Tuesday Poster Session
Category: Biliary/Pancreas
P4451 - Exploring the Impact: Periampullary Duodenal Diverticulum and Pancreatitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nishani Wickramarachchi, DO
HCA Healthcare Riverside Community Hospital
Riverside, CA
Presenting Author(s)
Nishani Wickramarachchi, DO1, Regis Lee, DO1, Crystal Dorgalli, DO, MS2, Alex Prevallet, DO1, Marco Paez, MD1
1HCA Healthcare Riverside Community Hospital, Riverside, CA; 2HCA Riverside Community Hospital, Riverside, CA
Introduction: Lemmel syndrome is a condition that involves a periampullary duodenal diverticulum that can cause compression of the pancreatic or common bile duct (CBD) leading to abdominal pain and obstructive jaundice. Due to its rarity, its complete pathophysiology is unclear. In this case, a patient presenting with abdominal pain, abnormal liver associated enzymes, and elevated lipase was found to have pancreatitis secondary to Lemmel syndrome.
Case Description/
Methods: A 51-year-old female presented to the hospital with 1 day of acute constant, non-radiating right upper quadrant (RUQ) and epigastric abdominal pain. She denied nausea, vomiting, jaundice, weight loss or alcohol use. She denied sick contacts, or travel history. On exam she had RUQ and epigastric tenderness. Labs showed elevated AST 770 U/L, ALT 933 U/L, lipase 605, total bilirubin 2.5 mg/dL, and ALP 123. Hepatitis A, B and C panel was negative. Abdominal CT showed a 2.9 cm prominent duodenal diverticulum with dilated 8 mm CBD without obstructive lesion or choledocholithiasis. Abdominal ultrasound showed dilated CBD of 6.6 mm and MRCP was negative for choledocholithiasis without pancreatic mass, dilation of the pancreatic duct and no cholecystitis. MRCP did show a 1.8x1.5 cm and a 1.7x1.0 cm duodenal diverticula in the ampullary region possibly causing extrinsic compression/mass effect on the distal CBD. Given findings and persistent pain, she was evaluated with endoscopic ultrasound (EUS) and side-viewing duodenoscope. EUS showed no choledocholithiasis, cholelithiasis, choledochocele and no evidence of pancreatic lesions. EUS showed a 5 mm CBD and an anechoic extraluminal sac-like structure with some acoustic artifacts consistent with a large periampullary diverticulum. Side-viewing duodenoscope evaluation showed a large type II center margin periampullary diverticula (Figure 1&2). Her pain resolved, liver enzymes continued to downtrend and she was discharged home without further interventions.
Discussion: The pathophysiology of Lemmel syndrome remains not fully understood, this case highlights the importance of considering Lemmel syndrome when a large periampullary diverticulum is seen with unexplained biliary symptoms and image findings suggestive of CBD dilation without other identifiable causes. Management is usually conservative, with surgical intervention considered only for significant or persistent symptoms. Recognition of this syndrome can help avoid unnecessary interventions and guide treatment strategies.
