Tuesday Poster Session
Category: Biliary/Pancreas
P4530 - A Case of Primary Choledocholithiasis Post-Choledochoduodenostomy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Fnu Arti, MD (she/her/hers)
Saint Francis Medical Center
Monroe, LA
Presenting Author(s)
Fnu Arti, MD, Harikrishna Bandla, MD, Rahul Robaish. Kumar, MD, Dirgha Upendrabhai Patel, MD, Henry H. Hinkle, MD
Saint Francis Medical Center, Monroe, LA
Introduction: Choledocholithiasis (stone in the common bile duct) leads to biliary obstruction, jaundice, and complications like cholangitis and pancreatitis. Primary choledocholithiasis, often due to bile stasis or infection, is rare, unlike secondary cases from gallbladder stone migration. Treatment involves stone removal and obstruction relief, with biliary-enteric anastomosis for recurrent disease. We report an unusual case of late-onset primary choledocholithiasis eight years post-cholecystectomy in a patient with prior choledochoduodenostomy, emphasizing diagnostic and management challenges.
Case Description/
Methods: An 84-year-old male with known history of a gallbladder polyp (post cholecystectomy 8 years prior) and duodenal diverticulum (post choledochoduodenostomy 4 years prior), presented with epigastric pain, nausea, vomiting, pruritus, and weight loss. Examination revealed jaundice and abdominal tenderness. Labs showed cholestasis, and Abdominal CT scan demonstrated dilated intrahepatic ducts with distal CBD obstruction. ERCP confirmed choledocholithiasis (fig-1), but altered anatomy precluded sphincterotomy. Partial stone extraction was achieved; double-pigtail stent was placed for larger stone breakdown (fig-2). After failed repeat ERCP, referral to a specialized center enabled successful 2 cm stone removal using cholangioscopy and hydraulic lithotripsy.
