Tuesday Poster Session
Category: Biliary/Pancreas
P4506 - A Diagnostic Detour: Acute Pancreatitis Revealing Hidden Synchronous Gastric and Pancreatic Neuroendocrine Tumors (NETs)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Panida Charnvitayapong, MD (she/her/hers)
University of Miami Miller School of Medicine at JFK Medical Center
Atlantis, FL
Presenting Author(s)
Panida Charnvitayapong, MD1, Bebika Subedi, MD1, Kayode Olowe, MD2
1University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL; 2HCA Florida Healthcare, Atlantis, FL
Introduction: Neuroendocrine tumors (NETs) are rare, heterogeneous neoplasms that can arise from various organs. They usually present either as asymptomatic nonfunctional tumors or as functional tumors causing hormone-related symptoms. Here, we describe an unusual instance of synchronous pancreatic and gastric NETs initially diagnosed as necrotizing pancreatitis.
Case Description/
Methods: A 37-year-old woman with no medical history presented to an outside hospital with epigastric pain, nausea, and bilious vomiting, similar to a prior self-resolving episode. Imaging studies (CT and MRI) demonstrated numerous pancreatic cysts suspicious for malignancy but led to a diagnosis of acute pancreatitis. After persistent symptoms, she arrived at our ED. She denied any diarrhea, alcohol and drug use, chronic NSAID use, or family history of autoimmune disease. Repeat CT revealed near-complete pancreas replacement by fluid-density lesions, the largest measuring 4.1 x 3.7 cm—raising concern for necrotizing pancreatitis. Labs showed leukocytosis (14.9), increased triglycerides (338), normal LFTs, glucose, and lipase. Tumor markers (CEA, CA 19-9) and autoimmune/infectious workups were negative.
The patient underwent endoscopic ultrasound (EUS) and esophagogastroduodenoscopy (EGD). Endoscopy revealed multiple small gastric polyps, some of which were removed. EUS showed a pancreas nearly replaced by cystic lesions. Fine needle aspiration (FNA) of pancreatic tissue and cyst fluid was performed, and MRCP was remarkable for cysts and large gastric varices likely due to splenic vein occlusion.
Gastric biopsy results indicated a well-differentiated gastric NET, WHO grade 2, with a Ki-67 index of 5–8%. Cytology from the pancreatic tail showed a well-differentiated NET, WHO grade 1, with Ki-67 of 1%. Due to extensive pancreatic involvement, total pancreatectomy was recommended, and she was referred to a tertiary center for further management.
Discussion: NETs are classified by their degree of histological/morphological differentiation (WHO classification) and graded cell proliferation (Ki67 index). Risk factors include genetic predisposition, diabetes, obesity, smoking, and alcohol use. Surgical intervention remains the primary treatment, while systemic therapies (i.e. SSAs, everolimus) are used for metastatic or unresectable cases.
In patients with unexplained abdominal pain and pancreatic cystic lesions—especially in the absence of typical risk factors—NETs should be considered to enable early diagnosis and appropriate management.
