Tuesday Poster Session
Category: Biliary/Pancreas
P4526 - The Double Duct Dilemma: When Methadone Mimics Malignancy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ana Finke Abbott, MD
Norwalk Hospital
Norwalk, CT
Presenting Author(s)
Ana Finke Abbott, MD, Syed Alishan Nasir, MD, Yonatan Hillman, MD
Norwalk Hospital, Norwalk, CT
Introduction: The double duct sign is an abnormal simultaneous dilation of the pancreatic duct (PD) and common bile duct (CBD). While typically due to an obstructive pathology and often indicative of underlying malignancy, benign etiologies have also been implicated. Once identified on CT or MRI, further evaluation via endoscopic ultrasound (EUS) or endoscopic retrograde cholangiopancreatography (ERCP) is typically performed. Methadone is an opioid agonist used to treat opioid use disorder that has been shown to alter gastrointestinal motility and impair gallbladder (GB) contraction, potentially contributing to biliary stasis and ductal dilation. We report a case of incidental double-duct sign in a patient on chronic methadone maintenance therapy (MMT).
Case Description/
Methods: A 67-year-old male with a prior history of heroin use, sober for 25 years, now on chronic methadone, presented with a two-week history of constipation, nausea, and vomiting, without associated weight loss. On admission, he was hemodynamically stable, and labs, including liver enzymes, bilirubin, lipase, complete blood count, and basic metabolic panel, were within normal limits. CT abdomen revealed dilated PD and CBD, consistent with double duct sign, raising concern for possible periampullary malignancy. MRI confirmed a 12 mm CBD, 6 mm PD, a 1.4 cm gallstone in the GB, and no obstructing lesions or masses. EUS showed esophagitis and gastritis, with normal duodenum and ampulla. ERCP confirmed CBD dilation to 8 mm, common hepatic duct dilation to 11 mm, and a 17 mm gallstone in the GB neck. The PD was mildly dilated with diffuse echogenicity in the pancreatic body, without masses or signs of malignancy. No anatomic cause for the double duct sign was identified. The hospitalization was complicated by persistent opioid-induced constipation, which responded to methylnaltrexone, and the patient was discharged with outpatient surgical referral for elective cholecystectomy.
Discussion: This case highlights a clinically relevant association between chronic methadone use and the double duct sign. In the absence of malignancy or obstruction, chronic opioid therapy may contribute to biliary and pancreatic duct dilation via its inhibitory effects on gastrointestinal and biliary motility. While MMT use remains prevalent, specialists should remain vigilant for its potential to mimic more serious conditions. Recognizing this association may help avoid unnecessary invasive procedures and guide individualized diagnostic and therapeutic strategies.
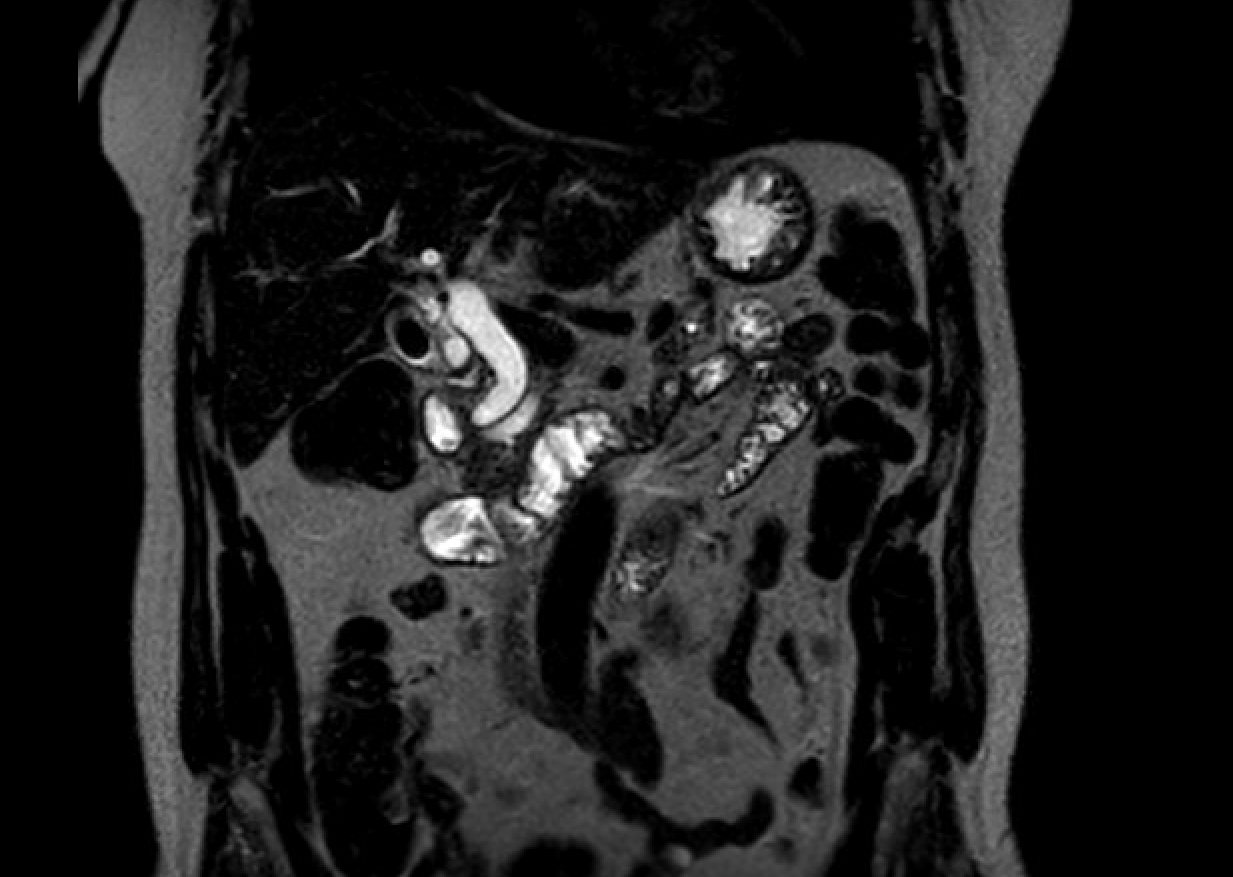
Figure: Double Duct on MRCP
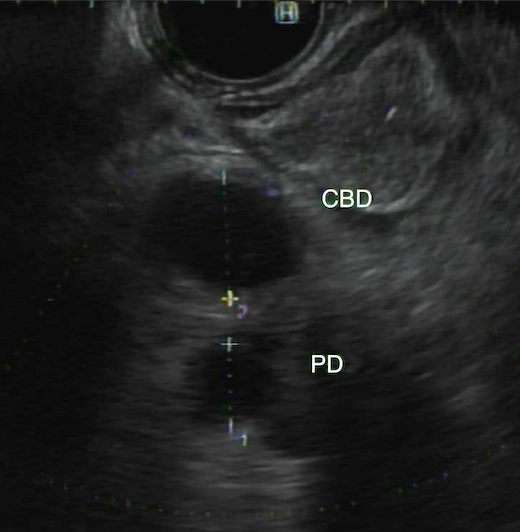
