Tuesday Poster Session
Category: Colon
Trends in Mortality of Enterocolitis Due to <i>Clostridioides difficile</i> in the Adult Population: CDC Data Analysis (1999–2020)
P4536 - Trends in Mortality of Enterocolitis Due to Clostridioides difficile in the Adult Population: CDC Data Analysis (1999–2020)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ammad Javaid Chaudhary, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Hafsa Shahid, MD1, Ammad Javaid. Chaudhary, MD2, Alia Iftikhar, MBBS3, Fatima Sial, MBBS4, Rabia Shahid, MBBS5, Aqsa Shoukat, 6, Syed-Mohammed Jafri, MD2
1Brigham and Women's Hospital, Boston, MA; 2Henry Ford Health, Detroit, MI; 3King Edward Medical University, Pakistan, Lahore, Punjab, Pakistan; 4King Edward Medical University, Lahore, Punjab, Pakistan; 5Faisalabad Medical University, Pakistan, Lahore, Punjab, Pakistan; 6Superior University, Lahore, Punjab, Pakistan
Introduction: Clostridioides difficile infection remains a major cause of illness and death, particularly when it progresses to enterocolitis. This study analyzes CDC data (1999–2020) to assess long-term mortality trends and identify disparities by demographics, sex, and region. The aim is to inform future public health strategies targeting C. difficile–related mortality reduction.
Methods: We analyzed U.S. mortality data using the CDC WONDER database, including adults aged 25 to 85+ years. Deaths attributed to enterocolitis due to Clostridioides difficile were included. Age-adjusted mortality rates (AAMRs) per 100,000 were stratified by sex, race/ethnicity, region, state, and urbanization level.
Results: From 1999–2020, 192,283 deaths occurred due to C. difficile enterocolitis among adults aged 25 to 85+, with AAMRs rising from 0.85 to 3.43 per 100,000. Both sexes showed steep mortality increases from 1999 to 2005 (APC: 32.32 in males; 34.75 in females), slower rises until 2008/2011 (APC: 7.96 and 4.07 in males; 3.59 and 12.78 in females), followed by declines (APC: -1.34 and -11.12 in males; -3.59 and -12.78 in females). White individuals had the highest early rise until 2005 (APC: 34.16), then a slower increase until 2011 (APC: 3.85). Black and Hispanic populations showed sharp increases until 2006 (APC: 27.44 and 32.89), slower increases until 2011 (Black APC: 5.41) and 2010 (Hispanic APC: 7.23), then declines (Black APCs: -1.69, -10.70; Hispanic APCs: -2.62, -9.30). Regional patterns mirrored this, with the West showing prolonged rise until 2008 (APC: 22.81), and the Northeast recording the steepest rise from 2002–2005 (APC: 46.76), followed by the Midwest (1999–2005 APC: 33.66). The steepest decline was in the West (2015–2020 APC: -12.34). Urbanization trends followed a similar course. Medium metro and micropolitan areas had the highest early rises (APC: 37.96 and 34.84), while large central and small metro areas had the sharpest recent declines (APC: -12.85 and -12.38). Highest AAMRs were seen in Missouri and Ohio (5.16–8.51), and the lowest in Mississippi and Alaska (0.97–2.83).
Discussion: From 1999 to 2020, mortality from C. difficile enterocolitis rose before declining across all groups. The early increase was most pronounced in females, White individuals, the Northeast and Midwest, and medium metro areas. These findings underscore the need for targeted public health efforts in high-risk populations and persistently affected regions. AI tools were used to enhance writing clarity.