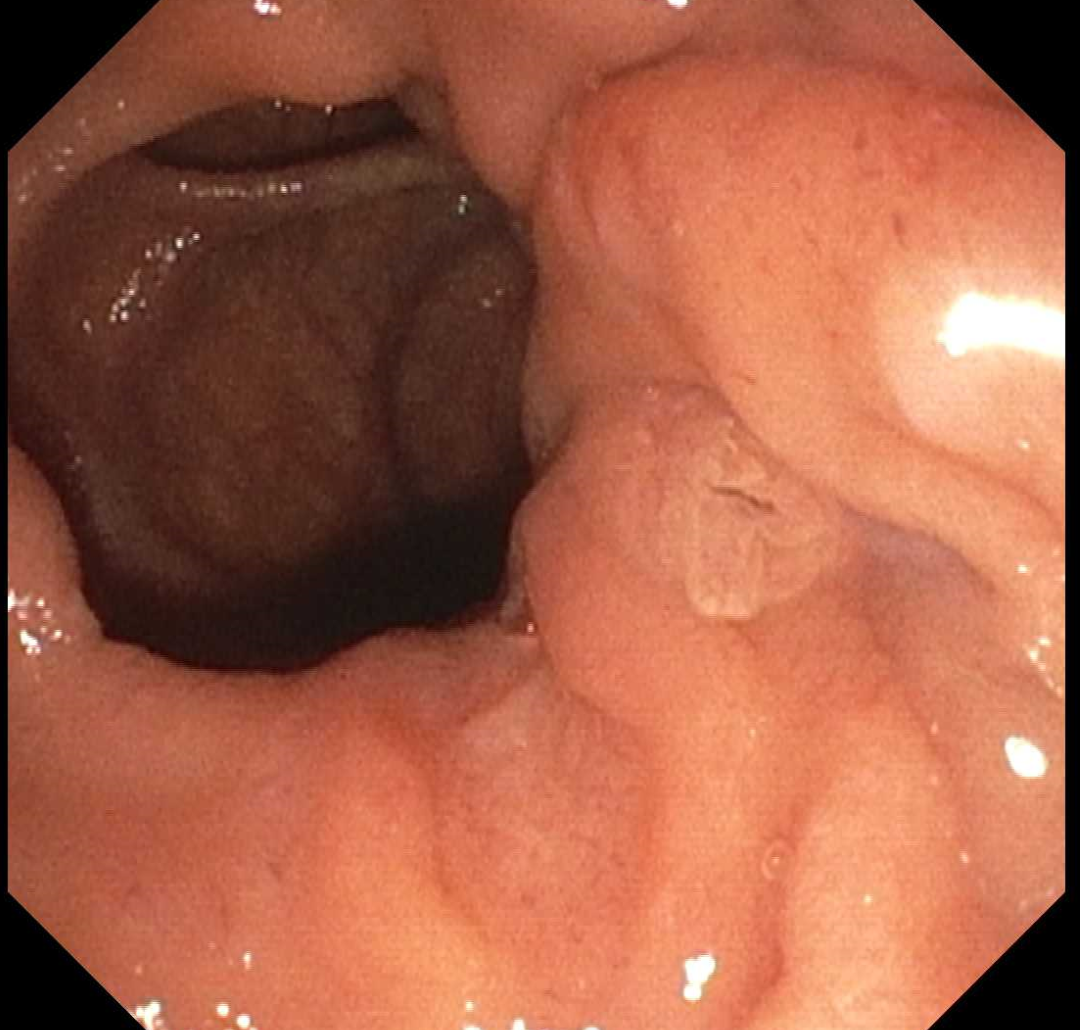
Figure: Figure 1: Type II Center margin periampullary diverticula
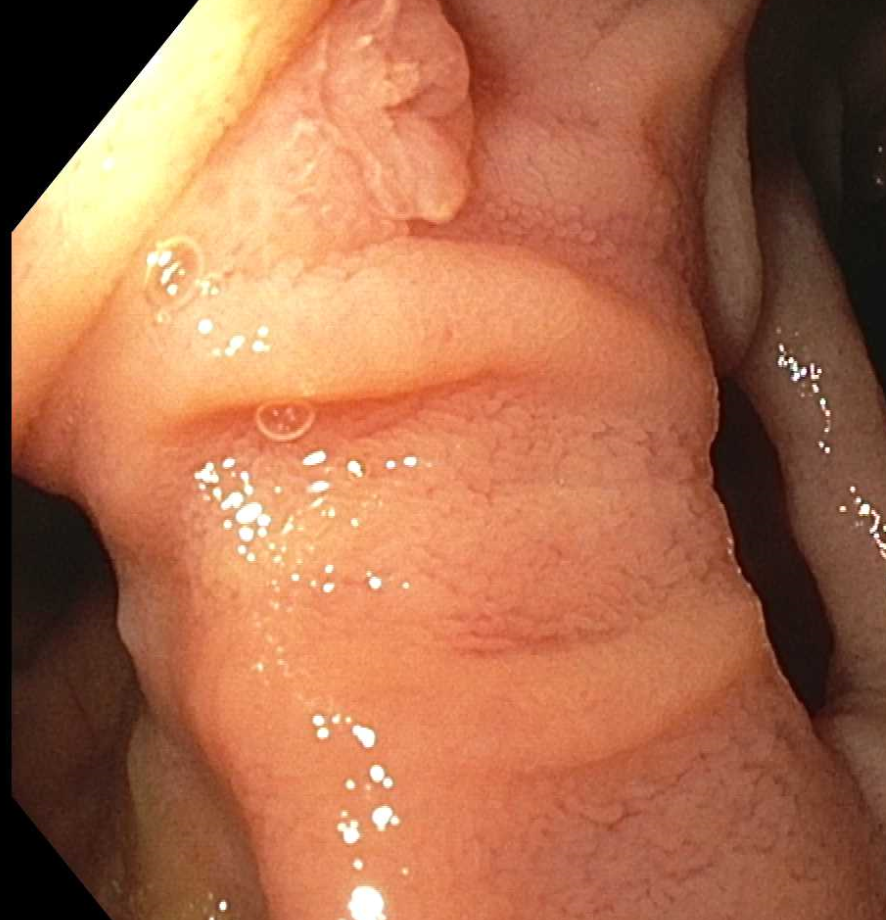
Figure: Figure 2: Two diverticulum visualized with the ampulla in the center
Disclosures:
Nishani Wickramarachchi indicated no relevant financial relationships.
Regis Lee indicated no relevant financial relationships.
Crystal Dorgalli indicated no relevant financial relationships.
Alex Prevallet indicated no relevant financial relationships.
Marco Paez indicated no relevant financial relationships.
Nishani Wickramarachchi, DO1, Regis Lee, DO1, Crystal Dorgalli, DO, MS2, Alex Prevallet, DO1, Marco Paez, MD1. P4451 - Exploring the Impact: Periampullary Duodenal Diverticulum and Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Healthcare Riverside Community Hospital, Riverside, CA; 2HCA Riverside Community Hospital, Riverside, CA
Introduction: Lemmel syndrome is a condition that involves a periampullary duodenal diverticulum that can cause compression of the pancreatic or common bile duct (CBD) leading to abdominal pain and obstructive jaundice. Due to its rarity, its complete pathophysiology is unclear. In this case, a patient presenting with abdominal pain, abnormal liver associated enzymes, and elevated lipase was found to have pancreatitis secondary to Lemmel syndrome.
Case Description/
