Tuesday Poster Session
Category: Biliary/Pancreas
P4471 - Beyond the Scope: A Rare Splenic Artery-Pancreatic Duct Fistula Diagnosed After Exhaustive Evaluation [Hemosuccus Pancreaticus]
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MK
Meghana Kakarla, MD
Infirmary Health
Mobile, AL
Presenting Author(s)
Meghana Kakarla, MD, Bennett S. Hooks, MD
Infirmary Health, Mobile, AL
Introduction: Hemosuccus pancreaticus (HP) is a rare and challenging cause of gastrointestinal (GI) bleeding due to hemorrhage into the pancreatic duct, most often from a ruptured pseudoaneurysm. We present an exceptionally rare subtype: a direct fistula between the splenic artery and pancreatic duct, without pseudoaneurysm or pseudocyst formation—described in fewer than 5% of HP cases
Case Description/
Methods: A 60-year-old man who had alcohol-related chronic pancreatitis, previous gastric ulcer repair, type 2 diabetes and previous DVT without anticoagulation presented with recurrent hematochezia, fatigue, and a hemoglobin level of 4.7 g/dL. He had an extensive but nondiagnostic evaluation over two years that included four EGDs, two colonoscopies, a capsule endoscopy, a Meckel scan, two CT angiographies (CTA) and two nuclear RBC-tagged bleeding scans. The patient received 23 units of packed red blood cells during the latest admission but the bleeding source was not identified. During an active bleeding episode, the third CTA revealed a fistulous connection that directly linked the splenic artery to the pancreatic duct. The patient received endovascular coil embolization of the splenic artery which resulted in no additional bleeding and his hemoglobin levels stabilized at one-month follow-up.
Discussion: On average, patients with HP undergo 2–6 endoscopic procedures and multiple imaging studies before diagnosis, particularly when bleeding is intermittent. This case emphasizes the need for heightened clinical suspicion in patients with alcohol-related chronic pancreatitis and recurrent, transfusion-dependent lower GI bleeding. active bleeding and definitive endovascular coil embolization are crucial to achieving hemostasis and avoiding surgical morbidity.
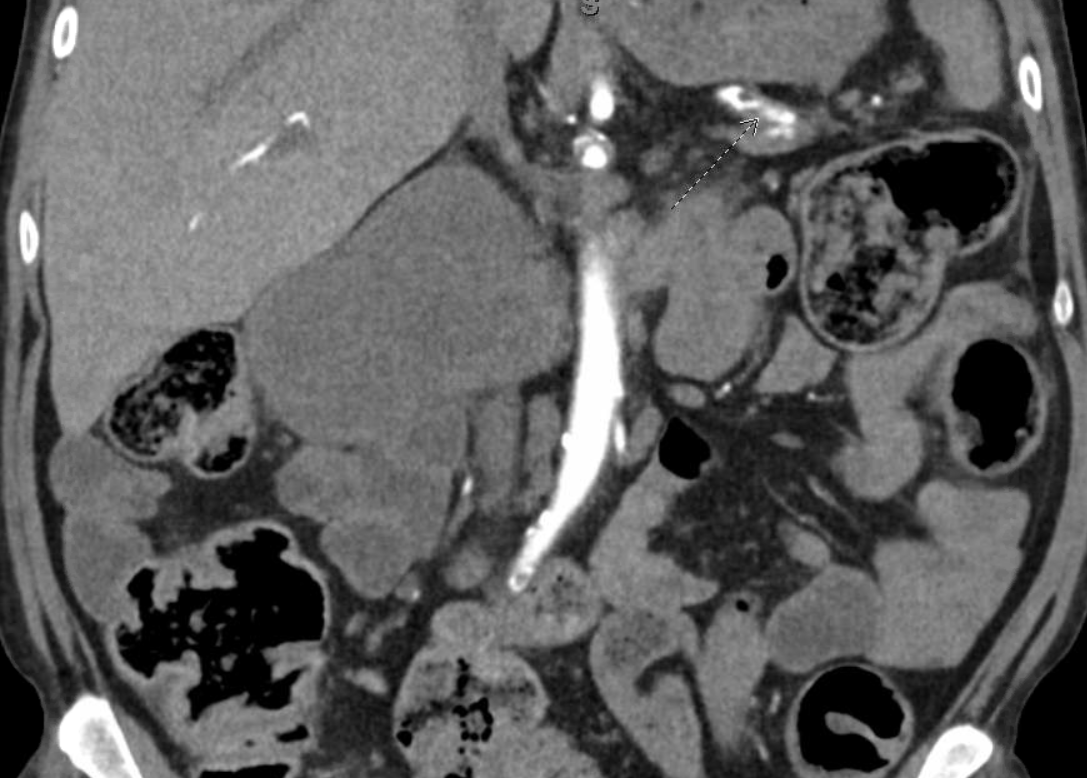
Figure: Coronal arterial phase CT angiogram demonstrating an aberrant arterial course suggestive of a direct splenic artery to pancreatic duct fistula. The splenic artery appears to course closely along the pancreas with contrast tracking toward the expected location of the pancreatic duct (dashed arrow). There is no evidence of a pseudoaneurysm or pseudocyst, distinguishing this rare presentation from more typical causes of hemosuccus pancreaticus. These findings are suggestive of a direct arterio-ductal communication.

