Tuesday Poster Session
Category: Biliary/Pancreas
P4450 - Pancreatic Head Mass With Jaundice: Not Always Pancreatic Adenocarcinoma - A Rare Case of Lymphoma Mimicking Pancreatic Adenocarcinoma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hannah Yoo, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Hannah Yoo, MD1, Lixamar Colon Vicenti, MD, MSNS2
1University of Texas Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX
Introduction: Pancreatic head mass with biliary obstruction is most commonly associated with Pancreatic Adenocarcinoma (PAC). Pancreatic Primary Lymphomas (PPL) is a rare tumor that can also mimic this presentation. Accurate diagnosis through endoscopic intervention and histology is crucial in determining the appropriate therapy.
Case Description/
Methods: A 48-year-old male with no medical history presented with 3-month abdominal/back pain, scleral icterus, and pruritus without constitutional symptoms. Labs revealed cholestatic liver injury (ALP 455, AST 116, ALT 286) and elevated lipase (1,337). Right upper quadrant US showed a dilated common bile duct (1.9 cm) without intrahepatic biliary dilation. CT abdomen/pelvis revealed a 7.4cm x 4.7 cm pancreatic head/uncinate process mass and a 2cm x 2.3cm mesenteric mass (Figure 1). Patient underwent EUS with FNA of the pancreatic mass and ERCP with biliary brushings, biliary sphincterotomy and stent placement due to biliary stricture. CA-199 and CEA were negative. CT abdomen 3 phase confirmed the pancreatic and mesenteric mass without vascular involvement. CT chest revealed no distant metastasis. Patient underwent CT-guided biopsy of the mesenteric mass and internal jugular tunneled port placement for presumed PAC. The FNA was positive for B-cell lymphoma of follicle center cell origin, most likely follicular lymphoma or diffuse large B-cell lymphoma (DLBCL). PET scan showed a bulky lymph node with SUV > 13 (16.3), concerning for aggressive lymphoma. R-CHOP was initiated to treat as aggressive B cell lymphoma.
Discussion: PPL is a rare pancreatic tumor, representing 0.2% of all pancreatic tumors and the most common histological type is DLBCL (80%).1 PPL and PAC can be be indistinguishable due to vague presentations of abdominal pain, jaundice, and constitutional symptoms and similar radiographic findings.1 Some studies suggest abdominal pain without jaundice or constitutional symptoms favors the diagnosis of PPLs.2 However, histological classification is require for a definitive diagnosis.3 Hence, endoscopic modalities like EUS-FNA are essential for diagnosis; and ERCP further allows for therapeutic intervention in cases of biliary obstruction or strictures. Distinguishing PPL from PAC is crucial because of the significant difference in management. PPL is treated with R-CHOP with possible radiation while PAC entails FOLFIRINOX and surgical resection, which alone carries serious risks including hemorrhage, pancreatitis, abscess formation, and anastomotic leak.1-2,4
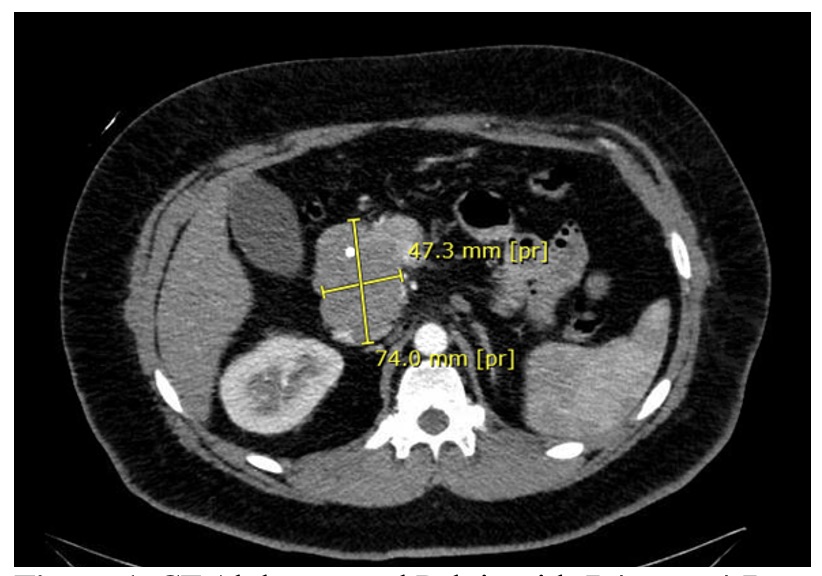
Figure: Figure 1. CT Abdomen and Pelvis with 7.4 cm x 4.7 cm mass on the pancreatic head and uncinate process.
Disclosures:
Hannah Yoo indicated no relevant financial relationships.
Lixamar Colon Vicenti indicated no relevant financial relationships.