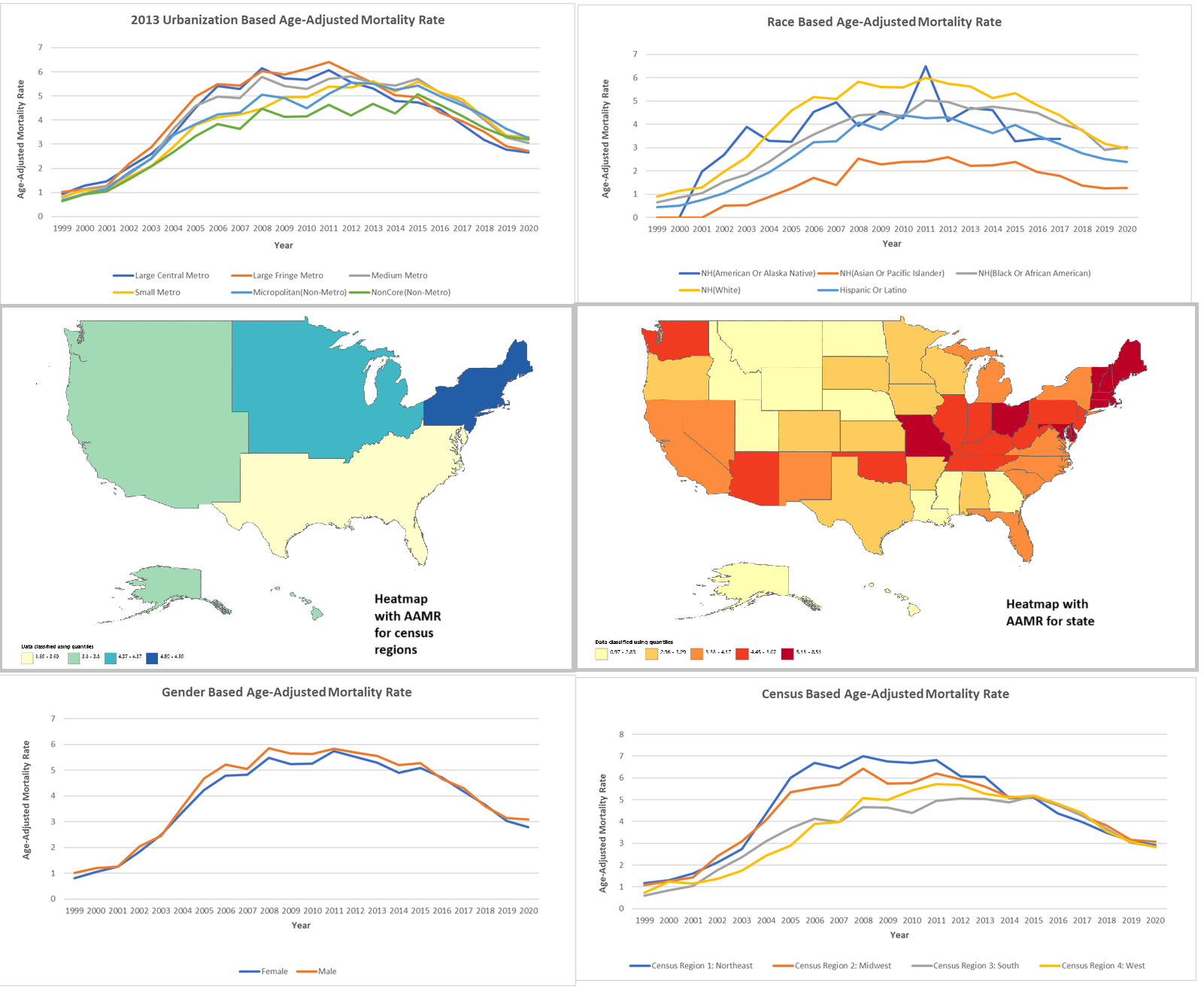
Figure: Trends in age-adjusted mortality rates (AAMRs) for C. difficile–related deaths among U.S. adults (1999–2020), stratified by region, sex, race/ethnicity, urbanization, and state-level distribution.
Disclosures:
Hafsa Shahid indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Alia Iftikhar indicated no relevant financial relationships.
Fatima Sial indicated no relevant financial relationships.
Rabia Shahid indicated no relevant financial relationships.
