Tuesday Poster Session
Category: Biliary/Pancreas
P4409 - A Rare Case of Portal Biliopathy in the Setting of Cavernomatous Transformation From Chronic Portal Vein Thrombosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sneh Sonaiya, MD, MPH, MBA
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Sneh Sonaiya, MD, MPH, MBA1, Zan Ferrin, DO2, Jiayi Ge, MD1, Amol Koldhekar, MD1, Vignan Manne, MD1
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV
Introduction: Extrahepatic portal vein obstruction (EHPVO) is a rare vascular condition marked by chronic portal vein thrombosis and cavernomatous transformation, often resulting in extensive collateral formation. Peribiliary collaterals can compress the bile ducts, leading to portal biliopathy, which may present with cholestasis, jaundice, or cholangitis. Chronic portal vein thrombosis is the most common etiology of EHPVO. We present a complex case of portal biliopathy managed with transjugular intrahepatic portosystemic shunt (TIPS) and portal vein thrombectomy.
Case Description/
Methods: A 60-year-old female with a history of choledocholithiasis presented with severe right upper quadrant abdominal pain. She had recently undergone multiple ERCPs, which included placement and removal of fully covered metal stents, biliary sludge extraction, and balloon sweeps for persistent common bile duct dilation. On presentation, CT revealed marked intrahepatic biliary dilatation and progression of cavernous transformation of the portal vein, suggestive of obstructive portal biliopathy likely secondary to EHPVO. The patient underwent a technically challenging but ultimately successful TIPS along with transplenic and transhepatic recanalization of portal vein thrombosis as well as portal vein mechanical thrombectomy. Her hospital course was complicated by Acute Hypoxic Respiratory Failure requiring mechanical ventilation, PEA arrest followed by Return of Spontaneous Circulation, ventilator-associated pneumonia, melena requiring blood transfusions with EGD notable for gastropathy, and heparin-induced thrombocytopenia necessitating a transition from a heparin to fondaparinux. Due to prolonged ventilator dependence, the patient ultimately required tracheostomy and PEG tube placement.
Discussion: Management of symptomatic portal biliopathy often requires both endoscopic biliary decompression and portal pressure reduction, and TIPS can be an effective strategy in such cases by decompressing the portal system and reducing collateral pressure. However, TIPS in EHPVO is technically challenging due to chronic thrombosis and cavernomatous transformation of the portal vein. In our patient, an initial TIPS attempt failed, but a repeat TIPS with portal vein thrombectomy was successful. This case highlights the diagnostic and therapeutic complexities of portal biliopathy in the setting of chronic EHPVO, and supports a multidisciplinary approach, including interventional radiology and gastroenterology, when managing such patients.
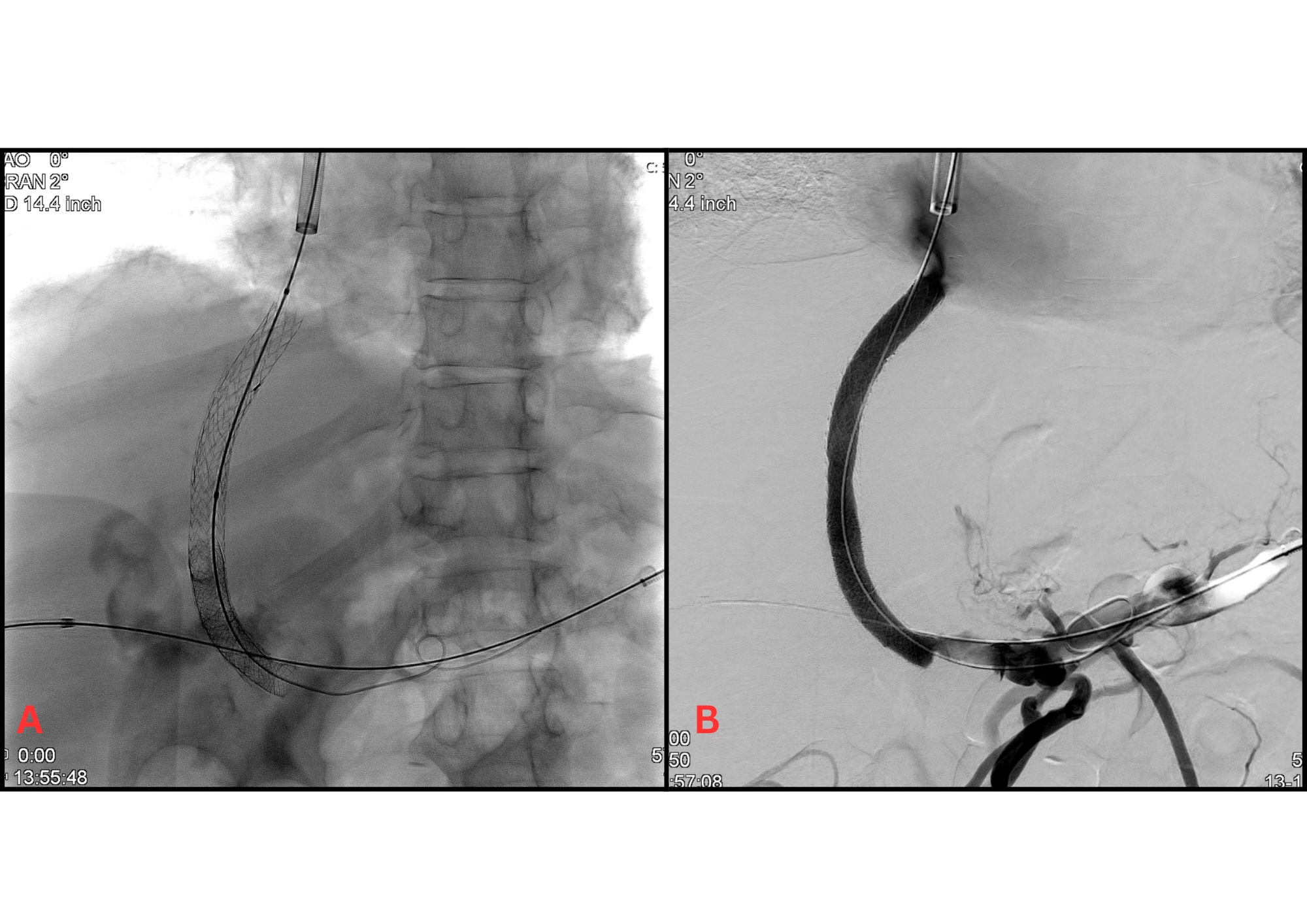
Figure: Figure 1.
(A) Fluoroscopic image demonstrating deployment of stent during transjugular intrahepatic portosystemic shunt (TIPS) placement.
