leslie, 2, Yasmin O. Ali, MBBS3, Cyrus Jahansouz, MD1, Eric Wise, MD, MA4, Ahmed Dirweesh, MD5, Stuart K. Amateau, MD, PhD5
1University of Minnesota, Minneapolis, MN; 2UMN, Minneapolis, MN; 3Hennepin Healthcare, Minneapolis, MN; 4University of Minnesota Medical School, Minneapolis, MN; 5University of Minnesota Medical Center, Minneapolis, MN
Introduction: Self-expanding metal stents (SEMS) are commonly used as a bridge to surgery in left-sided malignant colonic obstruction, where they have been shown to reduce ostomy rates. In contrast, their use in right-sided obstruction is infrequent, largely due to technical difficulties and assumptions of lower technical success. However, the literature evaluating SEMS in right-sided disease is limited, and further investigation is warranted. If proven effective, SEMS could support more favorable surgical strategies and potentially reduce the need for staged procedures involving ostomy creation.
Methods: We conducted a retrospective cohort study using the Nationwide Readmissions Database (NRD) from 2016–2022. Adult patients with malignant right-sided colonic obstruction who underwent colectomy were identified via ICD-10 codes and stratified based on receipt of SEMS prior to surgery. Baseline demographics, comorbidities, and outcomes were tabulated. Key endpoints included 90-day mortality, hospital length of stay, and ostomy creation. Adjusted 90-day logistic regression was performed to identify predictors of ostomy creation.
Results: A total of 24,146 patients with right-sided malignant colonic obstruction who underwent colectomy were included; 251 (1.0%) received SEMS prior to surgery. Baseline demographics were similar between groups. The Charlson Comorbidity Index was slightly higher in the stent group (Table 1.). There was no significant difference in 90-day mortality (8.8% vs. 10.1%, p=0.53) or length of stay (8.9 vs. 8.8 days, p=0.89). However, 90-day stoma formation