Tuesday Poster Session
Category: Biliary/Pancreas
P4468 - Microvascular Ischemic Injury to the Biliary Tree: A Rare Case of Sickle Cell Ischemic Cholangiopathy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Fawaz Hussain, MD
Wayne State University School of Medicine / Detroit Medical Center
Detroit, MI
Presenting Author(s)
Fawaz Hussain, MD1, Maryam Zaffer, BA2, Aabid Mohiuddin, DO1, Shefali Godara, MD1, Karan Mathur, MD1
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Nova Southeastern University, Clearwater, FL
Introduction: Sickle cell disease (SCD) is known to cause ischemic injury across multiple organ systems. However, ischemic injury to the biliary tree is exceedingly rare, occurring in fewer than 1% of SCD cases. Risk factors include homozygous (HbSS) SCD, advanced age, frequent vaso-occlusive episodes, liver fibrosis, and repeated blood transfusions. The case below illustrates a rare presentation of sickle cell ischemic cholangiopathy (SCIC) and hepatic non-caseating granulomas due to microvascular occlusion.
Case Description/
Methods: A 41-year-old female with a history of HbSS SCD and cholecystectomy was admitted for acute hypoxic respiratory failure due to acute chest syndrome, ultimately requiring mechanical ventilation. A month into her hospitalization, she developed right upper quadrant abdominal pain with newly elevated alkaline phosphatase which peaked at 1873 U/L, gamma-glutamyl transferase 948 U/L, and total bilirubin up to 7.6 mg/dL (primarily conjugated); AST and ALT remained within < 1.5x ULN. Her cholestatic liver injury worsened despite discontinuing hepatotoxic medications and resolution of sepsis. Serologic testing for all viral and autoimmune etiologies was negative. MRCP showed chronic hemosiderosis without biliary obstruction. Liver biopsy revealed sinusoidal congestion with sickled red blood cells, Kupffer cell hyperplasia, and small non-caseating granulomas. The hepatic granulomas were attributed to sickle cell hepatopathy since there was no evidence of systemic sarcoidosis, tuberculosis, brucellosis or iatrogenic etiology. Given the exclusion of other etiologies, her cholestatic liver injury was attributed to acute SCIC. She was initiated on ursodiol 13 mg/kg/day and underwent an exchange transfusion with subsequent improvement of alkaline phosphatase to 359 U/L and total bilirubin 0.81 mg/dL over a period of two weeks. However, prior to complete resolution, the patient was transitioned to hospice care and died shortly after palliative extubation.
Discussion: The biliary tree is particularly susceptible to ischemic injury in SCD due to its sole blood supply from small arteriolar branches of the hepatic artery. Exchange transfusions remain key in reducing the proportion of sickled erythrocytes to less than 20-30%; ursodiol may also provide benefit as seen in this case, however its role in SCIC is currently understudied. Further clinical guidance is needed to optimize the timely diagnosis and management of SCIC and minimize complications, especially in critically ill patients.
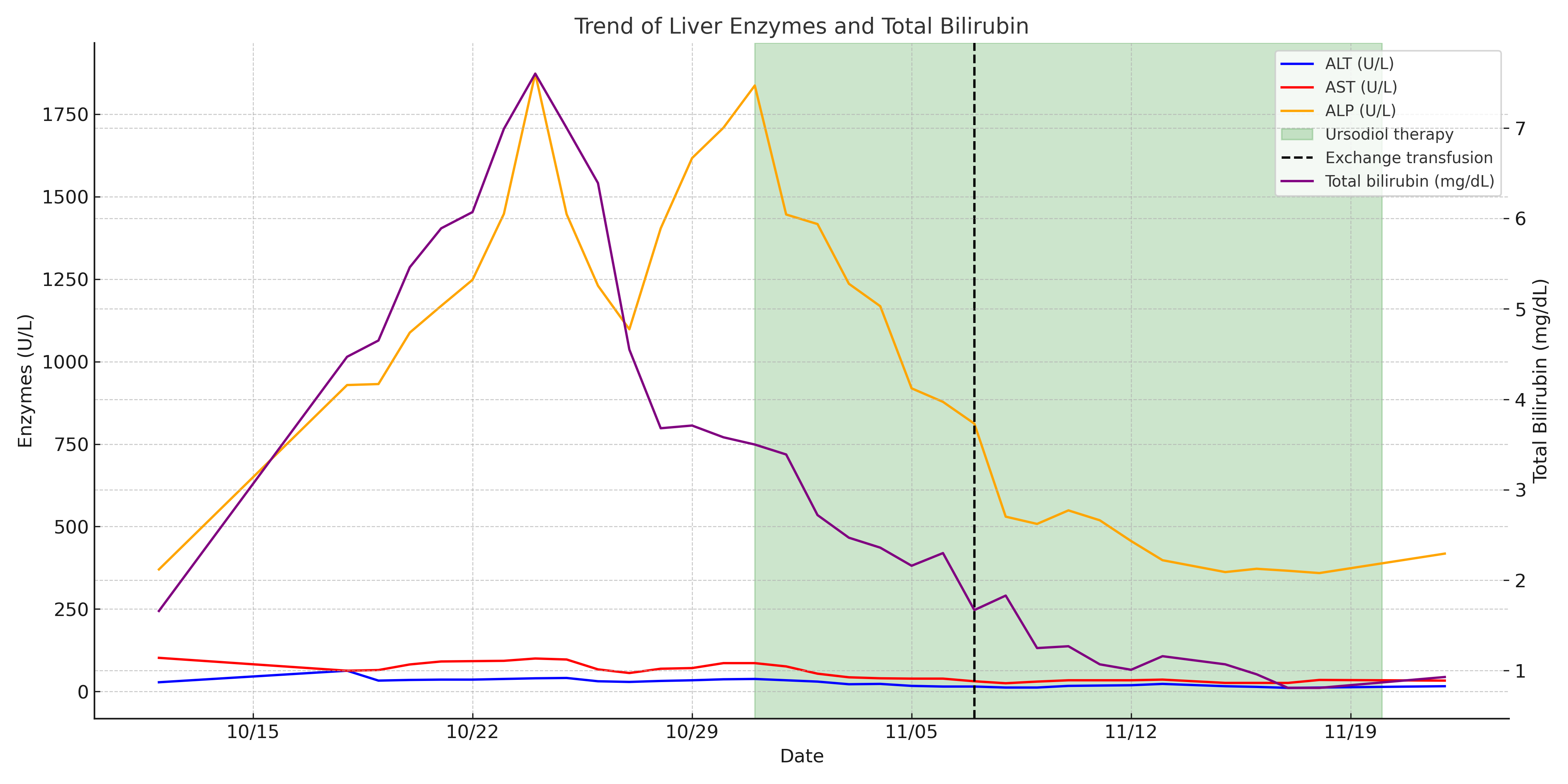
Figure: Temporal trend in serum liver enzymes, including alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and total bilirubin. A progressive decline in serum ALP was noted following the initiation of ursodiol and continued after exchange transfusion.