(B) Contrast-enhanced imaging showing successful shunt creation with opacification of the portal venous system, including recanalization of the thrombosed portal vein and decompression of cavernous collaterals. The irregular contrast flow and network of collateral vessels in the portal vein region suggest cavernomatous transformation typical of chronic portal vein thrombosis
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Zan Ferrin indicated no relevant financial relationships.
Jiayi Ge indicated no relevant financial relationships.
Amol Koldhekar indicated no relevant financial relationships.
Vignan Manne indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA1, Zan Ferrin, DO2, Jiayi Ge, MD1, Amol Koldhekar, MD1, Vignan Manne, MD1. P4409 - A Rare Case of Portal Biliopathy in the Setting of Cavernomatous Transformation From Chronic Portal Vein Thrombosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV
Introduction: Extrahepatic portal vein obstruction (EHPVO) is a rare vascular condition marked by chronic portal vein thrombosis and cavernomatous transformation, often resulting in extensive collateral formation. Peribiliary collaterals can compress the bile ducts, leading to portal biliopathy, which may present with cholestasis, jaundice, or cholangitis. Chronic portal vein thrombosis is the most common etiology of EHPVO. We present a complex case of portal biliopathy managed with transjugular intrahepatic portosystemic shunt (TIPS) and portal vein thrombectomy.
Case Description/
Methods: A 60-year-old female with a history of choledocholithiasis presented with severe right upper quadrant abdominal pain. She had recently undergone multiple ERCPs, which included placement and removal of fully covered metal stents, biliary sludge extraction, and balloon sweeps for persistent common bile duct dilation. On presentation, CT revealed marked intrahepatic biliary dilatation and progression of cavernous transformation of the portal vein, suggestive of obstructive portal biliopathy likely secondary to EHPVO. The patient underwent a technically challenging but ultimately successful TIPS along with transplenic and transhepatic recanalization of portal vein thrombosis as well as portal vein mechanical thrombectomy. Her hospital course was complicated by Acute Hypoxic Respiratory Failure requiring mechanical ventilation, PEA arrest followed by Return of Spontaneous Circulation, ventilator-associated pneumonia, melena requiring blood transfusions with EGD notable for gastropathy, and heparin-induced thrombocytopenia necessitating a transition from a heparin to fondaparinux. Due to prolonged ventilator dependence, the patient ultimately required tracheostomy and PEG tube placement.
Discussion: Management of symptomatic portal biliopathy often requires both endoscopic biliary decompression and portal pressure reduction, and TIPS can be an effective strategy in such cases by decompressing the portal system and reducing collateral pressure. However, TIPS in EHPVO is technically challenging due to chronic thrombosis and cavernomatous transformation of the portal vein. In our patient, an initial TIPS attempt failed, but a repeat TIPS with portal vein thrombectomy was successful. This case highlights the diagnostic and therapeutic complexities of portal biliopathy in the setting of chronic EHPVO, and supports a multidisciplinary approach, including interventional radiology and gastroenterology, when managing such patients.
