Tuesday Poster Session
Category: Colon
P4541 - The Impact of Heart Failure on Colorectal Cancer Survival: A Propensity-Matched Cohort and Survival Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Iyad Al-Bustami, MD, MPH (he/him/his)
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Iyad Al-Bustami, MD, MPH1, Sweta Lohani, MD1, Kenan Alrejjal, MBBS2, Kazi Haque, MD3, Aashutosh Sah, MD4, Chaula Desai, MD1, Ammar Yasser. Abdulfattah, MBBCh5, Delwar Khan, MD1, Daniel Low, MD6, Madhavi Reddy, MD7
1Brooklyn Hospital Center, Brooklyn, NY; 2MedStar Georgetown/Washington Hospital Center, Washington, DC; 3University of Texas Health, McGovern Medical School, Houston, TX; 4MacNeal Hospital Loyola Medicine, Berwyn, IL; 5SUNY Downstate Medical Center, Brooklyn, NY; 6University of Toronto, Toronto, ON, Canada; 7The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Colorectal cancer (CRC) is the third most commonly diagnosed cancer worldwide and accounts for a significant proportion of global cancer mortality. While advances in diagnosis and treatment have improved survival rates, CRC survivors face a substantial risk of non-cancer mortality, with cardiovascular disease (CVD) being a leading cause. Despite this, postoperative surveillance in CRC patients remains predominantly focused on cancer recurrence, often overlooking the significant burden of CVD. Emerging evidence suggests a complex interplay between CRC and CVD, driven by shared risk factors, chronic inflammation, and systemic treatment-related cardiotoxicity.
Methods: A retrospective cohort analysis was conducted using data from the TriNetX federated network, comparing two groups: Cohort 1 included 360,005 adult patients (≥18 years) diagnosed with CRC (ICD-10-CM: C18) without a diagnosis of heart failure (ICD-10CM: I50), while Cohort 2 consisted of 59,961 patients with both CRC and HF diagnosis. Propensity score matching was performed on 24 characteristics, including demographic variables (e.g., age, sex, race/ethnicity), oncology stage, and comorbid conditions (e.g., ischemic heart disease, diabetes mellitus, hypertensive diseases, chronic kidney disease). Cardiovascular outcomes between the cohorts were compared using risk measures and Kaplan-Meier survival analysis. Statistical significance was evaluated using the log-rank test and hazard ratios, and proportionality assumptions were tested.
Results: Each cohort consisted of 45,731 matched patients. Among Patients with CRC; HF cohort had significantly lower survival probabilities and higher mortality risk compared to cohort without HF. The outcome (death) in the control group was 30.3% and in the HF cohort group was 42.1%. We found that the OR for mortality was 1.389 (p-value < 0.001) (CI of 1.36-1.41). The hazard ratio (HR) for survival was 0.653 (95% CI: 0.639–0.667), indicating that the risk of death was substantially higher in CRC patients with HF. Median survival was reduced by over 1,200 days in the HF cohort (figure 1).
Discussion: Current CRC surveillance predominantly focuses on cancer recurrence, often overlooking the risks posed by comorbid conditions like HF. The data presented compellingly advocate for a paradigm shift towards integrated care pathways that concurrently address the dual burden of cancer and cardiovascular disease, ultimately optimizing outcomes for CRC patients.
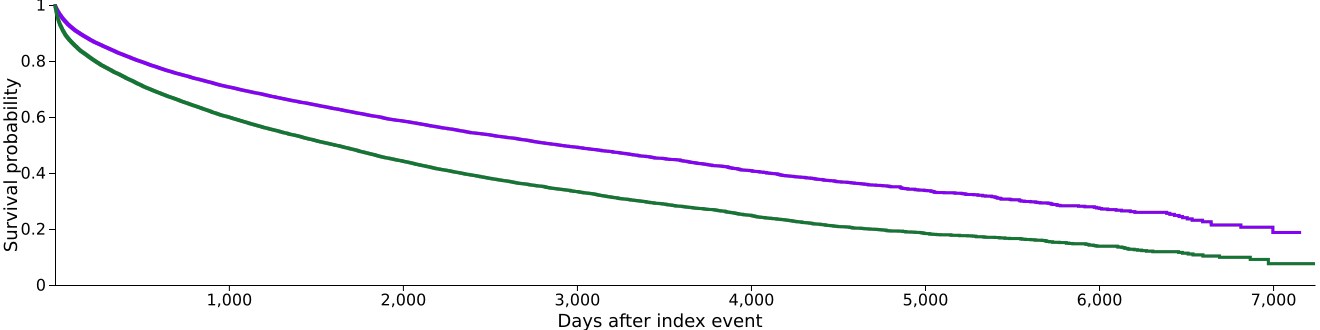
Figure: Figure 1: Kaplan-Meier survival analysis curve comparing colorectal cancer (CRC) patients without heart failure (HF) (purple) and those with HF (green).
Disclosures:
Iyad Al-Bustami indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Kenan Alrejjal indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Aashutosh Sah indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Ammar Abdulfattah indicated no relevant financial relationships.
Delwar Khan indicated no relevant financial relationships.