Figure: Double Duct EUS
Disclosures:
Ana Finke Abbott indicated no relevant financial relationships.
Syed Alishan Nasir indicated no relevant financial relationships.
Yonatan Hillman indicated no relevant financial relationships.
Ana Finke Abbott, MD, Syed Alishan Nasir, MD, Yonatan Hillman, MD. P4526 - The Double Duct Dilemma: When Methadone Mimics Malignancy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Norwalk Hospital, Norwalk, CT
Introduction: The double duct sign is an abnormal simultaneous dilation of the pancreatic duct (PD) and common bile duct (CBD). While typically due to an obstructive pathology and often indicative of underlying malignancy, benign etiologies have also been implicated. Once identified on CT or MRI, further evaluation via endoscopic ultrasound (EUS) or endoscopic retrograde cholangiopancreatography (ERCP) is typically performed. Methadone is an opioid agonist used to treat opioid use disorder that has been shown to alter gastrointestinal motility and impair gallbladder (GB) contraction, potentially contributing to biliary stasis and ductal dilation. We report a case of incidental double-duct sign in a patient on chronic methadone maintenance therapy (MMT).
Case Description/
Methods: A 67-year-old male with a prior history of heroin use, sober for 25 years, now on chronic methadone, presented with a two-week history of constipation, nausea, and vomiting, without associated weight loss. On admission, he was hemodynamically stable, and labs, including liver enzymes, bilirubin, lipase, complete blood count, and basic metabolic panel, were within normal limits. CT abdomen revealed dilated PD and CBD, consistent with double duct sign, raising concern for possible periampullary malignancy. MRI confirmed a 12 mm CBD, 6 mm PD, a 1.4 cm gallstone in the GB, and no obstructing lesions or masses. EUS showed esophagitis and gastritis, with normal duodenum and ampulla. ERCP confirmed CBD dilation to 8 mm, common hepatic duct dilation to 11 mm, and a 17 mm gallstone in the GB neck. The PD was mildly dilated with diffuse echogenicity in the pancreatic body, without masses or signs of malignancy. No anatomic cause for the double duct sign was identified. The hospitalization was complicated by persistent opioid-induced constipation, which responded to methylnaltrexone, and the patient was discharged with outpatient surgical referral for elective cholecystectomy.
Discussion: This case highlights a clinically relevant association between chronic methadone use and the double duct sign. In the absence of malignancy or obstruction, chronic opioid therapy may contribute to biliary and pancreatic duct dilation via its inhibitory effects on gastrointestinal and biliary motility. While MMT use remains prevalent, specialists should remain vigilant for its potential to mimic more serious conditions. Recognizing this association may help avoid unnecessary invasive procedures and guide individualized diagnostic and therapeutic strategies.