Methods: A 51-year-old female presented to the hospital with 1 day of acute constant, non-radiating right upper quadrant (RUQ) and epigastric abdominal pain. She denied nausea, vomiting, jaundice, weight loss or alcohol use. She denied sick contacts, or travel history. On exam she had RUQ and epigastric tenderness. Labs showed elevated AST 770 U/L, ALT 933 U/L, lipase 605, total bilirubin 2.5 mg/dL, and ALP 123. Hepatitis A, B and C panel was negative. Abdominal CT showed a 2.9 cm prominent duodenal diverticulum with dilated 8 mm CBD without obstructive lesion or choledocholithiasis. Abdominal ultrasound showed dilated CBD of 6.6 mm and MRCP was negative for choledocholithiasis without pancreatic mass, dilation of the pancreatic duct and no cholecystitis. MRCP did show a 1.8x1.5 cm and a 1.7x1.0 cm duodenal diverticula in the ampullary region possibly causing extrinsic compression/mass effect on the distal CBD. Given findings and persistent pain, she was evaluated with endoscopic ultrasound (EUS) and side-viewing duodenoscope. EUS showed no choledocholithiasis, cholelithiasis, choledochocele and no evidence of pancreatic lesions. EUS showed a 5 mm CBD and an anechoic extraluminal sac-like structure with some acoustic artifacts consistent with a large periampullary diverticulum. Side-viewing duodenoscope evaluation showed a large type II center margin periampullary diverticula (Figure 1&2). Her pain resolved, liver enzymes continued to downtrend and she was discharged home without further interventions.