Daniel Low indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Iyad Al-Bustami, MD, MPH1, Sweta Lohani, MD1, Kenan Alrejjal, MBBS2, Kazi Haque, MD3, Aashutosh Sah, MD4, Chaula Desai, MD1, Ammar Yasser. Abdulfattah, MBBCh5, Delwar Khan, MD1, Daniel Low, MD6, Madhavi Reddy, MD7. P4541 - The Impact of Heart Failure on Colorectal Cancer Survival: A Propensity-Matched Cohort and Survival Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2MedStar Georgetown/Washington Hospital Center, Washington, DC; 3University of Texas Health, McGovern Medical School, Houston, TX; 4MacNeal Hospital Loyola Medicine, Berwyn, IL; 5SUNY Downstate Medical Center, Brooklyn, NY; 6University of Toronto, Toronto, ON, Canada; 7The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Colorectal cancer (CRC) is the third most commonly diagnosed cancer worldwide and accounts for a significant proportion of global cancer mortality. While advances in diagnosis and treatment have improved survival rates, CRC survivors face a substantial risk of non-cancer mortality, with cardiovascular disease (CVD) being a leading cause. Despite this, postoperative surveillance in CRC patients remains predominantly focused on cancer recurrence, often overlooking the significant burden of CVD. Emerging evidence suggests a complex interplay between CRC and CVD, driven by shared risk factors, chronic inflammation, and systemic treatment-related cardiotoxicity.
Methods: A retrospective cohort analysis was conducted using data from the TriNetX federated network, comparing two groups: Cohort 1 included 360,005 adult patients (≥18 years) diagnosed with CRC (ICD-10-CM: C18) without a diagnosis of heart failure (ICD-10CM: I50), while Cohort 2 consisted of 59,961 patients with both CRC and HF diagnosis. Propensity score matching was performed on 24 characteristics, including demographic variables (e.g., age, sex, race/ethnicity), oncology stage, and comorbid conditions (e.g., ischemic heart disease, diabetes mellitus, hypertensive diseases, chronic kidney disease). Cardiovascular outcomes between the cohorts were compared using risk measures and Kaplan-Meier survival analysis. Statistical significance was evaluated using the log-rank test and hazard ratios, and proportionality assumptions were tested.
Results: Each cohort consisted of 45,731 matched patients. Among Patients with CRC; HF cohort had significantly lower survival probabilities and higher mortality risk compared to cohort without HF. The outcome (death) in the control group was 30.3% and in the HF cohort group was 42.1%. We found that the OR for mortality was 1.389 (p-value < 0.001) (CI of 1.36-1.41). The hazard ratio (HR) for survival was 0.653 (95% CI: 0.639–0.667), indicating that the risk of death was substantially higher in CRC patients with HF. Median survival was reduced by over 1,200 days in the HF cohort (figure 1).
Discussion: Current CRC surveillance predominantly focuses on cancer recurrence, often overlooking the risks posed by comorbid conditions like HF. The data presented compellingly advocate for a paradigm shift towards integrated care pathways that concurrently address the dual burden of cancer and cardiovascular disease, ultimately optimizing outcomes for CRC patients.
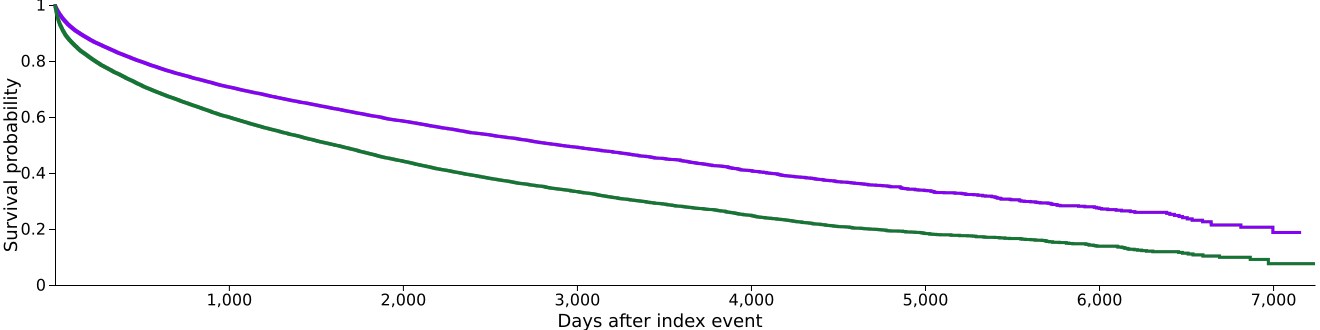
Figure: Figure 1: Kaplan-Meier survival analysis curve comparing colorectal cancer (CRC) patients without heart failure (HF) (purple) and those with HF (green).
Disclosures:
Iyad Al-Bustami indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Kenan Alrejjal indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Aashutosh Sah indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Ammar Abdulfattah indicated no relevant financial relationships.
Delwar Khan indicated no relevant financial relationships.
Daniel Low indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Iyad Al-Bustami, MD, MPH1, Sweta Lohani, MD1, Kenan Alrejjal, MBBS2, Kazi Haque, MD3, Aashutosh Sah, MD4, Chaula Desai, MD1, Ammar Yasser. Abdulfattah, MBBCh5, Delwar Khan, MD1, Daniel Low, MD6, Madhavi Reddy, MD7. P4541 - The Impact of Heart Failure on Colorectal Cancer Survival: A Propensity-Matched Cohort and Survival Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
