Tuesday Poster Session
Category: Biliary/Pancreas
P4528 - Delayed Diagnosis of Pancreaticobiliary Maljunction in an Elderly Patient: A Rare Cause of Recurrent Pancreatitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MH
Madiha Haseeb, MBBS
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Neha Boski, MD, FRCR1, Madiha Haseeb, MBBS2, Kausar Bano, MBBS3, Mahendra Kumar, MBBS4, Parvinder Kaur, MD5, Rohan Raj, MBBS6
1Apollo Radiology International, Hyderabad, India, Hyderabad, Telangana, India; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3Katihar Medical College Hospital, Katihar, Bihar, India; 4Sardar Patel Medical College, Bikaner, India, Bikaner, Rajasthan, India; 5Crimean State Medical University named after Sal Georgivsky Simferopol, Ukraine, Nawanshahr, Punjab, India; 6Memorial Hospital at Gulfport, Gulfport, MS
Introduction: Pancreaticobiliary maljunction (PBM) is a rare congenital anomaly in which the pancreatic and bile ducts join outside the duodenal wall, forming a long common channel. This anatomical variant prevents regulation by the sphincter of Oddi, leading to bidirectional reflux between bile and pancreatic secretions. PBM is classified into two types: with and without congenital choledochal cyst (CCD). While pediatric cases typically present with pancreatitis and liver dysfunction, adult presentations are rarer and more commonly associated with cholelithiasis or biliary tract malignancies. Delayed recognition in elderly patients remains infrequently documented.
Case Description/
Methods: A woman in her late seventies presented with intermittent upper abdominal discomfort. Routine labs showed mildly elevated alkaline phosphatase (126 IU/L and 146 IU/L two months apart), with normal bilirubin and aminotransferase levels, and borderline elevations in serum amylase and lipase. There was no history of alcohol consumption. Abdominal ultrasound revealed mild dilation of the pancreatic duct. MRI with MRCP demonstrated pancreaticobiliary maljunction with a long common channel joining outside the duodenal wall, without choledochal cyst formation. Additional findings included mild pancreatic body atrophy and dilated ductules in the uncinate process, suggestive of chronic pancreatitis secondary to pancreaticobiliary reflux. No mass lesions or calculi were identified. Given the patient’s age, absence of malignancy, and mild clinical symptoms, expectant management with imaging follow-up was advised.
Discussion: Pancreaticobiliary maljunction (PBM) is typically identified in childhood or young adulthood, but this case underscores that it can remain clinically silent and present later in life with only subtle biochemical and imaging findings. While PBM associated with a choledochal cyst often necessitates surgical bile diversion, cases without cysts are generally managed with prophylactic cholecystectomy due to the elevated risk of biliary tract malignancy. In our patient, expectant management was selected given her advanced age, absence of neoplastic changes, and mild, intermittent symptoms. This case highlights the importance of considering PBM even in elderly patients without classic symptoms and the diagnostic value of MRCP in subtle, delayed presentations.
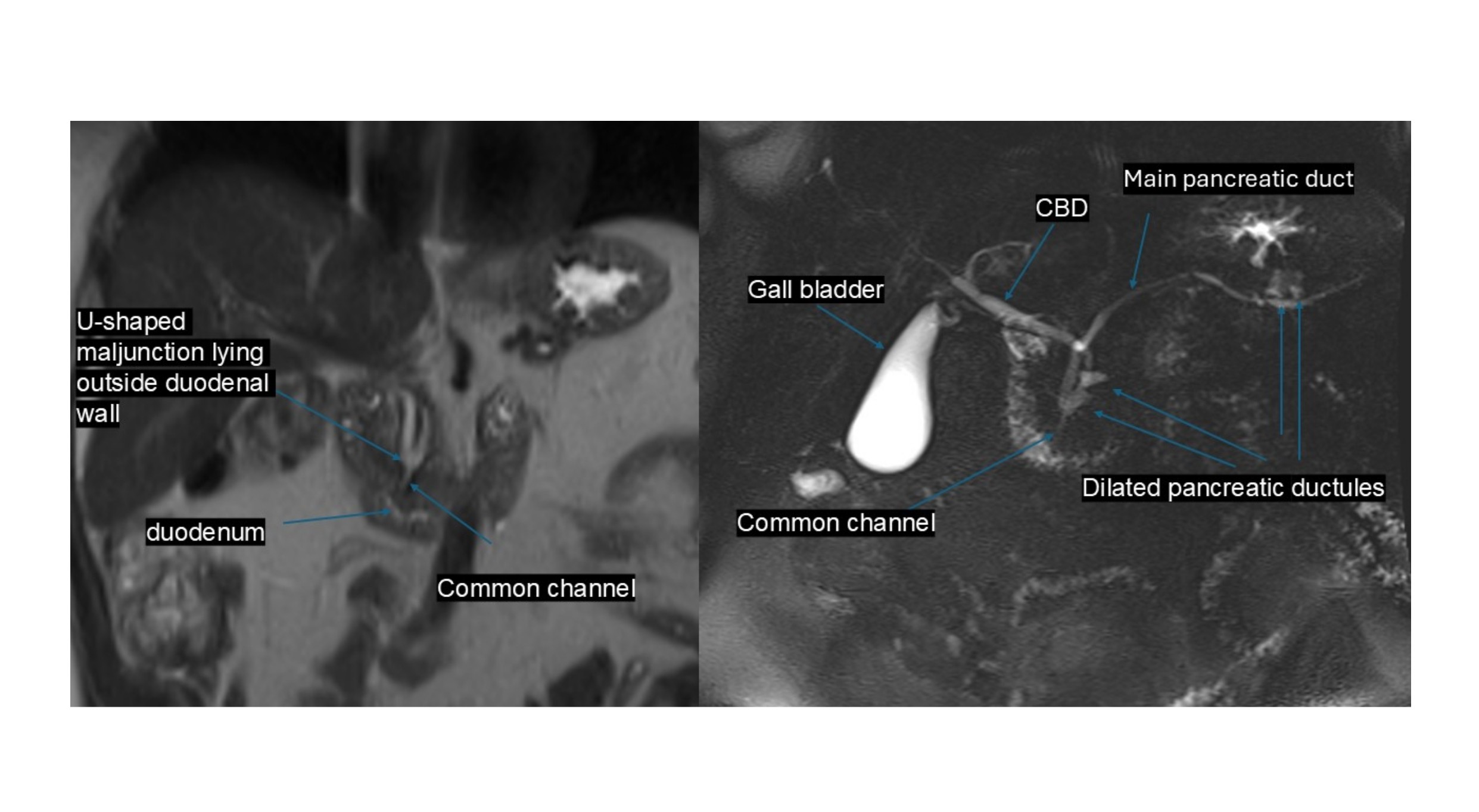
Figure: Coronal abdominal MR image (left) shows the pancreaticobiliary junction located outside the duodenal wall. MRCP image (right) demonstrates a long common channel with dilated pancreatic ductules. The common bile duct is of normal caliber, with no evidence of choledochal cyst, ductal obstruction, or intraluminal mass.