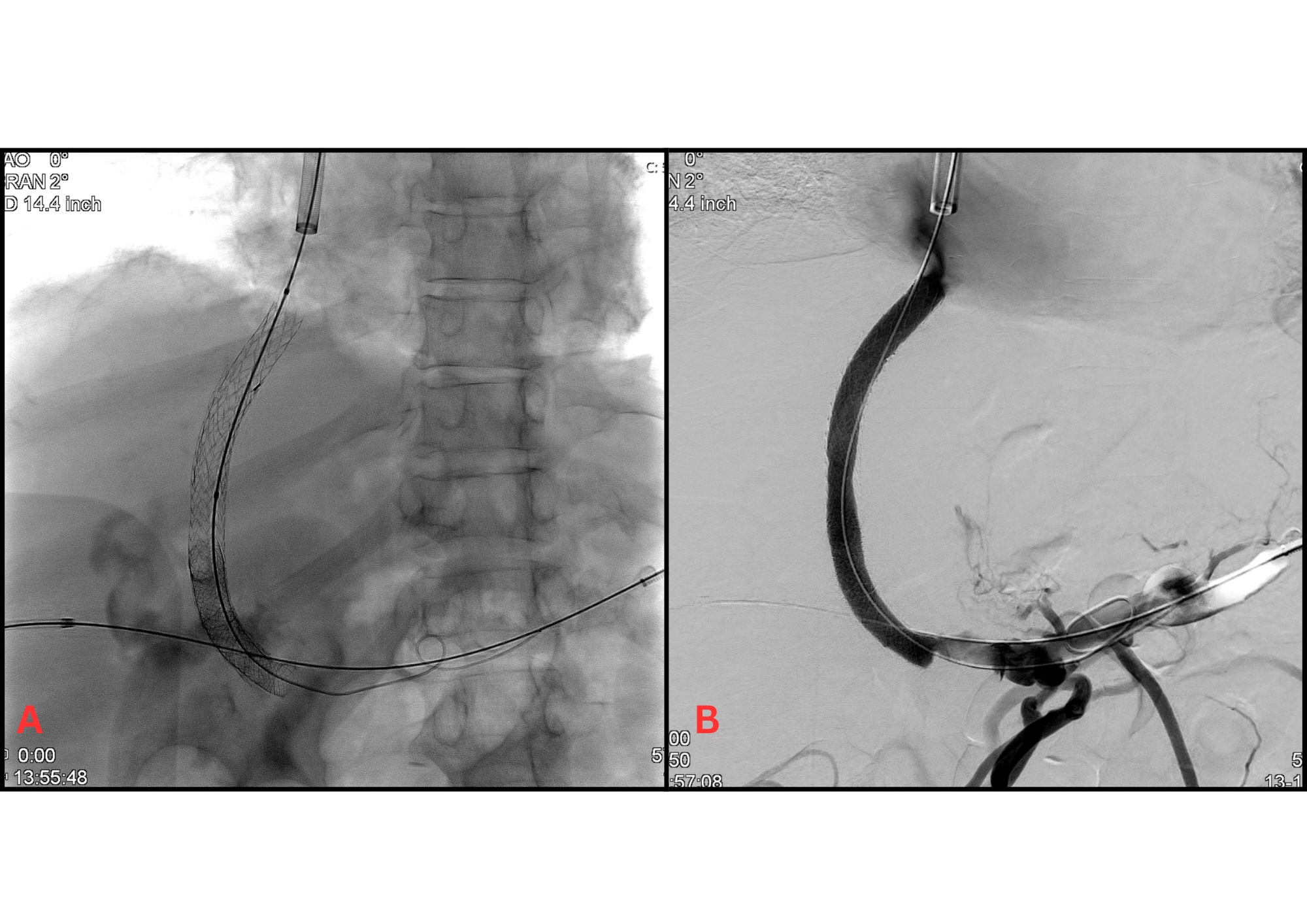
Figure: Figure 1.
(A) Fluoroscopic image demonstrating deployment of stent during transjugular intrahepatic portosystemic shunt (TIPS) placement.
(B) Contrast-enhanced imaging showing successful shunt creation with opacification of the portal venous system, including recanalization of the thrombosed portal vein and decompression of cavernous collaterals. The irregular contrast flow and network of collateral vessels in the portal vein region suggest cavernomatous transformation typical of chronic portal vein thrombosis
Disclosures:
Sneh Sonaiya indicated no relevant financial relationships.
Zan Ferrin indicated no relevant financial relationships.
Jiayi Ge indicated no relevant financial relationships.
Amol Koldhekar indicated no relevant financial relationships.
Vignan Manne indicated no relevant financial relationships.
Sneh Sonaiya, MD, MPH, MBA1, Zan Ferrin, DO2, Jiayi Ge, MD1, Amol Koldhekar, MD1, Vignan Manne, MD1. P4409 - A Rare Case of Portal Biliopathy in the Setting of Cavernomatous Transformation From Chronic Portal Vein Thrombosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
