Tuesday Poster Session
Category: Biliary/Pancreas
P4512 - A Pancreas's Tail, a Spleen's Hilum, and a Squamous Cell Cancer
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yannis S. Lafazanos, DO (he/him/his)
Advocate Lutheran General
Long Grove, IL
Presenting Author(s)
Yannis S. Lafazanos, DO1, Sufyan AbdulMujeeb, DO2, Asif Lakha, MD3, Nahren Asado, MD3, Eli Ehrenpreis, MD, FACG2
1Advocate Lutheran General, Long Grove, IL; 2Advocate Lutheran General, Park Ridge, IL; 3Advocate Lutheran General Hospital, Park Ridge, IL
Introduction: Primary squamous cell carcinoma of the pancreas (SCCP) is an extremely rare clinical entity, comprising anywhere between 0.5 to 5% of all pancreatic malignancies, with rising incidence. Pancreatic tissue, normally devoid of squamous cells, must undergo squamous metaplastic changes of its columnar ductal cells, either secondary to inflammation or within a pre-existing adenocarcinoma. Clinical data is poor for SCCP, with diagnostic pathways and treatment options limited, making this area ripe for standardization.
Case Description/
Methods: Our patient is a 76-year-old male with no significant past medical history who presented to his primary care physician’s office with a 4-month history of unintentional weight loss and left upper quadrant abdominal pain. He also noticed anorexia, early satiety, and night sweats. Examination was only notable for splenomegaly. Comprehensive metabolic panel was normal. MRI abdomen showed a large splenic cystic/solid lesion with possible invasion of the pancreas (Figure 1). GI was consulted for EUS with FNA of the left upper quadrant mass, which resulted in multiple biopsies along the splenic hilum and pancreatic tail. Pathology only showed rare, atypical changes, without a clear diagnosis. A few weeks later, he was evaluated by surgical oncology and taken to the OR for removal of a 17 cm tumor with distal pancreatectomy, splenectomy, omentectomy and transverse colon resection, positive for squamous cell carcinoma of the pancreas (Figure 2). He is currently undergoing adjuvant chemotherapy.
Discussion: For our patient, a SCCP that quickly metastasized from the pancreatic tail to the hilar spleen promoted confounding symptoms derived from splenic involvement. EUS with FNA of this splenic lesion was productive of nondiagnostic pathology, despite multiple sites biopsied, likely resultant of cystic aspiration, and points to the difficulty of transgastric biopsy of the left upper quadrant. Typically, MRI imaging and surgical intervention, at least in early-stage cancers, are the most common management strategies amongst the roughly 50 cases of SCCP present in the literature.
The gastroenterologist also has a role in mediating risk factors for SCCP, including mitigation of inflammatory states, like chronic pancreatitis, and careful pancreatic duct intervention, mostly related to stent placement, which have been implicated in many of the cases reviewed for this report. Our case should serve as further example for the need for continued clinical study of SCCP.
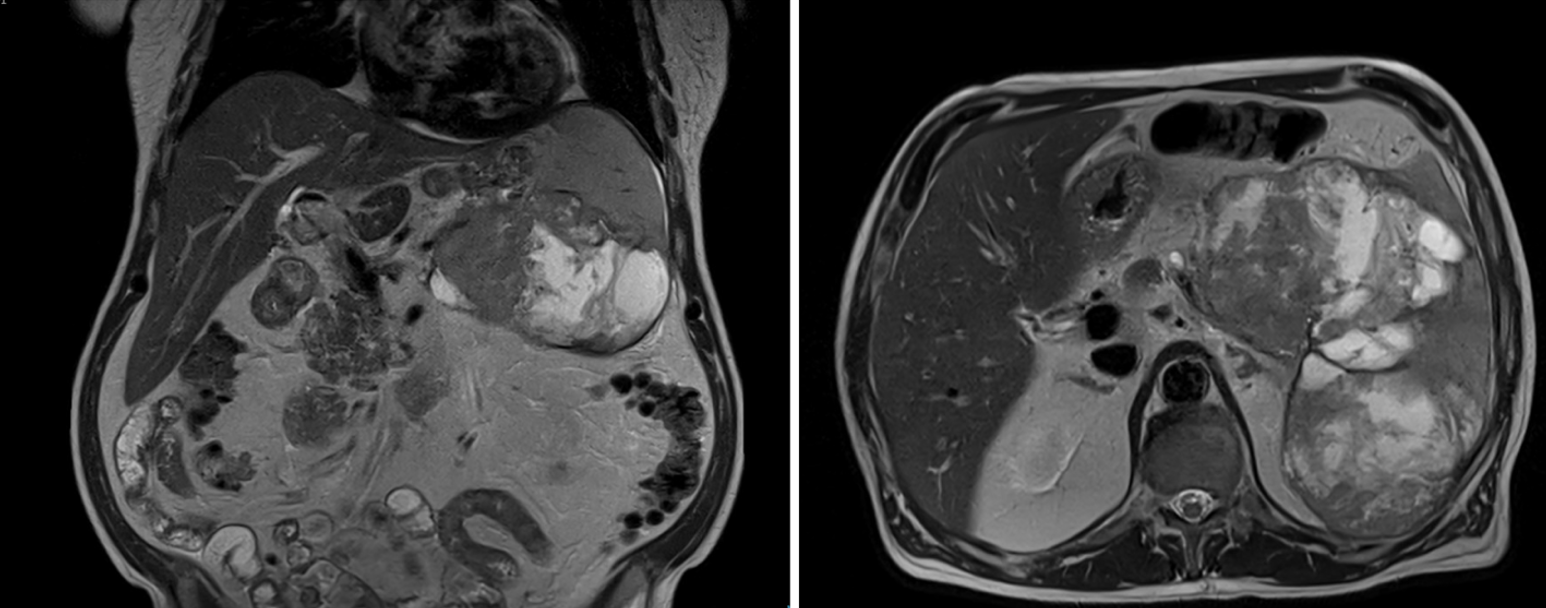
Figure: Figure 1. MRI abdomen. Large splenic cystic/solid lesion, composed of either two or three masses versus a large conglomerate mass centered within the spleen. Mass contacts the colon, stomach, and pancreas, with subtle invasion of the pancreas difficult to exclude on the study.