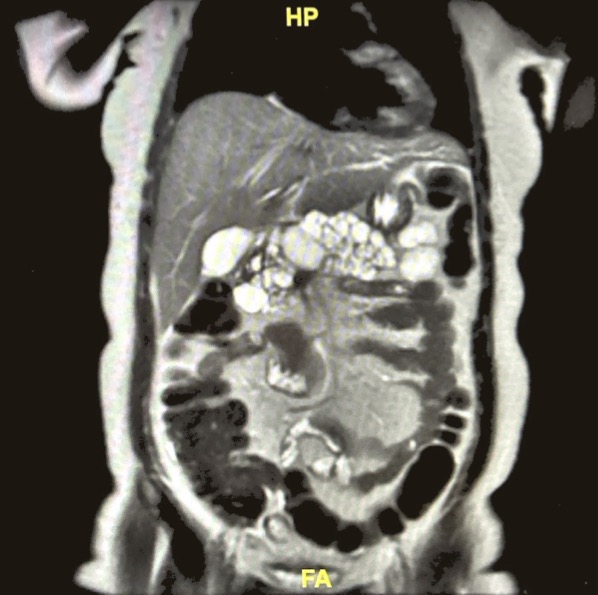
Figure: CT abdomen/pelvis (axial): Near complete replacement of the pancreatic bed with innumerable fluid density lesions largest measuring 4.1 x 3.7cm
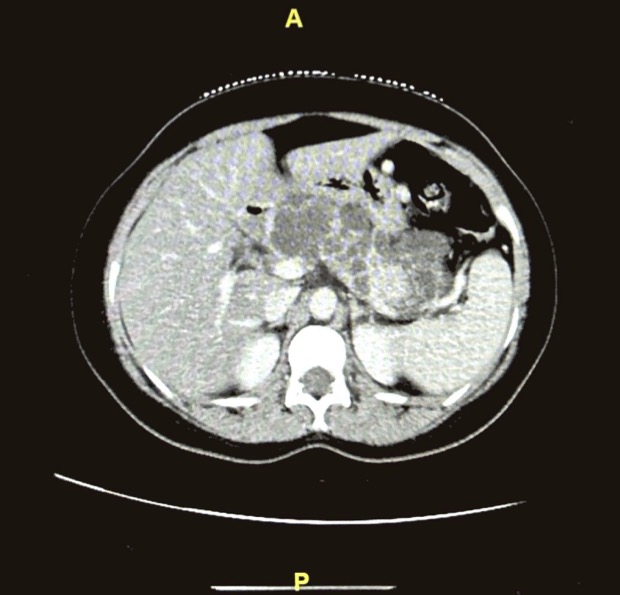
Figure: MRCP (Coronal): Innumerable varying-sized cysts throughout the pancreas essentially replacing entire pancreatic parenchyma
Disclosures:
Panida Charnvitayapong indicated no relevant financial relationships.
Bebika Subedi indicated no relevant financial relationships.
Kayode Olowe indicated no relevant financial relationships.
Panida Charnvitayapong, MD1, Bebika Subedi, MD1, Kayode Olowe, MD2. P4506 - A Diagnostic Detour: Acute Pancreatitis Revealing Hidden Synchronous Gastric and Pancreatic Neuroendocrine Tumors (NETs), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Miami Miller School of Medicine at JFK Medical Center, Atlantis, FL; 2HCA Florida Healthcare, Atlantis, FL
Introduction: Neuroendocrine tumors (NETs) are rare, heterogeneous neoplasms that can arise from various organs. They usually present either as asymptomatic nonfunctional tumors or as functional tumors causing hormone-related symptoms. Here, we describe an unusual instance of synchronous pancreatic and gastric NETs initially diagnosed as necrotizing pancreatitis.
Case Description/
Methods: A 37-year-old woman with no medical history presented to an outside hospital with epigastric pain, nausea, and bilious vomiting, similar to a prior self-resolving episode. Imaging studies (CT and MRI) demonstrated numerous pancreatic cysts suspicious for malignancy but led to a diagnosis of acute pancreatitis. After persistent symptoms, she arrived at our ED. She denied any diarrhea, alcohol and drug use, chronic NSAID use, or family history of autoimmune disease. Repeat CT revealed near-complete pancreas replacement by fluid-density lesions, the largest measuring 4.1 x 3.7 cm—raising concern for necrotizing pancreatitis. Labs showed leukocytosis (14.9), increased triglycerides (338), normal LFTs, glucose, and lipase. Tumor markers (CEA, CA 19-9) and autoimmune/infectious workups were negative.
The patient underwent endoscopic ultrasound (EUS) and esophagogastroduodenoscopy (EGD). Endoscopy revealed multiple small gastric polyps, some of which were removed. EUS showed a pancreas nearly replaced by cystic lesions. Fine needle aspiration (FNA) of pancreatic tissue and cyst fluid was performed, and MRCP was remarkable for cysts and large gastric varices likely due to splenic vein occlusion.