was significantly lower in the stent group (2.0% vs. 9.1%, p< 0.01) (Figure 1). In adjusted 90-day logistic regression, metastatic disease was the strongest predictor of ostomy creation (aOR 2.36, 95% CI: 2.12–2.63; p< 0.05). Stent placement was associated with significantly lower odds for ostomy formation (aOR 0.19 95% CI: 0.07 - 0.5, p< 0.05).
Discussion: SEMS was utilized in only 1.0% of eligible cases, yet its placement prior to right-sided colectomy was associated with a significantly lower rate of ostomy creation without negatively impacting mortality or length of stay. Metastatic disease was a strong predictor of ostomy, underscoring the need for careful patient selection. These findings support the selective use of SEMS as a bridge to surgery in appropriately screened patients with right-sided colonic obstruction. Further prospective studies and randomized controlled trials are warranted to validate these findings.
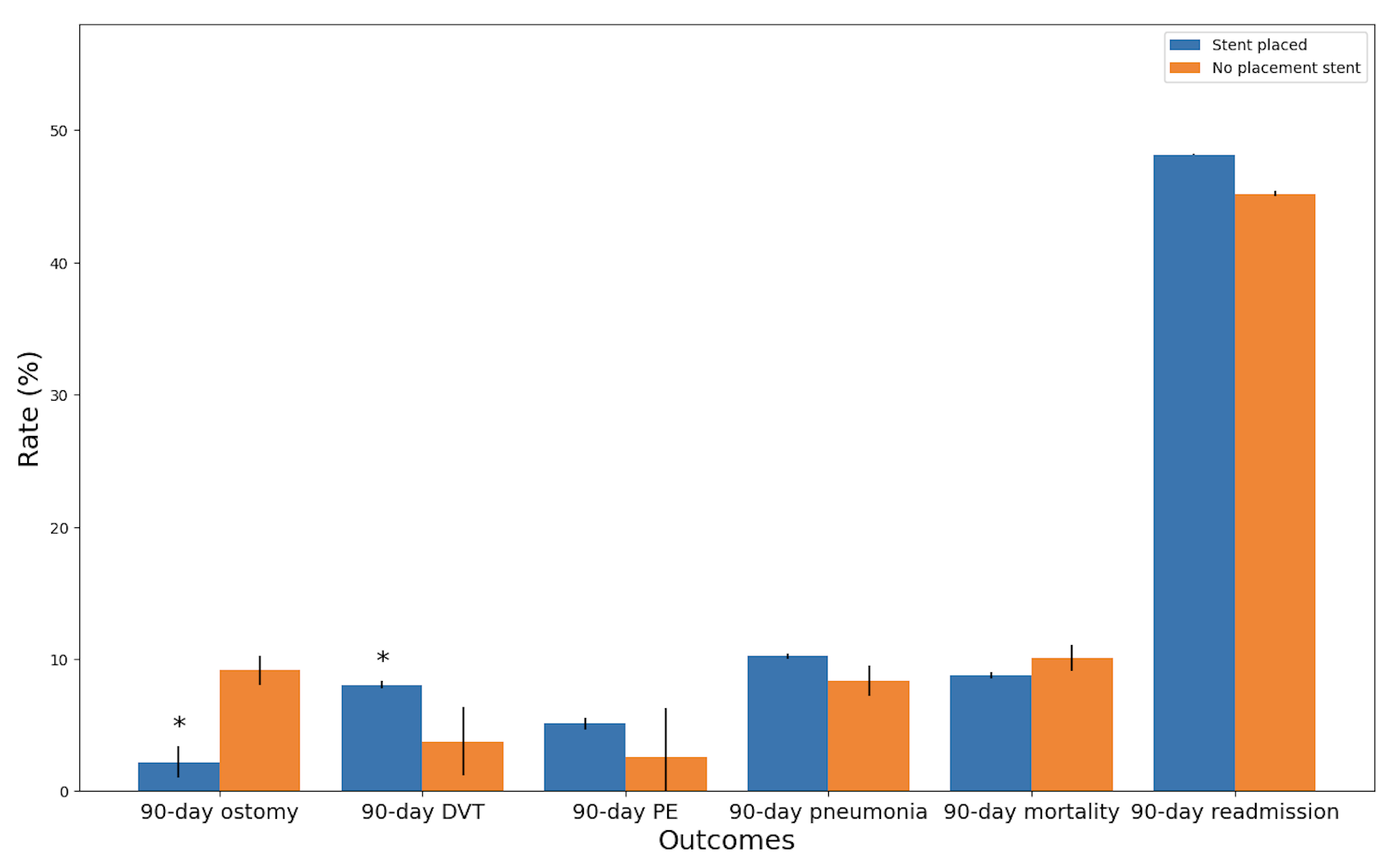
Figure: Table 1. Demographics and outcomes.
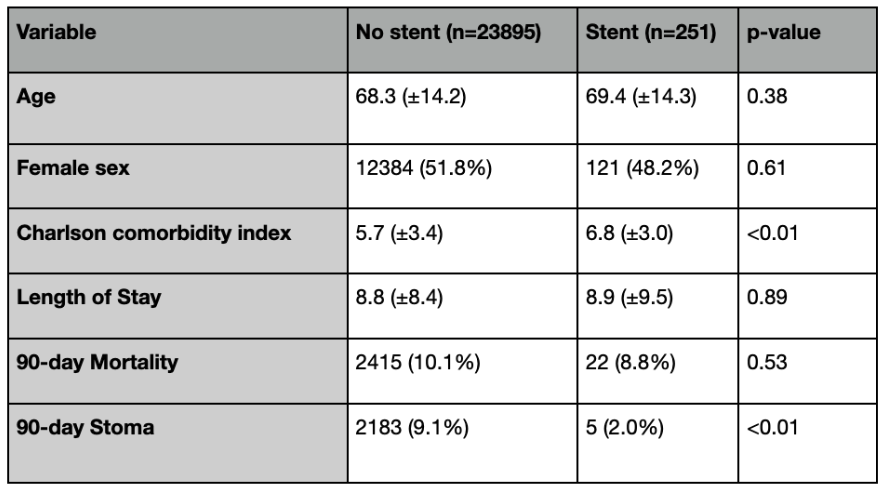
Figure: Figure 1. Comparison of 90-day postoperative outcomes between patients who underwent SEMS placement versus no stent placement prior to colectomy for right-sided malignant colonic obstruction. Asterisks indicate statistically significant differences between groups (p < 0.05).
Disclosures:
Khalid Ahmed indicated no relevant financial relationships.
Zachary Leslie indicated no relevant financial relationships.
Yasmin Ali indicated no relevant financial relationships.
Cyrus Jahansouz indicated no relevant financial relationships.
Eric Wise indicated no relevant financial relationships.
Ahmed Dirweesh indicated no relevant financial relationships.
Stuart Amateau: BSC – Consultant. Cook – Consultant. Endo-Therapeutics – Consultant. Merit – Consultant. Olympus – Advisor or Review Panel Member, Consultant. Provation – Advisory Committee/Board Member. Steris – Consultant.
