Tuesday Poster Session
Category: Biliary/Pancreas
P4511 - Dapagliflozin-Induced Necrotizing Pancreatitis: A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amine Rakab, MD (he/him/his)
Division of Medical Education, Weill Cornell Medicine
Doha, Ad Dawhah, Qatar
Presenting Author(s)
Rida Naqvi, BS1, Bisher Sawaf, MD2, Zohaib Ahmed, MD3, Yusuf Omar Hallak, MD1, Kiya Shazadeh Safavi, MD1, Amine Rakab, MD4, Abdallah Kobeissy, MD, MPH1, Ali Nawras, MD1
1The University of Toledo, Toledo, OH; 2University of Toledo Medical Center, Toledo, OH; 3University of Toledo College Medicine and Life Sciences, Toledo, OH; 4Division of Medical Education, Weill Cornell Medicine, Doha, Ad Dawhah, Qatar
Introduction: Necrotizing pancreatitis, a severe form of acute pancreatitis, involves pancreatic tissue death and may lead to systemic complications requiring intensive care. Sodium-glucose co-transporter 2 (SGLT-2) inhibitors, such as dapagliflozin, are used to manage type 2 diabetes, chronic kidney disease, and heart failure. While generally safe, rare instances of acute pancreatitis have been reported with SGLT-2 inhibitor use. This report discusses a case of necrotizing pancreatitis potentially induced by dapagliflozin.
Case Description/
Methods: A 72-year-old woman with insulin-dependent type 2 diabetes, coronary artery disease, stage 2 chronic kidney disease, and nonalcoholic steatohepatitis presented with hematemesis. Her medications included dapagliflozin, initiated approximately two weeks prior. She denied alcohol use, recent trauma, or gallstones. Laboratory tests revealed a lipase level of 16,600 U/L, an anion gap of 23, and a white blood cell count of 24,000/μL. Imaging confirmed acute interstitial edematous pancreatitis without biliary obstruction. Despite initial improvement with antibiotics, she was readmitted a week later with worsening symptoms. Imaging showed bilateral pleural effusions and necrotizing pancreatitis. She underwent endoscopic retrograde cholangiopancreatography (ERCP) with stent placement and necrosectomy. Cultures grew multidrug-resistant Enterococcus faecium. After further interventions, including additional necrosectomies and antibiotic therapy, her condition stabilized, and she was discharged to a skilled nursing facility.
Discussion: This case highlights a rare instance of necrotizing pancreatitis potentially associated with dapagliflozin use. The exact mechanism by which SGLT-2 inhibitors might induce pancreatitis is unclear. Proposed theories include drug-induced dehydration leading to lactic acidosis, alterations in insulin and glucagon levels promoting ketosis, and idiosyncratic immune or cytotoxic reactions. While large-scale studies have not established a definitive link between SGLT-2 inhibitors and pancreatitis, isolated case reports suggest a possible association. Clinicians should remain vigilant for signs of pancreatitis in patients initiating SGLT-2 inhibitors and consider discontinuation if symptoms arise. Further research is needed to elucidate the relationship between SGLT-2 inhibitors and pancreatic inflammation.
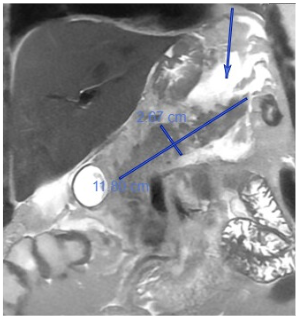
Figure: Image 1: MRI demonstrated no evidence of underlying pancreatic mass, however confirmed acute pancreatitis with non-enhancing tissue (indicating necrosis) with blood products within the pancreatic body. Additionally foci of non-enhancement were noted, indicating additional devitalized tissue at risk of necrosis and further hemorrhage. Arrow indicates fat stranding.
Disclosures:
Rida Naqvi indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Zohaib Ahmed indicated no relevant financial relationships.
Yusuf Omar Hallak indicated no relevant financial relationships.
Kiya Shazadeh Safavi indicated no relevant financial relationships.
Amine Rakab indicated no relevant financial relationships.
Abdallah Kobeissy indicated no relevant financial relationships.
Ali Nawras indicated no relevant financial relationships.