Figure: Axial arterial phase CT demonstrating an aberrant course of the splenic artery with close approximation to the pancreatic duct. There is contrast enhancement within the expected region of the pancreatic duct, raising suspicion for a direct arterio-ductal fistulous communication. No pseudoaneurysm or pseudocyst is seen. Findings are suggestive of a rare direct splenic artery to pancreatic duct fistula, a variant of hemosuccus pancreaticus.
Disclosures:
Meghana Kakarla indicated no relevant financial relationships.
Bennett Hooks indicated no relevant financial relationships.
Meghana Kakarla, MD, Bennett S. Hooks, MD. P4471 - Beyond the Scope: A Rare Splenic Artery-Pancreatic Duct Fistula Diagnosed After Exhaustive Evaluation [Hemosuccus Pancreaticus], ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Infirmary Health, Mobile, AL
Introduction: Hemosuccus pancreaticus (HP) is a rare and challenging cause of gastrointestinal (GI) bleeding due to hemorrhage into the pancreatic duct, most often from a ruptured pseudoaneurysm. We present an exceptionally rare subtype: a direct fistula between the splenic artery and pancreatic duct, without pseudoaneurysm or pseudocyst formation—described in fewer than 5% of HP cases
Case Description/
Methods: A 60-year-old man who had alcohol-related chronic pancreatitis, previous gastric ulcer repair, type 2 diabetes and previous DVT without anticoagulation presented with recurrent hematochezia, fatigue, and a hemoglobin level of 4.7 g/dL. He had an extensive but nondiagnostic evaluation over two years that included four EGDs, two colonoscopies, a capsule endoscopy, a Meckel scan, two CT angiographies (CTA) and two nuclear RBC-tagged bleeding scans. The patient received 23 units of packed red blood cells during the latest admission but the bleeding source was not identified. During an active bleeding episode, the third CTA revealed a fistulous connection that directly linked the splenic artery to the pancreatic duct. The patient received endovascular coil embolization of the splenic artery which resulted in no additional bleeding and his hemoglobin levels stabilized at one-month follow-up.
Discussion: On average, patients with HP undergo 2–6 endoscopic procedures and multiple imaging studies before diagnosis, particularly when bleeding is intermittent. This case emphasizes the need for heightened clinical suspicion in patients with alcohol-related chronic pancreatitis and recurrent, transfusion-dependent lower GI bleeding. active bleeding and definitive endovascular coil embolization are crucial to achieving hemostasis and avoiding surgical morbidity.