Khalid Ahmed, MD1, Zachary Leslie, 2, Yasmin O. Ali, MBBS3, Cyrus Jahansouz, MD1, Eric Wise, MD, MA4, Ahmed Dirweesh, MD5, Stuart K. Amateau, MD, PhD5. P4584 - Outcomes of Preoperative Stenting for Right-Sided Malignant Colonic Obstruction: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2UMN, Minneapolis, MN; 3Hennepin Healthcare, Minneapolis, MN; 4University of Minnesota Medical School, Minneapolis, MN; 5University of Minnesota Medical Center, Minneapolis, MN
Introduction: Self-expanding metal stents (SEMS) are commonly used as a bridge to surgery in left-sided malignant colonic obstruction, where they have been shown to reduce ostomy rates. In contrast, their use in right-sided obstruction is infrequent, largely due to technical difficulties and assumptions of lower technical success. However, the literature evaluating SEMS in right-sided disease is limited, and further investigation is warranted. If proven effective, SEMS could support more favorable surgical strategies and potentially reduce the need for staged procedures involving ostomy creation.
Methods: We conducted a retrospective cohort study using the Nationwide Readmissions Database (NRD) from 2016–2022. Adult patients with malignant right-sided colonic obstruction who underwent colectomy were identified via ICD-10 codes and stratified based on receipt of SEMS prior to surgery. Baseline demographics, comorbidities, and outcomes were tabulated. Key endpoints included 90-day mortality, hospital length of stay, and ostomy creation. Adjusted 90-day logistic regression was performed to identify predictors of ostomy creation.
Results: A total of 24,146 patients with right-sided malignant colonic obstruction who underwent colectomy were included; 251 (1.0%) received SEMS prior to surgery. Baseline demographics were similar between groups. The Charlson Comorbidity Index was slightly higher in the stent group (Table 1.). There was no significant difference in 90-day mortality (8.8% vs. 10.1%, p=0.53) or length of stay (8.9 vs. 8.8 days, p=0.89). However, 90-day stoma formation was significantly lower in the stent group (2.0% vs. 9.1%, p< 0.01) (Figure 1). In adjusted 90-day logistic regression, metastatic disease was the strongest predictor of ostomy creation (aOR 2.36, 95% CI: 2.12–2.63; p< 0.05). Stent placement was associated with significantly lower odds for ostomy formation (aOR 0.19 95% CI: 0.07 - 0.5, p< 0.05).