Disclosures:
Neha Boski indicated no relevant financial relationships.
Madiha Haseeb indicated no relevant financial relationships.
Kausar Bano indicated no relevant financial relationships.
Mahendra Kumar indicated no relevant financial relationships.
Parvinder Kaur indicated no relevant financial relationships.
Rohan Raj indicated no relevant financial relationships.
Neha Boski, MD, FRCR1, Madiha Haseeb, MBBS2, Kausar Bano, MBBS3, Mahendra Kumar, MBBS4, Parvinder Kaur, MD5, Rohan Raj, MBBS6. P4528 - Delayed Diagnosis of Pancreaticobiliary Maljunction in an Elderly Patient: A Rare Cause of Recurrent Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Apollo Radiology International, Hyderabad, India, Hyderabad, Telangana, India; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3Katihar Medical College Hospital, Katihar, Bihar, India; 4Sardar Patel Medical College, Bikaner, India, Bikaner, Rajasthan, India; 5Crimean State Medical University named after Sal Georgivsky Simferopol, Ukraine, Nawanshahr, Punjab, India; 6Memorial Hospital at Gulfport, Gulfport, MS
Introduction: Pancreaticobiliary maljunction (PBM) is a rare congenital anomaly in which the pancreatic and bile ducts join outside the duodenal wall, forming a long common channel. This anatomical variant prevents regulation by the sphincter of Oddi, leading to bidirectional reflux between bile and pancreatic secretions. PBM is classified into two types: with and without congenital choledochal cyst (CCD). While pediatric cases typically present with pancreatitis and liver dysfunction, adult presentations are rarer and more commonly associated with cholelithiasis or biliary tract malignancies. Delayed recognition in elderly patients remains infrequently documented.
Case Description/
Methods: A woman in her late seventies presented with intermittent upper abdominal discomfort. Routine labs showed mildly elevated alkaline phosphatase (126 IU/L and 146 IU/L two months apart), with normal bilirubin and aminotransferase levels, and borderline elevations in serum amylase and lipase. There was no history of alcohol consumption. Abdominal ultrasound revealed mild dilation of the pancreatic duct. MRI with MRCP demonstrated pancreaticobiliary maljunction with a long common channel joining outside the duodenal wall, without choledochal cyst formation. Additional findings included mild pancreatic body atrophy and dilated ductules in the uncinate process, suggestive of chronic pancreatitis secondary to pancreaticobiliary reflux. No mass lesions or calculi were identified. Given the patient’s age, absence of malignancy, and mild clinical symptoms, expectant management with imaging follow-up was advised.
Discussion: Pancreaticobiliary maljunction (PBM) is typically identified in childhood or young adulthood, but this case underscores that it can remain clinically silent and present later in life with only subtle biochemical and imaging findings. While PBM associated with a choledochal cyst often necessitates surgical bile diversion, cases without cysts are generally managed with prophylactic cholecystectomy due to the elevated risk of biliary tract malignancy. In our patient, expectant management was selected given her advanced age, absence of neoplastic changes, and mild, intermittent symptoms. This case highlights the importance of considering PBM even in elderly patients without classic symptoms and the diagnostic value of MRCP in subtle, delayed presentations.