Rida Naqvi, BS1, Bisher Sawaf, MD2, Zohaib Ahmed, MD3, Yusuf Omar Hallak, MD1, Kiya Shazadeh Safavi, MD1, Amine Rakab, MD4, Abdallah Kobeissy, MD, MPH1, Ali Nawras, MD1. P4511 - Dapagliflozin-Induced Necrotizing Pancreatitis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The University of Toledo, Toledo, OH; 2University of Toledo Medical Center, Toledo, OH; 3University of Toledo College Medicine and Life Sciences, Toledo, OH; 4Division of Medical Education, Weill Cornell Medicine, Doha, Ad Dawhah, Qatar
Introduction: Necrotizing pancreatitis, a severe form of acute pancreatitis, involves pancreatic tissue death and may lead to systemic complications requiring intensive care. Sodium-glucose co-transporter 2 (SGLT-2) inhibitors, such as dapagliflozin, are used to manage type 2 diabetes, chronic kidney disease, and heart failure. While generally safe, rare instances of acute pancreatitis have been reported with SGLT-2 inhibitor use. This report discusses a case of necrotizing pancreatitis potentially induced by dapagliflozin.
Case Description/
Methods: A 72-year-old woman with insulin-dependent type 2 diabetes, coronary artery disease, stage 2 chronic kidney disease, and nonalcoholic steatohepatitis presented with hematemesis. Her medications included dapagliflozin, initiated approximately two weeks prior. She denied alcohol use, recent trauma, or gallstones. Laboratory tests revealed a lipase level of 16,600 U/L, an anion gap of 23, and a white blood cell count of 24,000/μL. Imaging confirmed acute interstitial edematous pancreatitis without biliary obstruction. Despite initial improvement with antibiotics, she was readmitted a week later with worsening symptoms. Imaging showed bilateral pleural effusions and necrotizing pancreatitis. She underwent endoscopic retrograde cholangiopancreatography (ERCP) with stent placement and necrosectomy. Cultures grew multidrug-resistant Enterococcus faecium. After further interventions, including additional necrosectomies and antibiotic therapy, her condition stabilized, and she was discharged to a skilled nursing facility.
Discussion: This case highlights a rare instance of necrotizing pancreatitis potentially associated with dapagliflozin use. The exact mechanism by which SGLT-2 inhibitors might induce pancreatitis is unclear. Proposed theories include drug-induced dehydration leading to lactic acidosis, alterations in insulin and glucagon levels promoting ketosis, and idiosyncratic immune or cytotoxic reactions. While large-scale studies have not established a definitive link between SGLT-2 inhibitors and pancreatitis, isolated case reports suggest a possible association. Clinicians should remain vigilant for signs of pancreatitis in patients initiating SGLT-2 inhibitors and consider discontinuation if symptoms arise. Further research is needed to elucidate the relationship between SGLT-2 inhibitors and pancreatic inflammation.
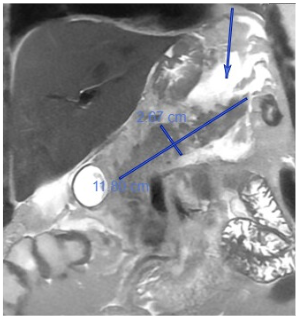
Figure: Image 1: MRI demonstrated no evidence of underlying pancreatic mass, however confirmed acute pancreatitis with non-enhancing tissue (indicating necrosis) with blood products within the pancreatic body. Additionally foci of non-enhancement were noted, indicating additional devitalized tissue at risk of necrosis and further hemorrhage. Arrow indicates fat stranding.
Disclosures:
Rida Naqvi indicated no relevant financial relationships.
Bisher Sawaf indicated no relevant financial relationships.
Zohaib Ahmed indicated no relevant financial relationships.
Yusuf Omar Hallak indicated no relevant financial relationships.
Kiya Shazadeh Safavi indicated no relevant financial relationships.
Amine Rakab indicated no relevant financial relationships.
Abdallah Kobeissy indicated no relevant financial relationships.
Ali Nawras indicated no relevant financial relationships.
Rida Naqvi, BS1, Bisher Sawaf, MD2, Zohaib Ahmed, MD3, Yusuf Omar Hallak, MD1, Kiya Shazadeh Safavi, MD1, Amine Rakab, MD4, Abdallah Kobeissy, MD, MPH1, Ali Nawras, MD1. P4511 - Dapagliflozin-Induced Necrotizing Pancreatitis: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