Discussion: Although bile duct stones can occur following cholecystectomy, they are most prevalent within the first three years following the procedure. After the three-year mark, migration of surgical clips is considered the most common mechanism for choledocholithiasis, with stone formation occurring much less likely. The exact mechanism for delayed stone formation and CBD obstruction remains unknown, but possible explanations include primary hepatic lithiasis and retrograde accumulation of debris in the CBD. This case demonstrates late choledocholithiasis following cholecystectomy and choledochoduodenostomy—a standard treatment for recurrent stones that paradoxically contributed to obstruction due to altered anatomy. It highlights the limitations of conventional endoscopic approaches and the necessity of advanced techniques like cholangioscopy. Long-term monitoring and specialized multidisciplinary care are crucial for high-risk patients to ensure optimal outcomes.
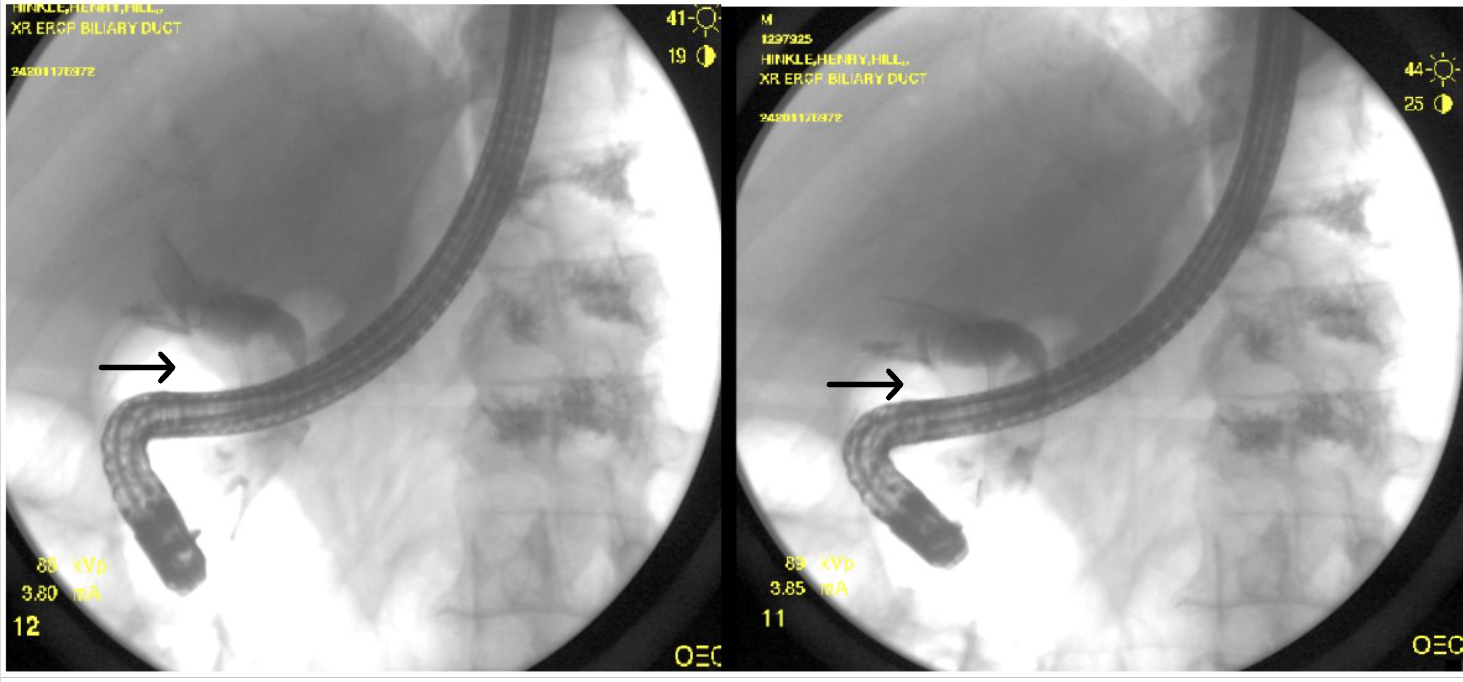
Figure: Figure 1 showing filling defects due to large stones during ERCP contrast injection highlighted by black arrows.
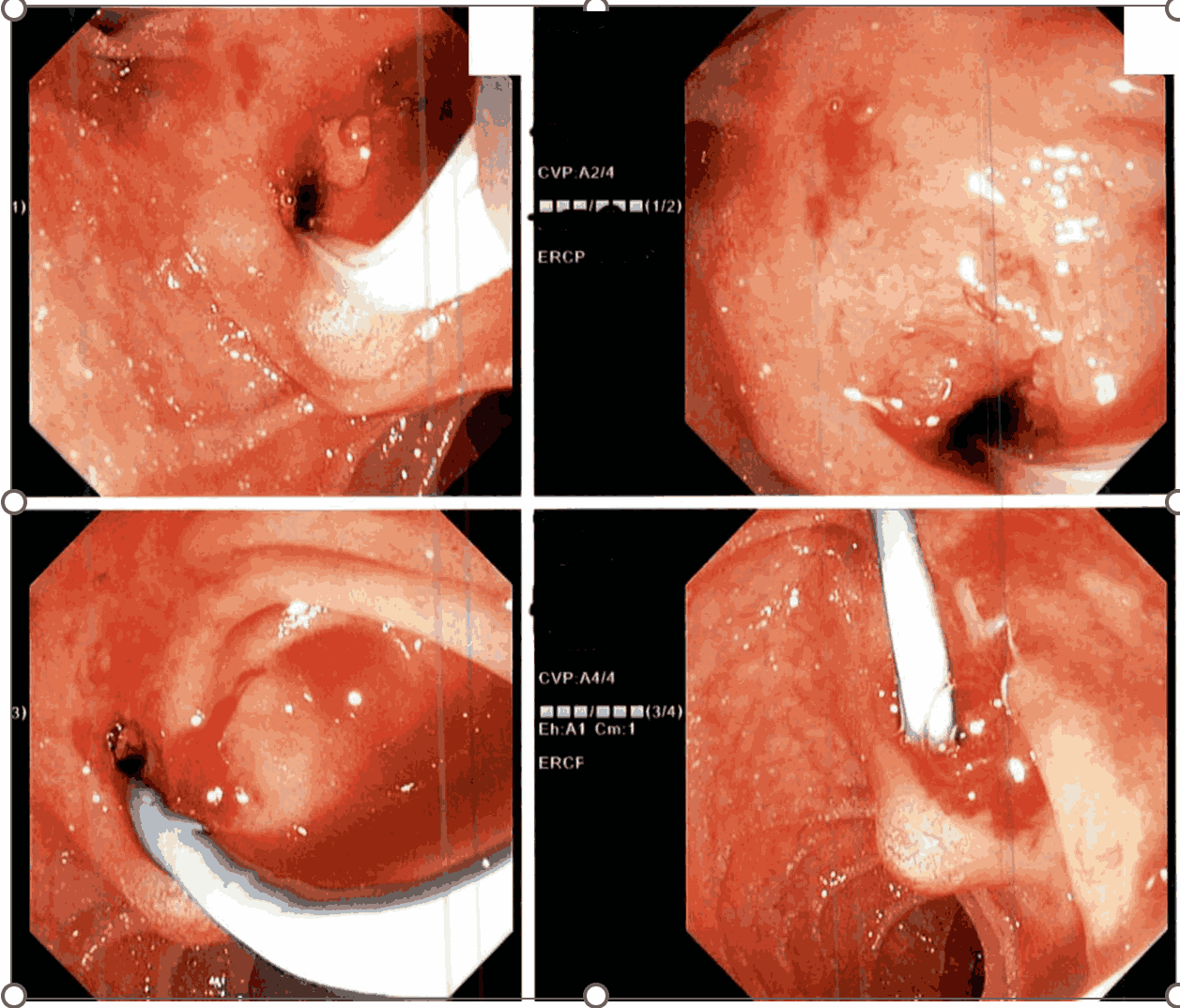
Figure: Figure 2 highlighting endoscopic visualization and double pigtail stent placement.
Disclosures:
Fnu Arti indicated no relevant financial relationships.
Harikrishna Bandla indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Dirgha Upendrabhai Patel indicated no relevant financial relationships.
Henry Hinkle indicated no relevant financial relationships.
Fnu Arti, MD, Harikrishna Bandla, MD, Rahul Robaish. Kumar, MD, Dirgha Upendrabhai Patel, MD, Henry H. Hinkle, MD. P4530 - A Case of Primary Choledocholithiasis Post-Choledochoduodenostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Saint Francis Medical Center, Monroe, LA
Introduction: Choledocholithiasis (stone in the common bile duct) leads to biliary obstruction, jaundice, and complications like cholangitis and pancreatitis. Primary choledocholithiasis, often due to bile stasis or infection, is rare, unlike secondary cases from gallbladder stone migration. Treatment involves stone removal and obstruction relief, with biliary-enteric anastomosis for recurrent disease. We report an unusual case of late-onset primary choledocholithiasis eight years post-cholecystectomy in a patient with prior choledochoduodenostomy, emphasizing diagnostic and management challenges.