Disclosures:
Fawaz Hussain indicated no relevant financial relationships.
Maryam Zaffer indicated no relevant financial relationships.
Aabid Mohiuddin indicated no relevant financial relationships.
Shefali Godara indicated no relevant financial relationships.
Karan Mathur indicated no relevant financial relationships.
Fawaz Hussain, MD1, Maryam Zaffer, BA2, Aabid Mohiuddin, DO1, Shefali Godara, MD1, Karan Mathur, MD1. P4468 - Microvascular Ischemic Injury to the Biliary Tree: A Rare Case of Sickle Cell Ischemic Cholangiopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 2Nova Southeastern University, Clearwater, FL
Introduction: Sickle cell disease (SCD) is known to cause ischemic injury across multiple organ systems. However, ischemic injury to the biliary tree is exceedingly rare, occurring in fewer than 1% of SCD cases. Risk factors include homozygous (HbSS) SCD, advanced age, frequent vaso-occlusive episodes, liver fibrosis, and repeated blood transfusions. The case below illustrates a rare presentation of sickle cell ischemic cholangiopathy (SCIC) and hepatic non-caseating granulomas due to microvascular occlusion.
Case Description/
Methods: A 41-year-old female with a history of HbSS SCD and cholecystectomy was admitted for acute hypoxic respiratory failure due to acute chest syndrome, ultimately requiring mechanical ventilation. A month into her hospitalization, she developed right upper quadrant abdominal pain with newly elevated alkaline phosphatase which peaked at 1873 U/L, gamma-glutamyl transferase 948 U/L, and total bilirubin up to 7.6 mg/dL (primarily conjugated); AST and ALT remained within < 1.5x ULN. Her cholestatic liver injury worsened despite discontinuing hepatotoxic medications and resolution of sepsis. Serologic testing for all viral and autoimmune etiologies was negative. MRCP showed chronic hemosiderosis without biliary obstruction. Liver biopsy revealed sinusoidal congestion with sickled red blood cells, Kupffer cell hyperplasia, and small non-caseating granulomas. The hepatic granulomas were attributed to sickle cell hepatopathy since there was no evidence of systemic sarcoidosis, tuberculosis, brucellosis or iatrogenic etiology. Given the exclusion of other etiologies, her cholestatic liver injury was attributed to acute SCIC. She was initiated on ursodiol 13 mg/kg/day and underwent an exchange transfusion with subsequent improvement of alkaline phosphatase to 359 U/L and total bilirubin 0.81 mg/dL over a period of two weeks. However, prior to complete resolution, the patient was transitioned to hospice care and died shortly after palliative extubation.
Discussion: The biliary tree is particularly susceptible to ischemic injury in SCD due to its sole blood supply from small arteriolar branches of the hepatic artery. Exchange transfusions remain key in reducing the proportion of sickled erythrocytes to less than 20-30%; ursodiol may also provide benefit as seen in this case, however its role in SCIC is currently understudied. Further clinical guidance is needed to optimize the timely diagnosis and management of SCIC and minimize complications, especially in critically ill patients.