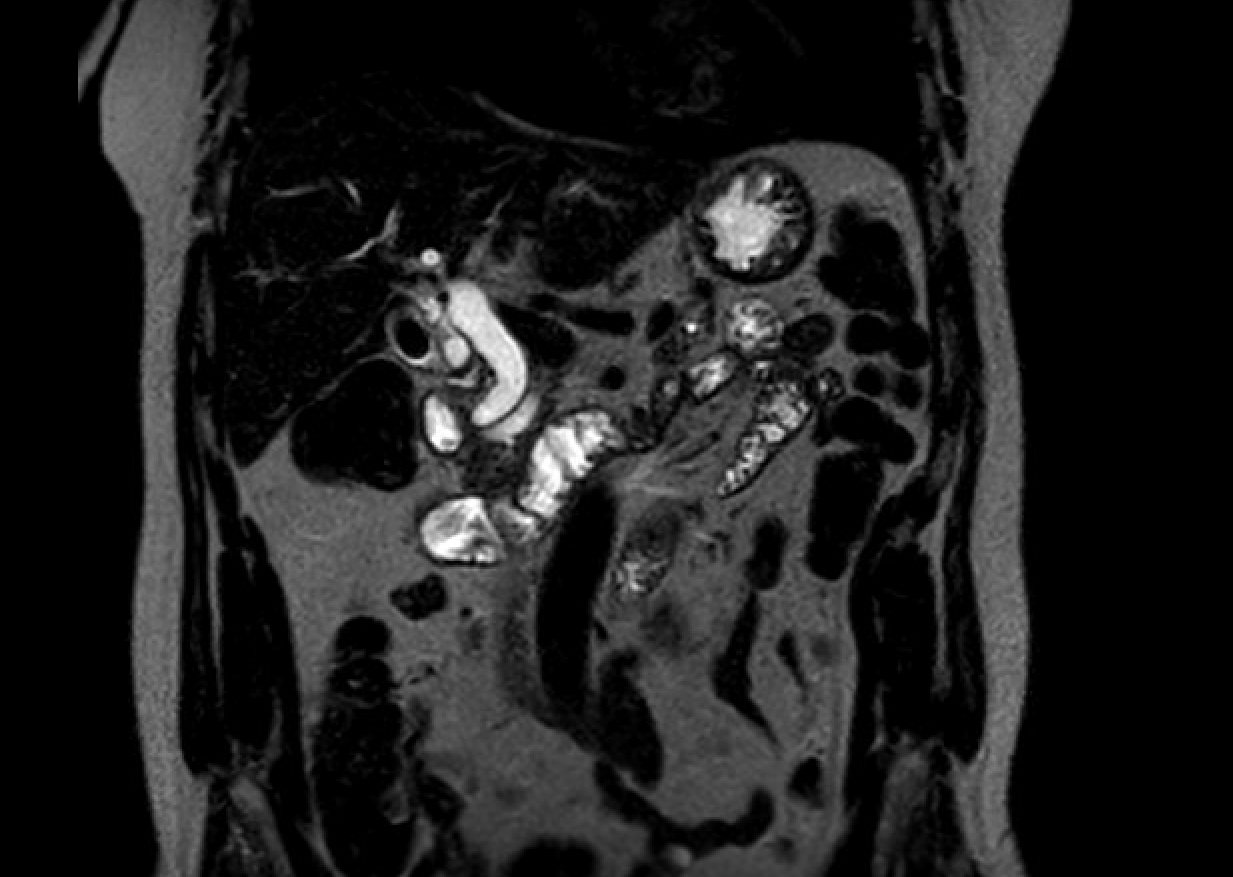
Figure: Double Duct on MRCP
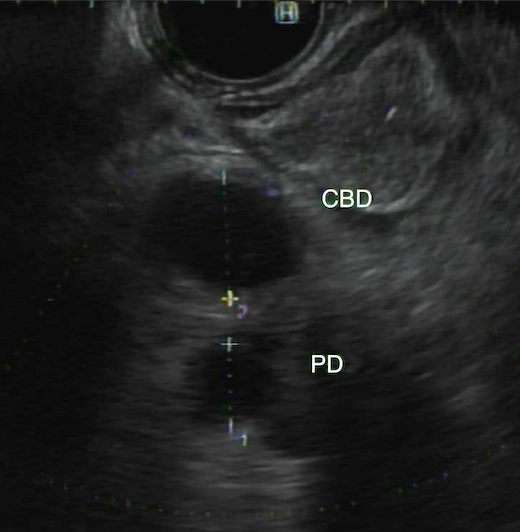
Figure: Double Duct EUS
Disclosures:
Ana Finke Abbott indicated no relevant financial relationships.
Syed Alishan Nasir indicated no relevant financial relationships.
Yonatan Hillman indicated no relevant financial relationships.
Ana Finke Abbott, MD, Syed Alishan Nasir, MD, Yonatan Hillman, MD. P4526 - The Double Duct Dilemma: When Methadone Mimics Malignancy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