Case Description/
Methods: An 84-year-old male with known history of a gallbladder polyp (post cholecystectomy 8 years prior) and duodenal diverticulum (post choledochoduodenostomy 4 years prior), presented with epigastric pain, nausea, vomiting, pruritus, and weight loss. Examination revealed jaundice and abdominal tenderness. Labs showed cholestasis, and Abdominal CT scan demonstrated dilated intrahepatic ducts with distal CBD obstruction. ERCP confirmed choledocholithiasis (fig-1), but altered anatomy precluded sphincterotomy. Partial stone extraction was achieved; double-pigtail stent was placed for larger stone breakdown (fig-2). After failed repeat ERCP, referral to a specialized center enabled successful 2 cm stone removal using cholangioscopy and hydraulic lithotripsy.
Discussion: Although bile duct stones can occur following cholecystectomy, they are most prevalent within the first three years following the procedure. After the three-year mark, migration of surgical clips is considered the most common mechanism for choledocholithiasis, with stone formation occurring much less likely. The exact mechanism for delayed stone formation and CBD obstruction remains unknown, but possible explanations include primary hepatic lithiasis and retrograde accumulation of debris in the CBD. This case demonstrates late choledocholithiasis following cholecystectomy and choledochoduodenostomy—a standard treatment for recurrent stones that paradoxically contributed to obstruction due to altered anatomy. It highlights the limitations of conventional endoscopic approaches and the necessity of advanced techniques like cholangioscopy. Long-term monitoring and specialized multidisciplinary care are crucial for high-risk patients to ensure optimal outcomes.