Gastric biopsy results indicated a well-differentiated gastric NET, WHO grade 2, with a Ki-67 index of 5–8%. Cytology from the pancreatic tail showed a well-differentiated NET, WHO grade 1, with Ki-67 of 1%. Due to extensive pancreatic involvement, total pancreatectomy was recommended, and she was referred to a tertiary center for further management.
Discussion: NETs are classified by their degree of histological/morphological differentiation (WHO classification) and graded cell proliferation (Ki67 index). Risk factors include genetic predisposition, diabetes, obesity, smoking, and alcohol use. Surgical intervention remains the primary treatment, while systemic therapies (i.e. SSAs, everolimus) are used for metastatic or unresectable cases.
In patients with unexplained abdominal pain and pancreatic cystic lesions—especially in the absence of typical risk factors—NETs should be considered to enable early diagnosis and appropriate management.
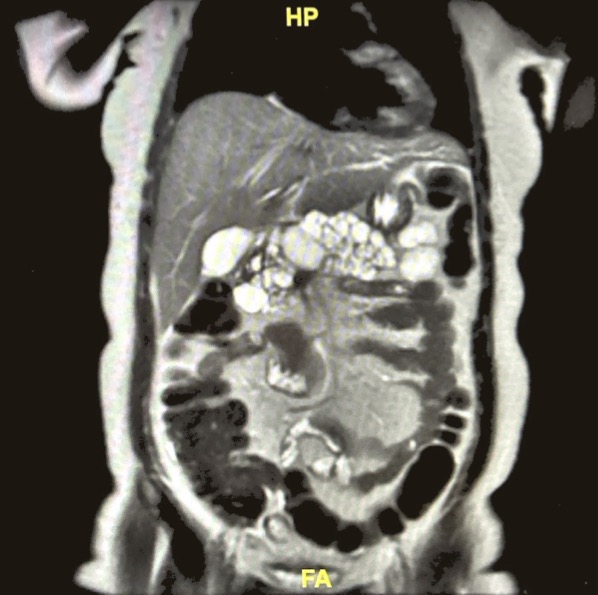
Figure: CT abdomen/pelvis (axial): Near complete replacement of the pancreatic bed with innumerable fluid density lesions largest measuring 4.1 x 3.7cm
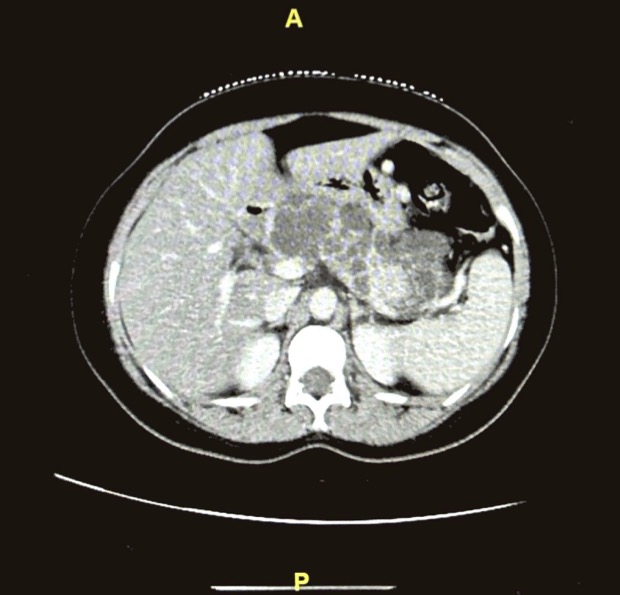
Figure: MRCP (Coronal): Innumerable varying-sized cysts throughout the pancreas essentially replacing entire pancreatic parenchyma
Disclosures:
Panida Charnvitayapong indicated no relevant financial relationships.
Bebika Subedi indicated no relevant financial relationships.
Kayode Olowe indicated no relevant financial relationships.
Panida Charnvitayapong, MD1, Bebika Subedi, MD1, Kayode Olowe, MD2. P4506 - A Diagnostic Detour: Acute Pancreatitis Revealing Hidden Synchronous Gastric and Pancreatic Neuroendocrine Tumors (NETs), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