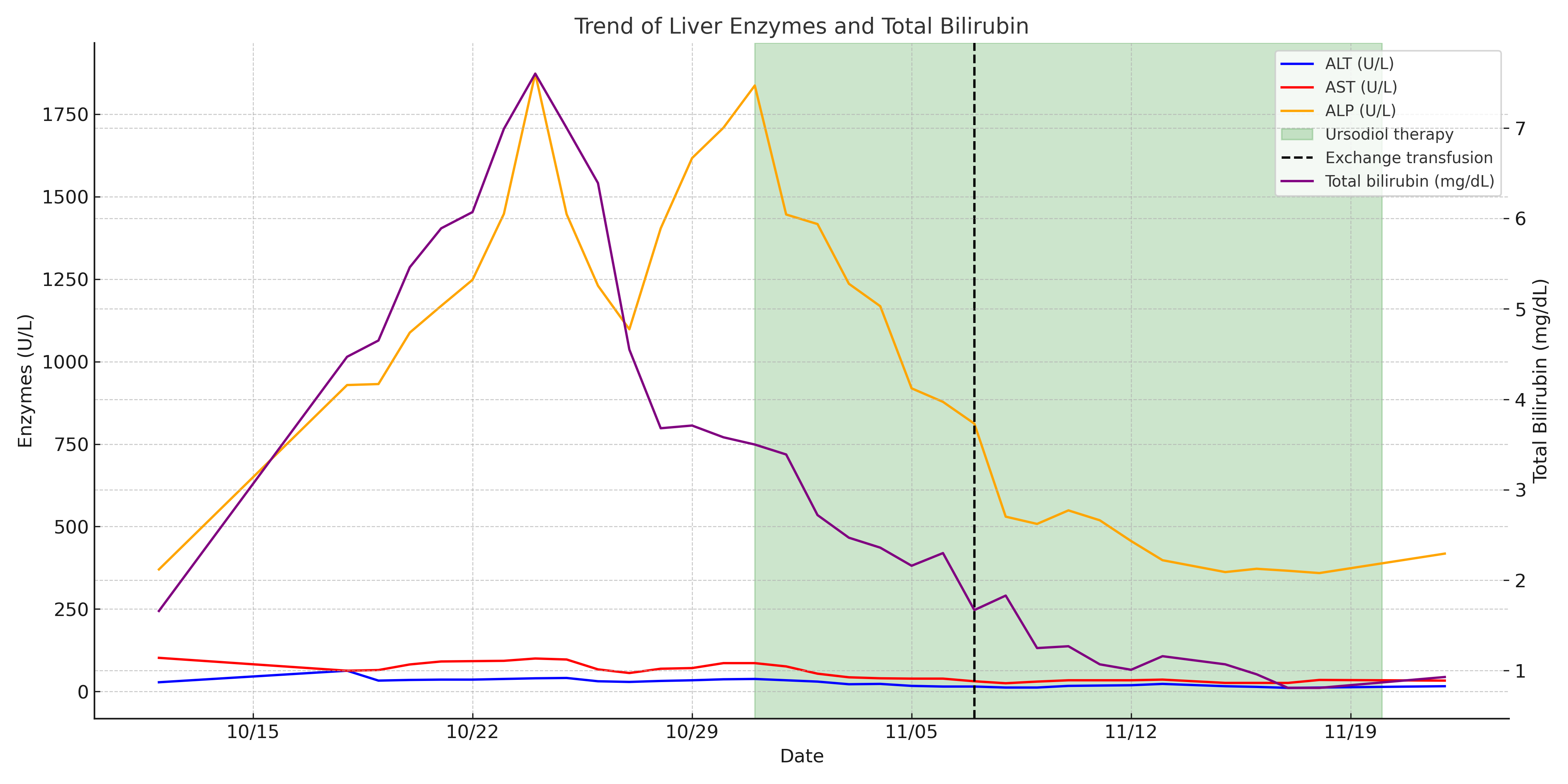
Figure: Temporal trend in serum liver enzymes, including alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and total bilirubin. A progressive decline in serum ALP was noted following the initiation of ursodiol and continued after exchange transfusion.
Disclosures:
Fawaz Hussain indicated no relevant financial relationships.
Maryam Zaffer indicated no relevant financial relationships.
Aabid Mohiuddin indicated no relevant financial relationships.
Shefali Godara indicated no relevant financial relationships.
Karan Mathur indicated no relevant financial relationships.
Fawaz Hussain, MD1, Maryam Zaffer, BA2, Aabid Mohiuddin, DO1, Shefali Godara, MD1, Karan Mathur, MD1. P4468 - Microvascular Ischemic Injury to the Biliary Tree: A Rare Case of Sickle Cell Ischemic Cholangiopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
