Tuesday Poster Session
Category: Biliary/Pancreas
P4466 - Here We Go Again, Recurrent Severe Pancreatitis in an Adult With Pancreas Divisum
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Aryak Singh, MD (he/him/his)
Saint Vincent Medical Center
Bridgeport, CT
Presenting Author(s)
Aryak Singh, MD1, Pujitha Vallivedu, MD2, Mariam Farhan, MD2
1Saint Vincent Medical Center, Bridgeport, CT; 2ST VINCENT'S MEDICAL CENTER - - BRIDGPORT, CT, Bridgeport, CT
Introduction: Pancreas Divisum (PD) occurs when the ventral and dorsal ducts of the embryonic pancreas fail to fuse during organogenesis, occurring in about 10% of the population. While 95% of patients are asymptomatic, it can lead to acute and chronic recurrent pancreatitis. The average age distribution is 40-50 years. This case of PD was the cause of severe recurrent pancreatitis.
Case Description/
Methods: 72-year-old female with history of thyroid nodules and hyperlipidemia presented with severe abdominal pain and admitted with a diagnosis of pancreatitis due to clinical and imaging findings. Her hospital course was complicated by necrotizing emphysematous pancreatitis, peripancreatic fluid collection, hypocalcemia, and bilateral pleural effusions. Despite no significant alcohol intake, family history, offending medications, viral infections, gallstones, negative workup for autoimmune pancreatitis, and hypertriglyceridemia, she was readmitted for pancreatitis twice. She subsequently underwent a Magnetic Resonance Cholangio Pancreatography which revealed a diagnosis of PD. She followed up with a pancreatic and biliary specialist and had another negative workup. After these recurrent severe episodes of pancreatitis, she underwent Endoscopic Retrograde Cholangiopancreatography (ERCP) with sphincterotomy which eventually ameliorated her symptoms.
Discussion: PD is the most common congenital pancreatic anomaly and can be overlooked as a cause of recurrent acute pancreatitis. It should be considered when common causes like alcohol use, high triglycerides, and gallstones are ruled out. In PD, the smaller ventral duct drains through the major papilla, while the larger dorsal duct drains through the minor papilla. The major obstructive cause is inadequate drainage of pancreatic secretions from minor papilla, which leads to raised intrapancreatic ductal pressure, contributing to pancreatitis. Endoscopic ultrasound is an effective first-line investigation for assessing pancreatitis, but ERCP remains the gold standard for diagnosing PD. ERCP assists in confirming by fluoroscopy and determines the type of PD, complete or incomplete. Sphincteroplasty effectively treats recurrent acute pancreatitis, but once chronic pancreatitis sets in, ductal drainage or resection is needed. It is crucial to suspect PD early when autoimmune, infectious, and social causes are ruled out.
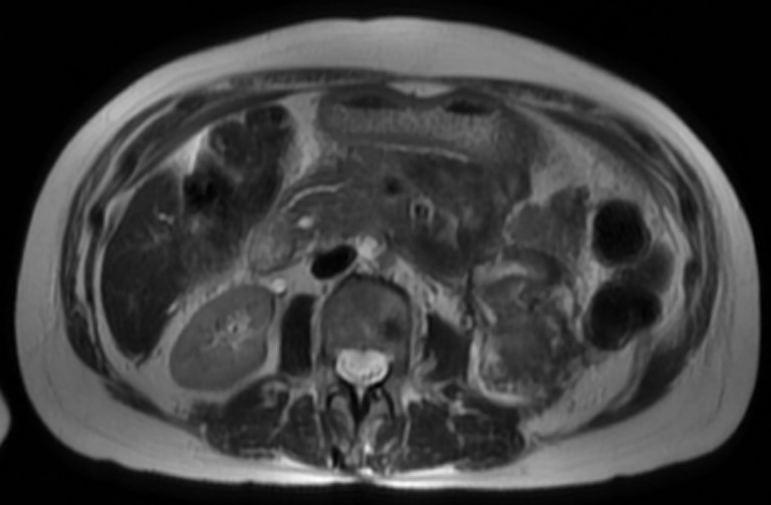
Figure: Magnetic Resonance Cholangio Pancreatography image showing Pancreas Divisum
Disclosures:
Aryak Singh indicated no relevant financial relationships.
Pujitha Vallivedu indicated no relevant financial relationships.
Mariam Farhan indicated no relevant financial relationships.