Aqsa Shoukat indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Hafsa Shahid, MD1, Ammad Javaid. Chaudhary, MD2, Alia Iftikhar, MBBS3, Fatima Sial, MBBS4, Rabia Shahid, MBBS5, Aqsa Shoukat, 6, Syed-Mohammed Jafri, MD2. P4536 - Trends in Mortality of Enterocolitis Due to <i>Clostridioides difficile</i> in the Adult Population: CDC Data Analysis (1999–2020), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brigham and Women's Hospital, Boston, MA; 2Henry Ford Health, Detroit, MI; 3King Edward Medical University, Pakistan, Lahore, Punjab, Pakistan; 4King Edward Medical University, Lahore, Punjab, Pakistan; 5Faisalabad Medical University, Pakistan, Lahore, Punjab, Pakistan; 6Superior University, Lahore, Punjab, Pakistan
Introduction: Clostridioides difficile infection remains a major cause of illness and death, particularly when it progresses to enterocolitis. This study analyzes CDC data (1999–2020) to assess long-term mortality trends and identify disparities by demographics, sex, and region. The aim is to inform future public health strategies targeting C. difficile–related mortality reduction.
Methods: We analyzed U.S. mortality data using the CDC WONDER database, including adults aged 25 to 85+ years. Deaths attributed to enterocolitis due to Clostridioides difficile were included. Age-adjusted mortality rates (AAMRs) per 100,000 were stratified by sex, race/ethnicity, region, state, and urbanization level.
Results: From 1999–2020, 192,283 deaths occurred due to C. difficile enterocolitis among adults aged 25 to 85+, with AAMRs rising from 0.85 to 3.43 per 100,000. Both sexes showed steep mortality increases from 1999 to 2005 (APC: 32.32 in males; 34.75 in females), slower rises until 2008/2011 (APC: 7.96 and 4.07 in males; 3.59 and 12.78 in females), followed by declines (APC: -1.34 and -11.12 in males; -3.59 and -12.78 in females). White individuals had the highest early rise until 2005 (APC: 34.16), then a slower increase until 2011 (APC: 3.85). Black and Hispanic populations showed sharp increases until 2006 (APC: 27.44 and 32.89), slower increases until 2011 (Black APC: 5.41) and 2010 (Hispanic APC: 7.23), then declines (Black APCs: -1.69, -10.70; Hispanic APCs: -2.62, -9.30). Regional patterns mirrored this, with the West showing prolonged rise until 2008 (APC: 22.81), and the Northeast recording the steepest rise from 2002–2005 (APC: 46.76), followed by the Midwest (1999–2005 APC: 33.66). The steepest decline was in the West (2015–2020 APC: -12.34). Urbanization trends followed a similar course. Medium metro and micropolitan areas had the highest early rises (APC: 37.96 and 34.84), while large central and small metro areas had the sharpest recent declines (APC: -12.85 and -12.38). Highest AAMRs were seen in Missouri and Ohio (5.16–8.51), and the lowest in Mississippi and Alaska (0.97–2.83).
Discussion: From 1999 to 2020, mortality from C. difficile enterocolitis rose before declining across all groups. The early increase was most pronounced in females, White individuals, the Northeast and Midwest, and medium metro areas. These findings underscore the need for targeted public health efforts in high-risk populations and persistently affected regions. AI tools were used to enhance writing clarity.