Discussion: The pathophysiology of Lemmel syndrome remains not fully understood, this case highlights the importance of considering Lemmel syndrome when a large periampullary diverticulum is seen with unexplained biliary symptoms and image findings suggestive of CBD dilation without other identifiable causes. Management is usually conservative, with surgical intervention considered only for significant or persistent symptoms. Recognition of this syndrome can help avoid unnecessary interventions and guide treatment strategies.
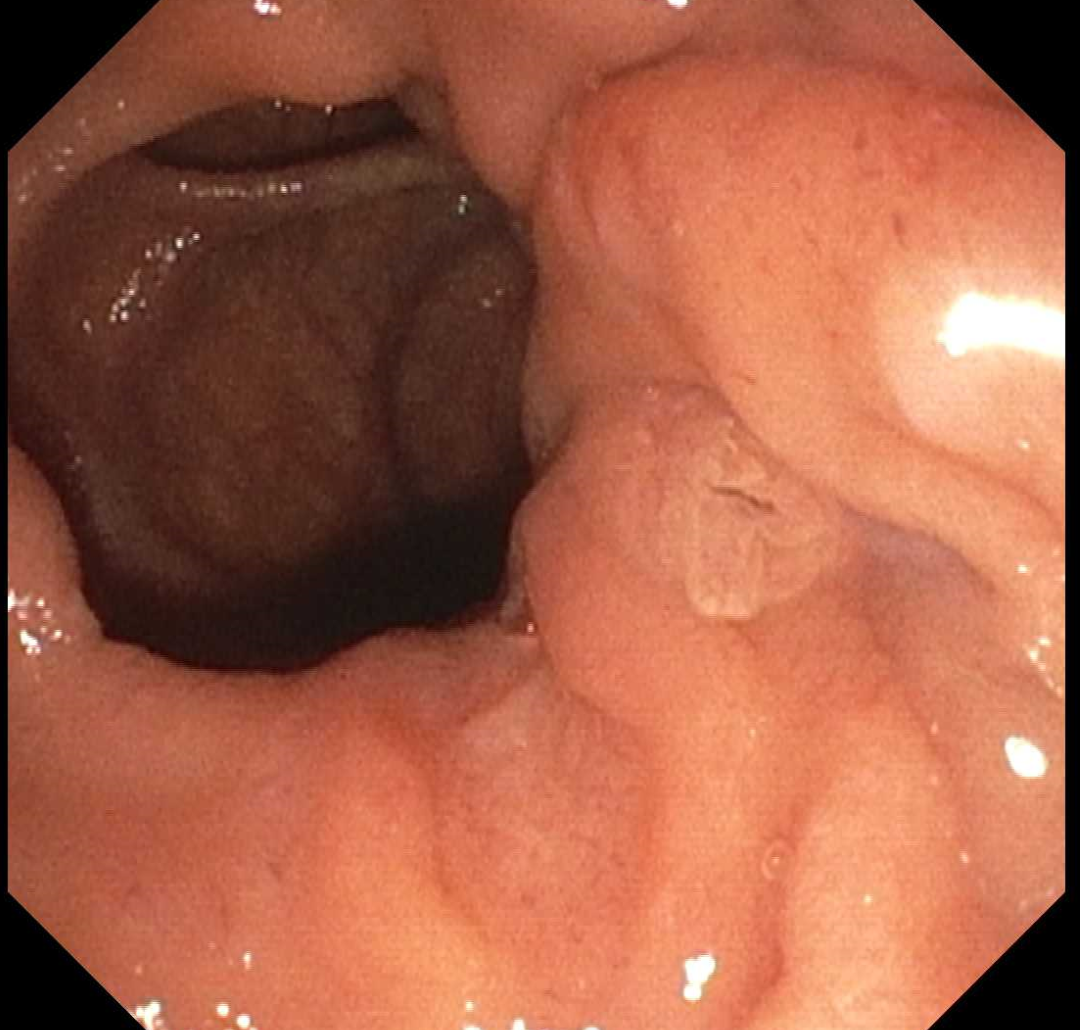
Figure: Figure 1: Type II Center margin periampullary diverticula