Aryak Singh, MD1, Pujitha Vallivedu, MD2, Mariam Farhan, MD2. P4466 - Here We Go Again, Recurrent Severe Pancreatitis in an Adult With Pancreas Divisum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Vincent Medical Center, Bridgeport, CT; 2ST VINCENT'S MEDICAL CENTER - - BRIDGPORT, CT, Bridgeport, CT
Introduction: Pancreas Divisum (PD) occurs when the ventral and dorsal ducts of the embryonic pancreas fail to fuse during organogenesis, occurring in about 10% of the population. While 95% of patients are asymptomatic, it can lead to acute and chronic recurrent pancreatitis. The average age distribution is 40-50 years. This case of PD was the cause of severe recurrent pancreatitis.
Case Description/
Methods: 72-year-old female with history of thyroid nodules and hyperlipidemia presented with severe abdominal pain and admitted with a diagnosis of pancreatitis due to clinical and imaging findings. Her hospital course was complicated by necrotizing emphysematous pancreatitis, peripancreatic fluid collection, hypocalcemia, and bilateral pleural effusions. Despite no significant alcohol intake, family history, offending medications, viral infections, gallstones, negative workup for autoimmune pancreatitis, and hypertriglyceridemia, she was readmitted for pancreatitis twice. She subsequently underwent a Magnetic Resonance Cholangio Pancreatography which revealed a diagnosis of PD. She followed up with a pancreatic and biliary specialist and had another negative workup. After these recurrent severe episodes of pancreatitis, she underwent Endoscopic Retrograde Cholangiopancreatography (ERCP) with sphincterotomy which eventually ameliorated her symptoms.
Discussion: PD is the most common congenital pancreatic anomaly and can be overlooked as a cause of recurrent acute pancreatitis. It should be considered when common causes like alcohol use, high triglycerides, and gallstones are ruled out. In PD, the smaller ventral duct drains through the major papilla, while the larger dorsal duct drains through the minor papilla. The major obstructive cause is inadequate drainage of pancreatic secretions from minor papilla, which leads to raised intrapancreatic ductal pressure, contributing to pancreatitis. Endoscopic ultrasound is an effective first-line investigation for assessing pancreatitis, but ERCP remains the gold standard for diagnosing PD. ERCP assists in confirming by fluoroscopy and determines the type of PD, complete or incomplete. Sphincteroplasty effectively treats recurrent acute pancreatitis, but once chronic pancreatitis sets in, ductal drainage or resection is needed. It is crucial to suspect PD early when autoimmune, infectious, and social causes are ruled out.
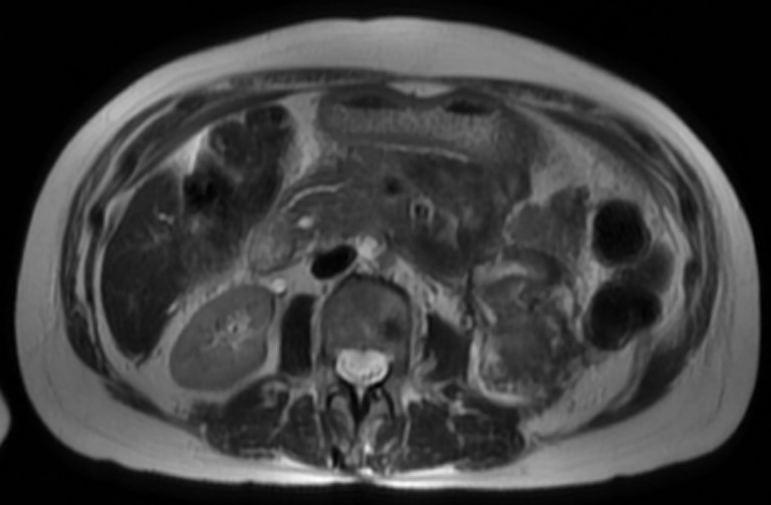
Figure: Magnetic Resonance Cholangio Pancreatography image showing Pancreas Divisum
Disclosures:
Aryak Singh indicated no relevant financial relationships.
Pujitha Vallivedu indicated no relevant financial relationships.
Mariam Farhan indicated no relevant financial relationships.
Aryak Singh, MD1, Pujitha Vallivedu, MD2, Mariam Farhan, MD2. P4466 - Here We Go Again, Recurrent Severe Pancreatitis in an Adult With Pancreas Divisum, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