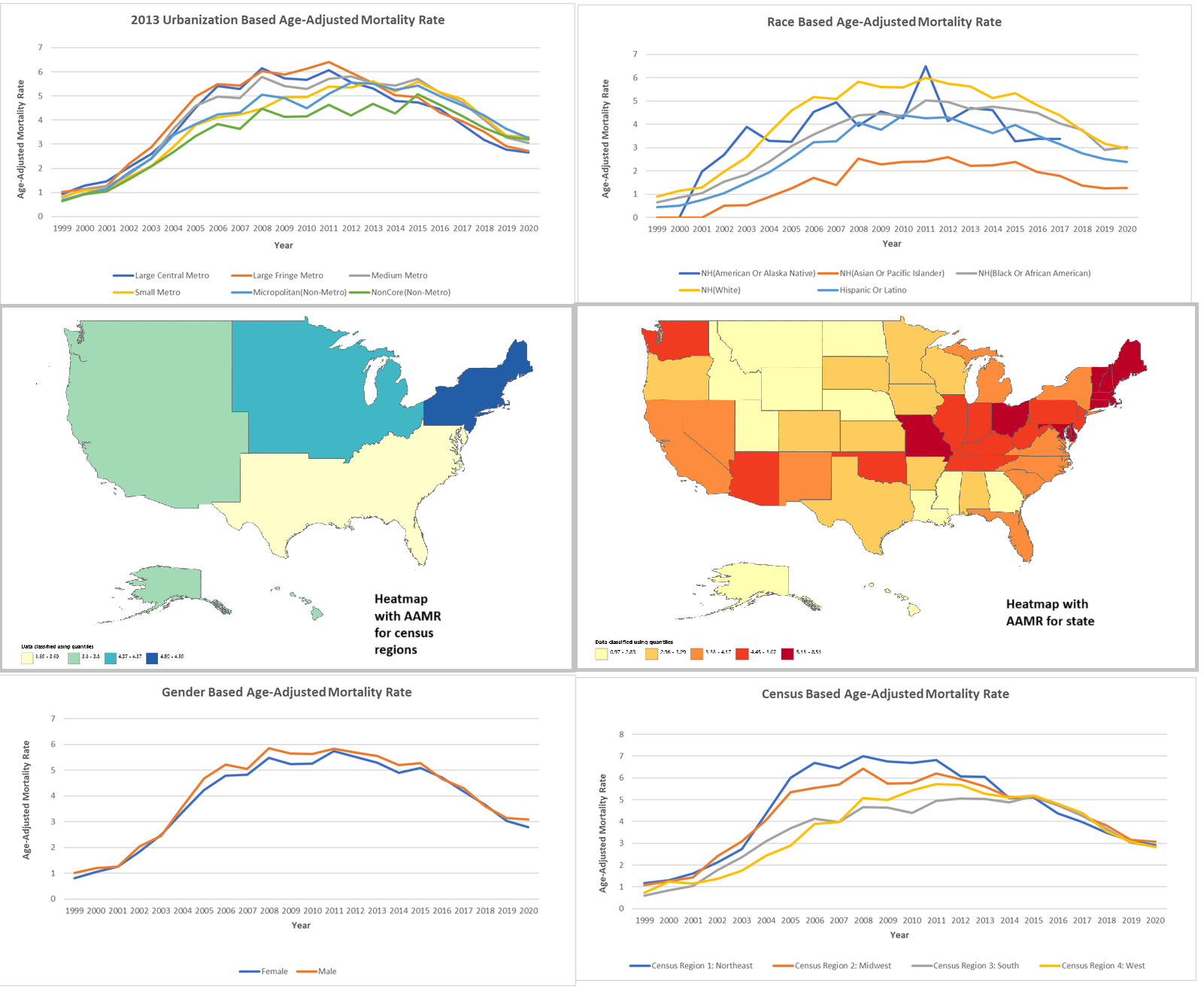
Figure: Trends in age-adjusted mortality rates (AAMRs) for C. difficile–related deaths among U.S. adults (1999–2020), stratified by region, sex, race/ethnicity, urbanization, and state-level distribution.
Disclosures:
Hafsa Shahid indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Alia Iftikhar indicated no relevant financial relationships.
Fatima Sial indicated no relevant financial relationships.
Rabia Shahid indicated no relevant financial relationships.
Aqsa Shoukat indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Hafsa Shahid, MD1, Ammad Javaid. Chaudhary, MD2, Alia Iftikhar, MBBS3, Fatima Sial, MBBS4, Rabia Shahid, MBBS5, Aqsa Shoukat, 6, Syed-Mohammed Jafri, MD2. P4536 - Trends in Mortality of Enterocolitis Due to <i>Clostridioides difficile</i> in the Adult Population: CDC Data Analysis (1999–2020), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
