Tuesday Poster Session
Category: Biliary/Pancreas
P4465 - Recurrent Hemobilia in a Patient With Familial Hypertriglyceridemia-Induced Pancreatitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Minting Yu, MD (she/her/hers)
University of Illinois
Chicago, IL
Presenting Author(s)
Abhimanyu Karumanchi, MBBS1, Minting Yu, MD2, Herman Suga, MD2, Ashley Vareedayah, MD3, Brian Boulay, MD2
1Kamineni Institute of Medical Sciences, Narketpalli, Broomfield, CO; 2University of Illinois, Chicago, IL; 3University of Illinois Hospital, Chicago, IL
Introduction: A 35-year-old male with familial hypertriglyceridemia-induced necrotizing pancreatitis, complicated by recurrent biliary stricture, portal vein thrombosis (PVT) with cavernous transformation, varices and hemobilia. This case illustrates that when endoscopic options are exhausted for the management of hemobilia, a multidisciplinary approach with innovative strategies can be used to achieve portal decompression and hemostasis.
Case Description/
Methods: The patient initially presented in 2014 with recurrent acute pancreatitis, complicated by biliary stricture and jaundice. Over the years, he underwent multiple ERCP for biliary stent placement and exchange, for refractory biliary stricture.
In April 2022, he presented with hematemesis. He was thrombocytopenic and CT demonstrated splenomegaly. Endoscopy revealed gastric and esophageal varices, complications from PVT in the setting of chronic pancreatitis. Splenic artery embolization was performed, followed by splenectomy and cholecystectomy in May 2022.
In June 2024, he was hospitalized with melena and elevated liver enzymes. ERCP revealed hemobilia with balloon sweep. Cholangiogram revealed a pulsating intraductal varix and fistula in the biliary epithelium corresponding to the site of choledocal varices. Hemostasis was achieved with a fully covered metal stent. Recurrent bleeding was noted during repeat ERCP for stent removal, necessitating additional stent placement. Octreotide was initiated, due to intolerance of beta-blocker.
Cross sectional imaging in August 2024 showed cavernous transformation of the portal vein and gallbladder fossa varices. Standard TIPS was deferred due to complex anatomy. After multidisciplinary discussion, he underwent percutaneous transmesentric portal vein reconstruction and TIPS placement – an unconventional route. Mesenteric venogram at the time was notable for contrast opacification of the common bile duct draining into the small bowel, confirming active hemobilia. Post-procedure, collaterals were decompressed and residual varices embolized.
Discussion: Hemobilia, is rare and often caused by trauma, inflammation, malignancy, or varices. In this case, hemobilia was due to choledochal varices from chronic PVT. Portal vein reconstruction and TIPS via SMV access restored portal flow, confirmed active hemobilia, and achieved hemostasis. This case underscores the evolving role of advanced endovascular techniques and collaborative care in managing portal hypertension-related GI bleeding.

Figure: ERCP spyglass show intraductal varix
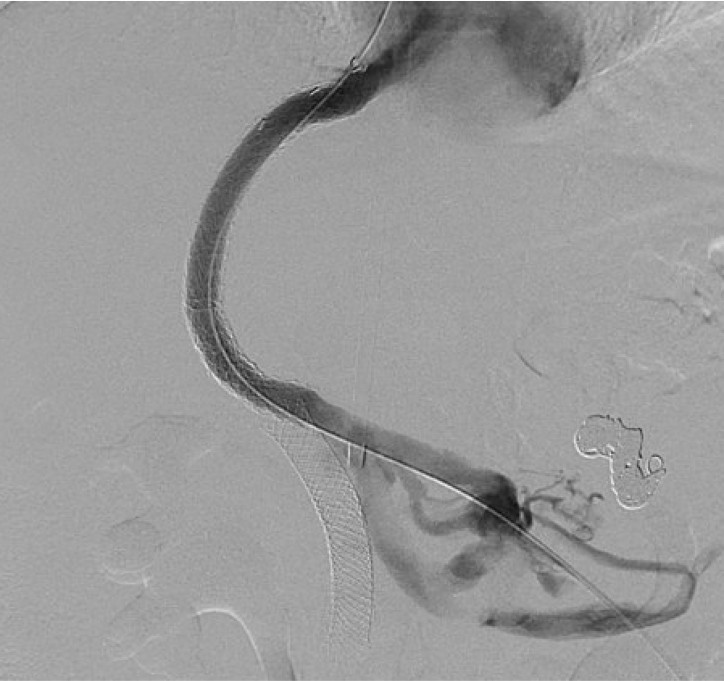
Figure: IR TIPS procedure showing active bleeding into the bile duct
Disclosures:
Abhimanyu Karumanchi indicated no relevant financial relationships.
Minting Yu indicated no relevant financial relationships.
Herman Suga indicated no relevant financial relationships.
Ashley Vareedayah indicated no relevant financial relationships.
Brian Boulay: ConMed – Consultant. Cook Medical – Consultant.