Figure: Figure 2. Pathology. Malignant cells with pleomorphic nuclei and keratin pearls formation (400x; H&E). P40 immunohistochemical staining, specific for squamous cell cancers, shows diffuse positive nuclear staining (100x). Noted portions of the excised squamous cell carcinoma that microscopically abuts but does not involve the pancreatic tissue (50x; H&E).
Disclosures:
Yannis Lafazanos indicated no relevant financial relationships.
Sufyan AbdulMujeeb indicated no relevant financial relationships.
Asif Lakha indicated no relevant financial relationships.
Nahren Asado indicated no relevant financial relationships.
Eli Ehrenpreis: E2Bio Consultants – Intellectual Property/Patents, CEO, Owner/Ownership Interest. E2Bio Life Sciences – CEO, Owner/Ownership Interest.
Yannis S. Lafazanos, DO1, Sufyan AbdulMujeeb, DO2, Asif Lakha, MD3, Nahren Asado, MD3, Eli Ehrenpreis, MD, FACG2. P4512 - A Pancreas's Tail, a Spleen's Hilum, and a Squamous Cell Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Advocate Lutheran General, Long Grove, IL; 2Advocate Lutheran General, Park Ridge, IL; 3Advocate Lutheran General Hospital, Park Ridge, IL
Introduction: Primary squamous cell carcinoma of the pancreas (SCCP) is an extremely rare clinical entity, comprising anywhere between 0.5 to 5% of all pancreatic malignancies, with rising incidence. Pancreatic tissue, normally devoid of squamous cells, must undergo squamous metaplastic changes of its columnar ductal cells, either secondary to inflammation or within a pre-existing adenocarcinoma. Clinical data is poor for SCCP, with diagnostic pathways and treatment options limited, making this area ripe for standardization.
Case Description/
Methods: Our patient is a 76-year-old male with no significant past medical history who presented to his primary care physician’s office with a 4-month history of unintentional weight loss and left upper quadrant abdominal pain. He also noticed anorexia, early satiety, and night sweats. Examination was only notable for splenomegaly. Comprehensive metabolic panel was normal. MRI abdomen showed a large splenic cystic/solid lesion with possible invasion of the pancreas (Figure 1). GI was consulted for EUS with FNA of the left upper quadrant mass, which resulted in multiple biopsies along the splenic hilum and pancreatic tail. Pathology only showed rare, atypical changes, without a clear diagnosis. A few weeks later, he was evaluated by surgical oncology and taken to the OR for removal of a 17 cm tumor with distal pancreatectomy, splenectomy, omentectomy and transverse colon resection, positive for squamous cell carcinoma of the pancreas (Figure 2). He is currently undergoing adjuvant chemotherapy.
Discussion: For our patient, a SCCP that quickly metastasized from the pancreatic tail to the hilar spleen promoted confounding symptoms derived from splenic involvement. EUS with FNA of this splenic lesion was productive of nondiagnostic pathology, despite multiple sites biopsied, likely resultant of cystic aspiration, and points to the difficulty of transgastric biopsy of the left upper quadrant. Typically, MRI imaging and surgical intervention, at least in early-stage cancers, are the most common management strategies amongst the roughly 50 cases of SCCP present in the literature.