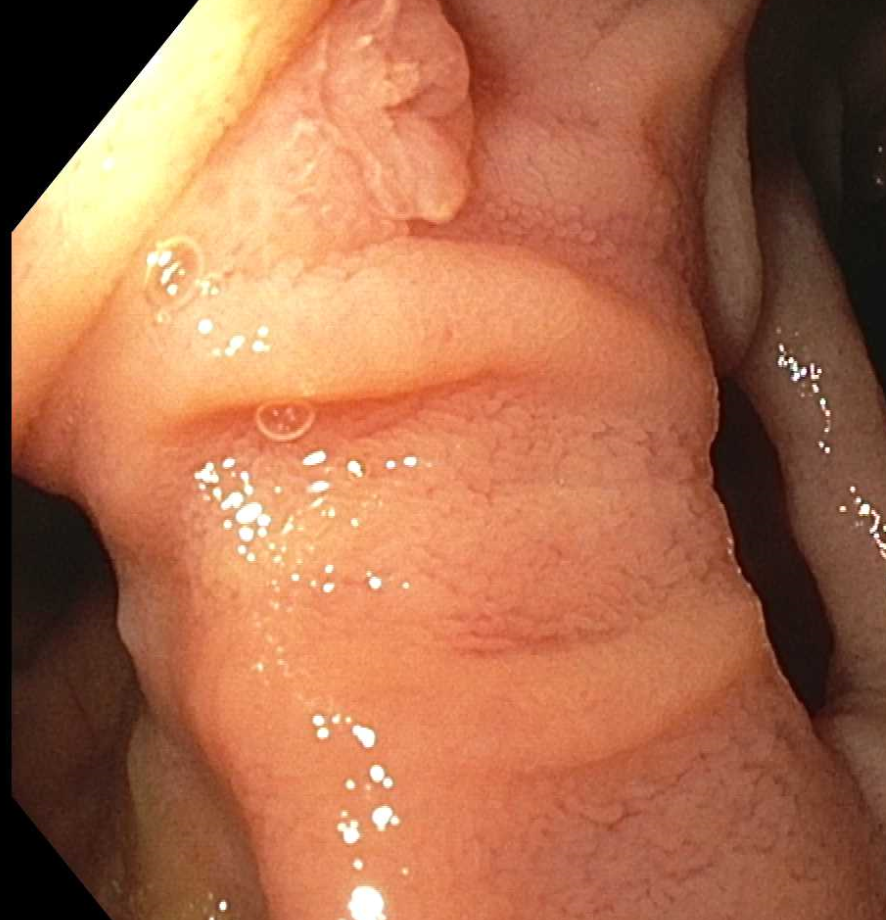
Figure: Figure 2: Two diverticulum visualized with the ampulla in the center
Disclosures:
Nishani Wickramarachchi indicated no relevant financial relationships.
Regis Lee indicated no relevant financial relationships.
Crystal Dorgalli indicated no relevant financial relationships.
Alex Prevallet indicated no relevant financial relationships.
Marco Paez indicated no relevant financial relationships.
Nishani Wickramarachchi, DO1, Regis Lee, DO1, Crystal Dorgalli, DO, MS2, Alex Prevallet, DO1, Marco Paez, MD1. P4451 - Exploring the Impact: Periampullary Duodenal Diverticulum and Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