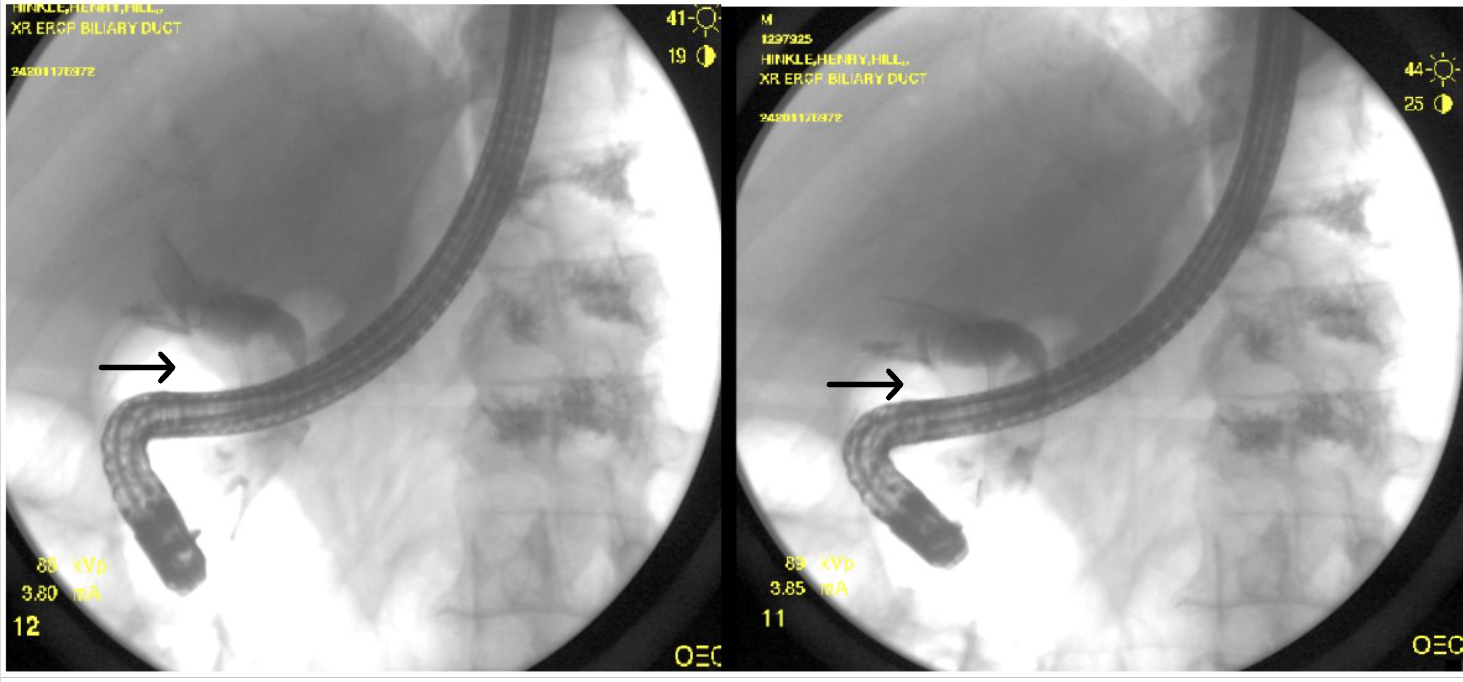
Figure: Figure 1 showing filling defects due to large stones during ERCP contrast injection highlighted by black arrows.