The gastroenterologist also has a role in mediating risk factors for SCCP, including mitigation of inflammatory states, like chronic pancreatitis, and careful pancreatic duct intervention, mostly related to stent placement, which have been implicated in many of the cases reviewed for this report. Our case should serve as further example for the need for continued clinical study of SCCP.
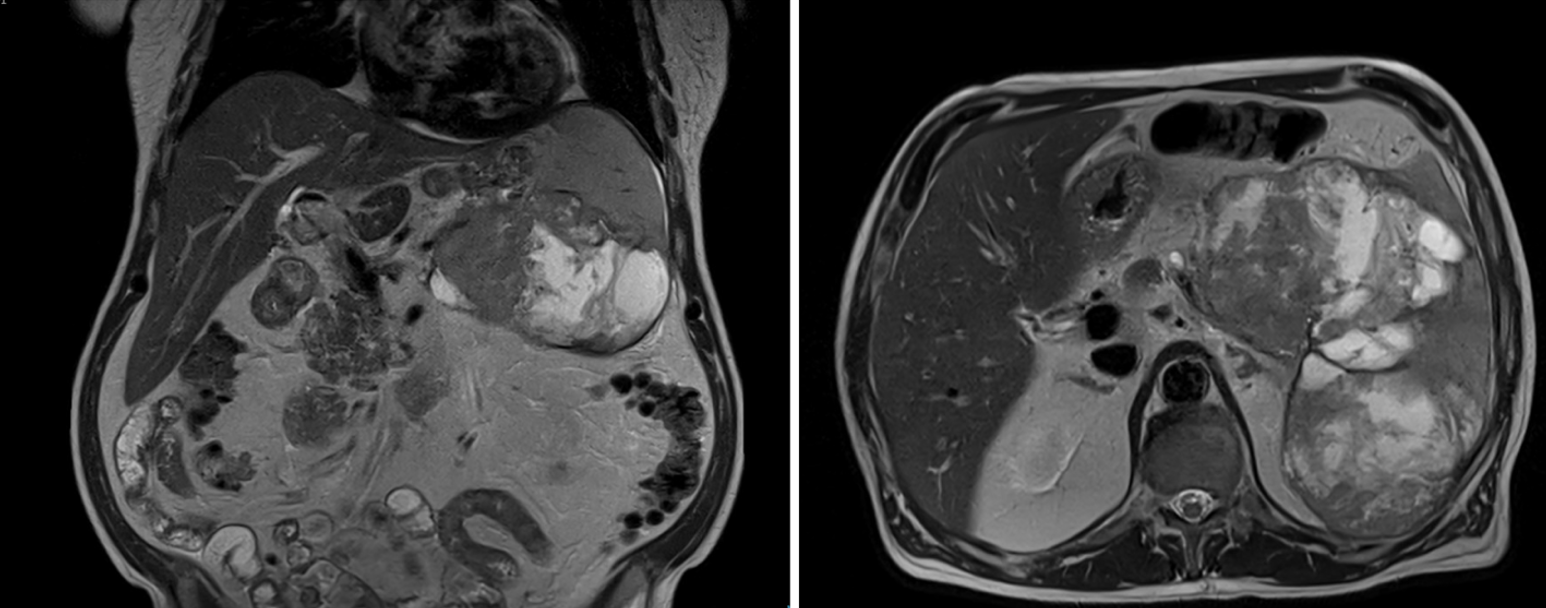
Figure: Figure 1. MRI abdomen. Large splenic cystic/solid lesion, composed of either two or three masses versus a large conglomerate mass centered within the spleen. Mass contacts the colon, stomach, and pancreas, with subtle invasion of the pancreas difficult to exclude on the study.

Figure: Figure 2. Pathology. Malignant cells with pleomorphic nuclei and keratin pearls formation (400x; H&E). P40 immunohistochemical staining, specific for squamous cell cancers, shows diffuse positive nuclear staining (100x). Noted portions of the excised squamous cell carcinoma that microscopically abuts but does not involve the pancreatic tissue (50x; H&E).
Disclosures:
Yannis Lafazanos indicated no relevant financial relationships.
Sufyan AbdulMujeeb indicated no relevant financial relationships.
Asif Lakha indicated no relevant financial relationships.
Nahren Asado indicated no relevant financial relationships.
Eli Ehrenpreis: E2Bio Consultants – Intellectual Property/Patents, CEO, Owner/Ownership Interest. E2Bio Life Sciences – CEO, Owner/Ownership Interest.
Yannis S. Lafazanos, DO1, Sufyan AbdulMujeeb, DO2, Asif Lakha, MD3, Nahren Asado, MD3, Eli Ehrenpreis, MD, FACG2. P4512 - A Pancreas's Tail, a Spleen's Hilum, and a Squamous Cell Cancer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