Hannah Yoo, MD1, Lixamar Colon Vicenti, MD, MSNS2. P4450 - Pancreatic Head Mass With Jaundice: Not Always Pancreatic Adenocarcinoma - A Rare Case of Lymphoma Mimicking Pancreatic Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX
Introduction: Pancreatic head mass with biliary obstruction is most commonly associated with Pancreatic Adenocarcinoma (PAC). Pancreatic Primary Lymphomas (PPL) is a rare tumor that can also mimic this presentation. Accurate diagnosis through endoscopic intervention and histology is crucial in determining the appropriate therapy.
Case Description/
Methods: A 48-year-old male with no medical history presented with 3-month abdominal/back pain, scleral icterus, and pruritus without constitutional symptoms. Labs revealed cholestatic liver injury (ALP 455, AST 116, ALT 286) and elevated lipase (1,337). Right upper quadrant US showed a dilated common bile duct (1.9 cm) without intrahepatic biliary dilation. CT abdomen/pelvis revealed a 7.4cm x 4.7 cm pancreatic head/uncinate process mass and a 2cm x 2.3cm mesenteric mass (Figure 1). Patient underwent EUS with FNA of the pancreatic mass and ERCP with biliary brushings, biliary sphincterotomy and stent placement due to biliary stricture. CA-199 and CEA were negative. CT abdomen 3 phase confirmed the pancreatic and mesenteric mass without vascular involvement. CT chest revealed no distant metastasis. Patient underwent CT-guided biopsy of the mesenteric mass and internal jugular tunneled port placement for presumed PAC. The FNA was positive for B-cell lymphoma of follicle center cell origin, most likely follicular lymphoma or diffuse large B-cell lymphoma (DLBCL). PET scan showed a bulky lymph node with SUV > 13 (16.3), concerning for aggressive lymphoma. R-CHOP was initiated to treat as aggressive B cell lymphoma.
Discussion: PPL is a rare pancreatic tumor, representing 0.2% of all pancreatic tumors and the most common histological type is DLBCL (80%).1 PPL and PAC can be be indistinguishable due to vague presentations of abdominal pain, jaundice, and constitutional symptoms and similar radiographic findings.1 Some studies suggest abdominal pain without jaundice or constitutional symptoms favors the diagnosis of PPLs.2 However, histological classification is require for a definitive diagnosis.3 Hence, endoscopic modalities like EUS-FNA are essential for diagnosis; and ERCP further allows for therapeutic intervention in cases of biliary obstruction or strictures. Distinguishing PPL from PAC is crucial because of the significant difference in management. PPL is treated with R-CHOP with possible radiation while PAC entails FOLFIRINOX and surgical resection, which alone carries serious risks including hemorrhage, pancreatitis, abscess formation, and anastomotic leak.1-2,4
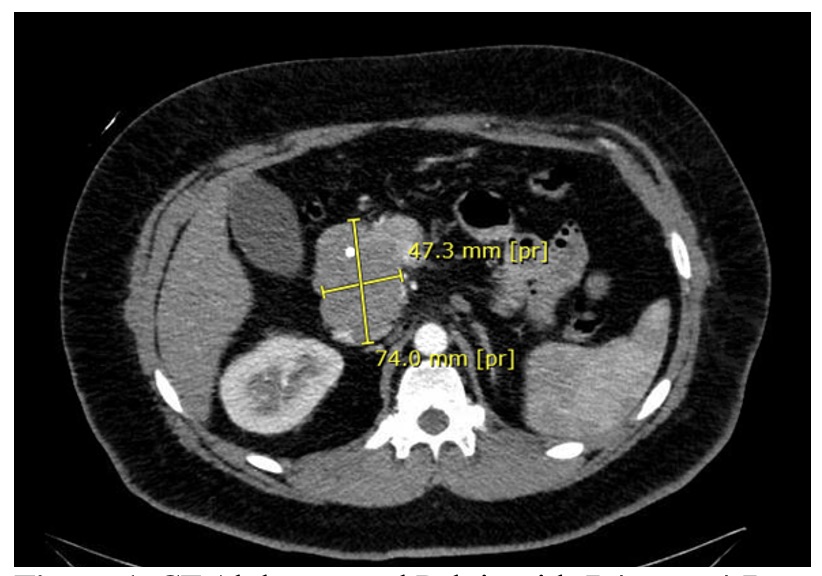
Figure: Figure 1. CT Abdomen and Pelvis with 7.4 cm x 4.7 cm mass on the pancreatic head and uncinate process.
Disclosures:
Hannah Yoo indicated no relevant financial relationships.
Lixamar Colon Vicenti indicated no relevant financial relationships.
Hannah Yoo, MD1, Lixamar Colon Vicenti, MD, MSNS2. P4450 - Pancreatic Head Mass With Jaundice: Not Always Pancreatic Adenocarcinoma - A Rare Case of Lymphoma Mimicking Pancreatic Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