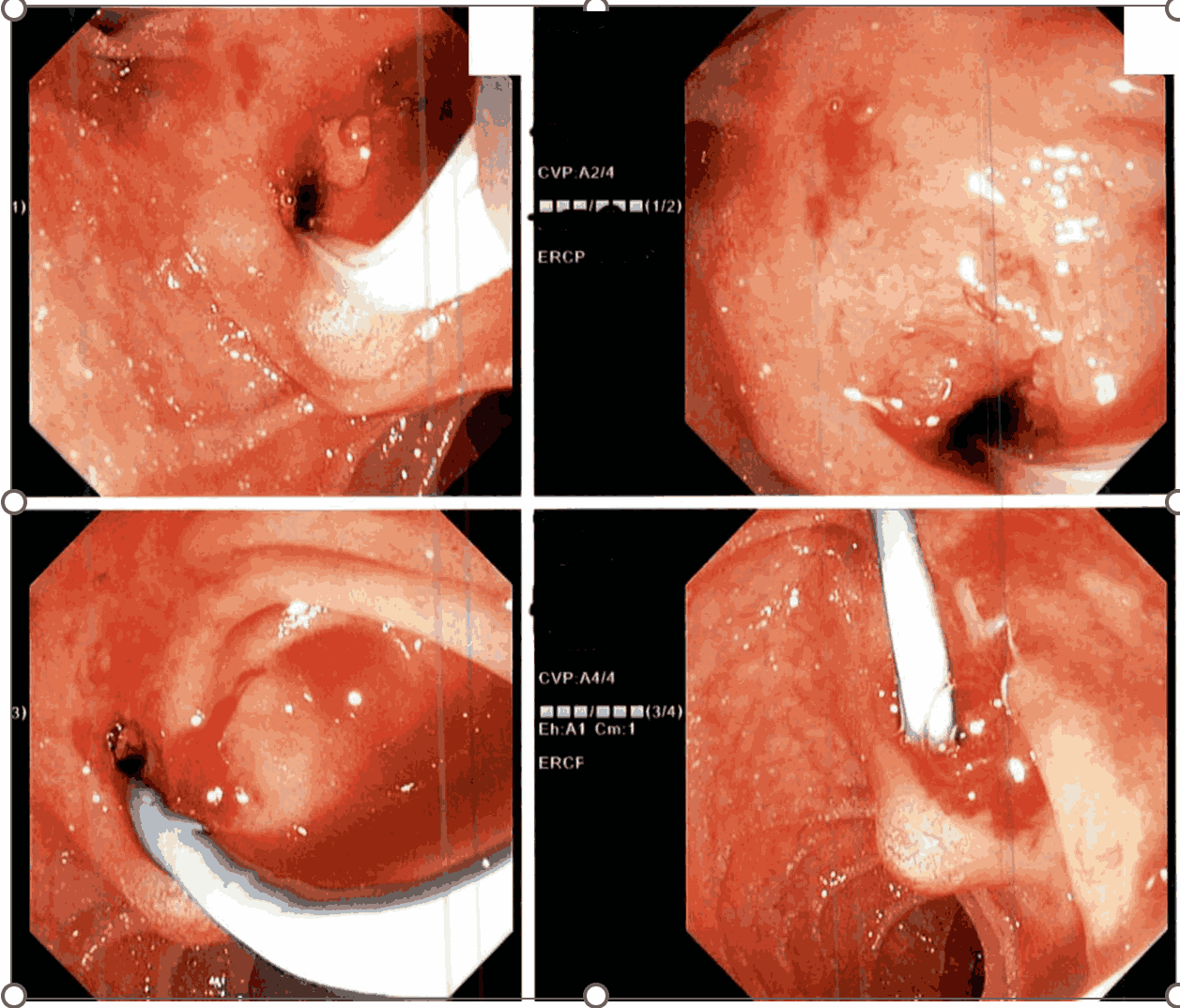
Figure: Figure 2 highlighting endoscopic visualization and double pigtail stent placement.
Disclosures:
Fnu Arti indicated no relevant financial relationships.
Harikrishna Bandla indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Dirgha Upendrabhai Patel indicated no relevant financial relationships.
Henry Hinkle indicated no relevant financial relationships.
Fnu Arti, MD, Harikrishna Bandla, MD, Rahul Robaish. Kumar, MD, Dirgha Upendrabhai Patel, MD, Henry H. Hinkle, MD. P4530 - A Case of Primary Choledocholithiasis Post-Choledochoduodenostomy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