Discussion: SEMS was utilized in only 1.0% of eligible cases, yet its placement prior to right-sided colectomy was associated with a significantly lower rate of ostomy creation without negatively impacting mortality or length of stay. Metastatic disease was a strong predictor of ostomy, underscoring the need for careful patient selection. These findings support the selective use of SEMS as a bridge to surgery in appropriately screened patients with right-sided colonic obstruction. Further prospective studies and randomized controlled trials are warranted to validate these findings.
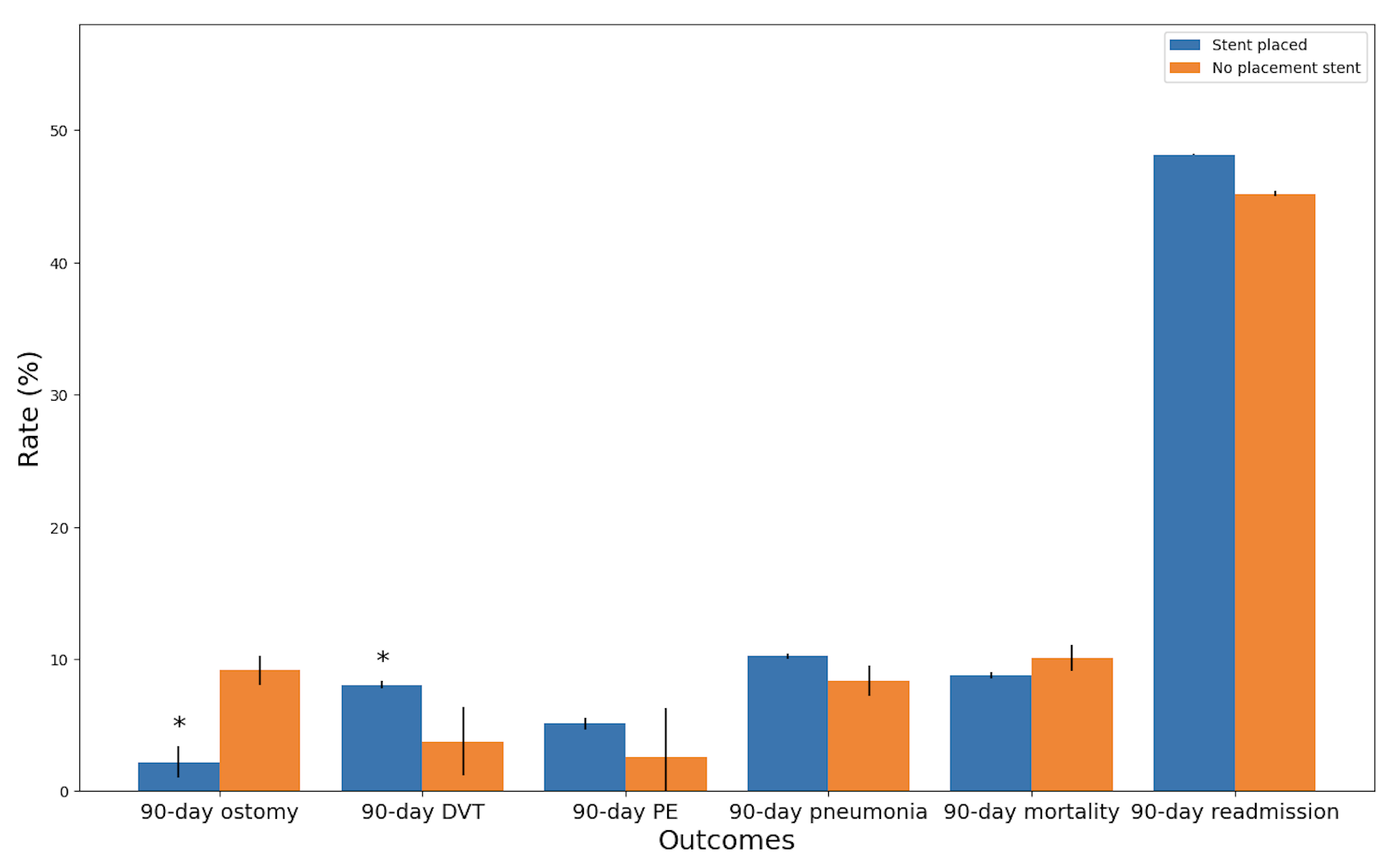
Figure: Table 1. Demographics and outcomes.
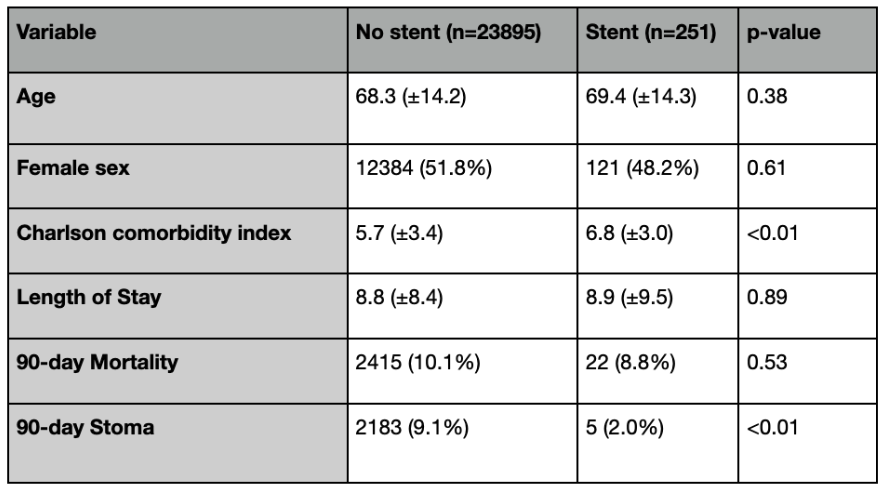
Figure: Figure 1. Comparison of 90-day postoperative outcomes between patients who underwent SEMS placement versus no stent placement prior to colectomy for right-sided malignant colonic obstruction. Asterisks indicate statistically significant differences between groups (p < 0.05).
Disclosures:
Khalid Ahmed indicated no relevant financial relationships.
Zachary Leslie indicated no relevant financial relationships.
Yasmin Ali indicated no relevant financial relationships.
Cyrus Jahansouz indicated no relevant financial relationships.
Eric Wise indicated no relevant financial relationships.
Ahmed Dirweesh indicated no relevant financial relationships.
Stuart Amateau: BSC – Consultant. Cook – Consultant. Endo-Therapeutics – Consultant. Merit – Consultant. Olympus – Advisor or Review Panel Member, Consultant. Provation – Advisory Committee/Board Member. Steris – Consultant.
Khalid Ahmed, MD1, Zachary Leslie, 2, Yasmin O. Ali, MBBS3, Cyrus Jahansouz, MD1, Eric Wise, MD, MA4, Ahmed Dirweesh, MD5, Stuart K. Amateau, MD, PhD5. P4584 - Outcomes of Preoperative Stenting for Right-Sided Malignant Colonic Obstruction: A Nationwide Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