Abhimanyu Karumanchi, MBBS1, Minting Yu, MD2, Herman Suga, MD2, Ashley Vareedayah, MD3, Brian Boulay, MD2. P4465 - Recurrent Hemobilia in a Patient With Familial Hypertriglyceridemia-Induced Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kamineni Institute of Medical Sciences, Narketpalli, Broomfield, CO; 2University of Illinois, Chicago, IL; 3University of Illinois Hospital, Chicago, IL
Introduction: A 35-year-old male with familial hypertriglyceridemia-induced necrotizing pancreatitis, complicated by recurrent biliary stricture, portal vein thrombosis (PVT) with cavernous transformation, varices and hemobilia. This case illustrates that when endoscopic options are exhausted for the management of hemobilia, a multidisciplinary approach with innovative strategies can be used to achieve portal decompression and hemostasis.
Case Description/
Methods: The patient initially presented in 2014 with recurrent acute pancreatitis, complicated by biliary stricture and jaundice. Over the years, he underwent multiple ERCP for biliary stent placement and exchange, for refractory biliary stricture.
In April 2022, he presented with hematemesis. He was thrombocytopenic and CT demonstrated splenomegaly. Endoscopy revealed gastric and esophageal varices, complications from PVT in the setting of chronic pancreatitis. Splenic artery embolization was performed, followed by splenectomy and cholecystectomy in May 2022.
In June 2024, he was hospitalized with melena and elevated liver enzymes. ERCP revealed hemobilia with balloon sweep. Cholangiogram revealed a pulsating intraductal varix and fistula in the biliary epithelium corresponding to the site of choledocal varices. Hemostasis was achieved with a fully covered metal stent. Recurrent bleeding was noted during repeat ERCP for stent removal, necessitating additional stent placement. Octreotide was initiated, due to intolerance of beta-blocker.
Cross sectional imaging in August 2024 showed cavernous transformation of the portal vein and gallbladder fossa varices. Standard TIPS was deferred due to complex anatomy. After multidisciplinary discussion, he underwent percutaneous transmesentric portal vein reconstruction and TIPS placement – an unconventional route. Mesenteric venogram at the time was notable for contrast opacification of the common bile duct draining into the small bowel, confirming active hemobilia. Post-procedure, collaterals were decompressed and residual varices embolized.
Discussion: Hemobilia, is rare and often caused by trauma, inflammation, malignancy, or varices. In this case, hemobilia was due to choledochal varices from chronic PVT. Portal vein reconstruction and TIPS via SMV access restored portal flow, confirmed active hemobilia, and achieved hemostasis. This case underscores the evolving role of advanced endovascular techniques and collaborative care in managing portal hypertension-related GI bleeding.

Figure: ERCP spyglass show intraductal varix
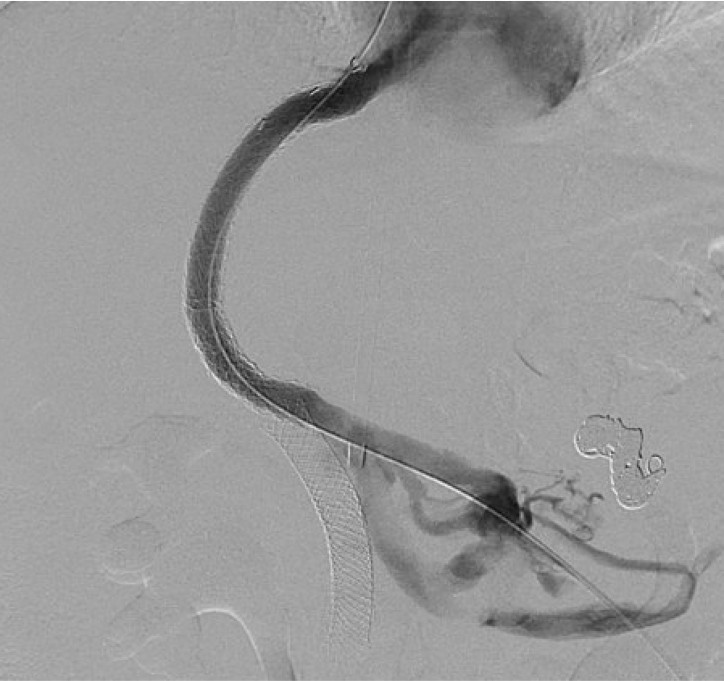
Figure: IR TIPS procedure showing active bleeding into the bile duct
Disclosures:
Abhimanyu Karumanchi indicated no relevant financial relationships.
Minting Yu indicated no relevant financial relationships.
Herman Suga indicated no relevant financial relationships.
Ashley Vareedayah indicated no relevant financial relationships.
Brian Boulay: ConMed – Consultant. Cook Medical – Consultant.
Abhimanyu Karumanchi, MBBS1, Minting Yu, MD2, Herman Suga, MD2, Ashley Vareedayah, MD3, Brian Boulay, MD2. P4465 - Recurrent Hemobilia in a Patient With Familial Hypertriglyceridemia-Induced Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