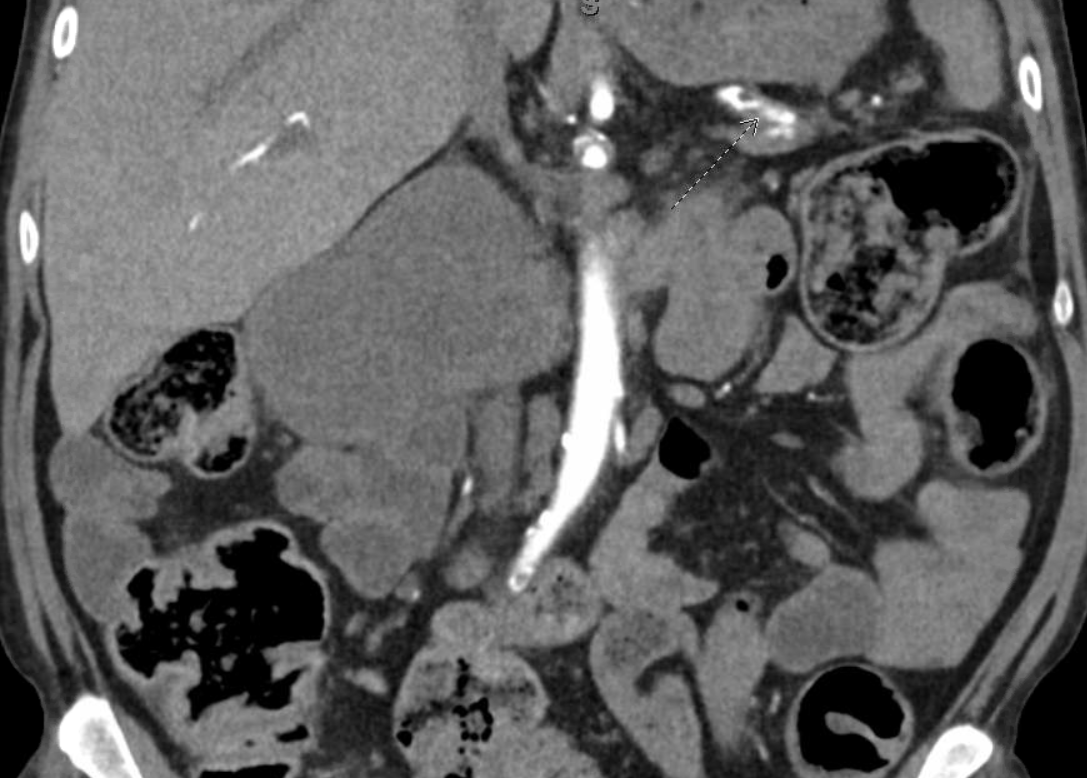
Figure: Coronal arterial phase CT angiogram demonstrating an aberrant arterial course suggestive of a direct splenic artery to pancreatic duct fistula. The splenic artery appears to course closely along the pancreas with contrast tracking toward the expected location of the pancreatic duct (dashed arrow). There is no evidence of a pseudoaneurysm or pseudocyst, distinguishing this rare presentation from more typical causes of hemosuccus pancreaticus. These findings are suggestive of a direct arterio-ductal communication.

Figure: Axial arterial phase CT demonstrating an aberrant course of the splenic artery with close approximation to the pancreatic duct. There is contrast enhancement within the expected region of the pancreatic duct, raising suspicion for a direct arterio-ductal fistulous communication. No pseudoaneurysm or pseudocyst is seen. Findings are suggestive of a rare direct splenic artery to pancreatic duct fistula, a variant of hemosuccus pancreaticus.
Disclosures:
Meghana Kakarla indicated no relevant financial relationships.
Bennett Hooks indicated no relevant financial relationships.
Meghana Kakarla, MD, Bennett S. Hooks, MD. P4471 - Beyond the Scope: A Rare Splenic Artery-Pancreatic Duct Fistula Diagnosed After Exhaustive Evaluation [Hemosuccus Pancreaticus], ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