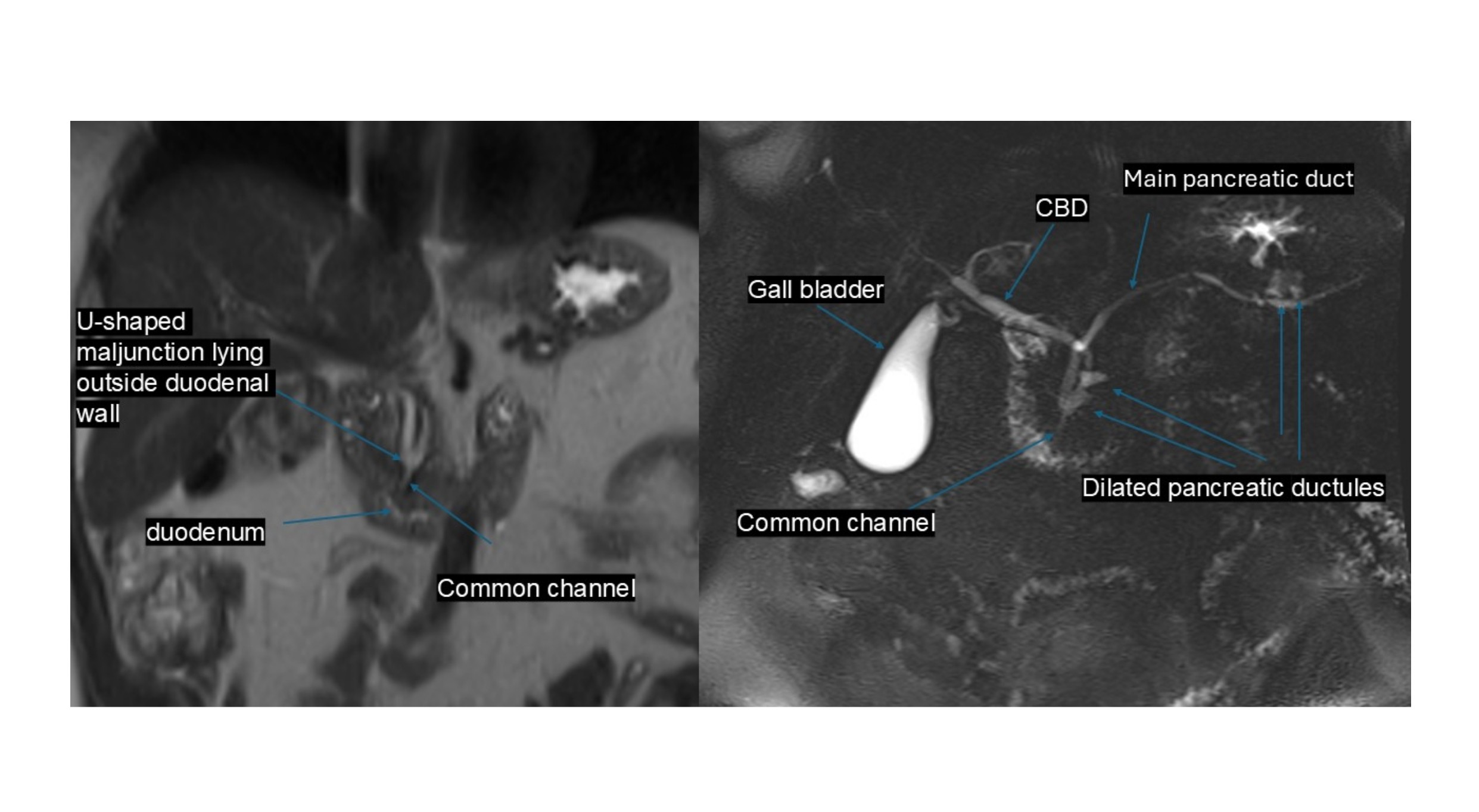
Figure: Coronal abdominal MR image (left) shows the pancreaticobiliary junction located outside the duodenal wall. MRCP image (right) demonstrates a long common channel with dilated pancreatic ductules. The common bile duct is of normal caliber, with no evidence of choledochal cyst, ductal obstruction, or intraluminal mass.
Disclosures:
Neha Boski indicated no relevant financial relationships.
Madiha Haseeb indicated no relevant financial relationships.
Kausar Bano indicated no relevant financial relationships.
Mahendra Kumar indicated no relevant financial relationships.
Parvinder Kaur indicated no relevant financial relationships.
Rohan Raj indicated no relevant financial relationships.
Neha Boski, MD, FRCR1, Madiha Haseeb, MBBS2, Kausar Bano, MBBS3, Mahendra Kumar, MBBS4, Parvinder Kaur, MD5, Rohan Raj, MBBS6. P4528 - Delayed Diagnosis of Pancreaticobiliary Maljunction in an Elderly Patient: A Rare Cause of Recurrent Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
