Tuesday Poster Session
Category: Biliary/Pancreas
P4407 - Advanced Endoscopy Fallibility in Isolated IgG4-Related Cholangitis: A Case Spanning Borders Resolved Completely With Stenting and Steroids
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mahmoud Barbarawi, MD (he/him/his)
DHR Health in affiliation with University of Houston, Tilman J. Fertitta College of Medicine
McAllen, TX
Presenting Author(s)
Mahmoud Barbarawi, MD1, Jathniel Panneflek, MD1, Majdi Salahie, MD2, Zaid Barbarawi, MD3, Juan Sanchez, MD, FACG4
1DHR Health in affiliation with University of Houston, Tilman J. Fertitta College of Medicine, McAllen, TX; 2DHR Health, McAllen, TX; 3Jordan University of Science and Technology, McAllen, TX; 4DHR Health Gastroenterology, McAllen, TX
Introduction: Immunoglobulin G4-related sclerosing cholangitis (IgG4-SC) is an immune-mediated cholangiopathy that clinically and radiographically mimics cholangiocarcinoma. Isolated extra-pancreatic involvement is rare and difficult to distinguish from malignancy, particularly when initial pathology is inconclusive. Despite widespread reliance on ERCP, EUS, and cholangioscopy, these techniques often fall short when inflammation is focal and plasma cell-mediated.
Case Description/
Methods: A 59-year-old Hispanic man presented with progressive jaundice, 15-pound weight loss, and new-onset type 2 diabetes. He had been diagnosed abroad with presumed pancreatic cancer based on biliary imaging. In the U.S., CT and MRCP identified a dominant distal common bile duct stricture without a mass. Initial ERCP with balloon dilation, brushing, and biopsy was nondiagnostic. Cytology revealed only reactive changes. Subsequent EUS-FNB and SpyGlass-directed biopsy also failed to yield definitive findings. No pancreatic parenchymal or ductal abnormalities were observed.
After two months of evaluation, serum IgG4 results returned >4× the upper limit of normal. Pathology was re-reviewed and revealed storiform fibrosis, obliterative phlebitis, and >10 IgG4-positive plasma cells per high-power field. The diagnosis of isolated IgG4-SC was established. A prednisone taper (starting at 40 mg/day) was initiated. Follow-up ERCP at 4 months demonstrated substantial stricture improvement; at 7 months, cholangiography showed complete ductal resolution without the need for further stenting or immunosuppressive therapy.
Discussion: In dominant biliary strictures, the guiding principle is to consider malignancy until it is definitively excluded. This case required multiple high-yield sampling modalities - ERCP, SpyGlass, and EUS-FNB - before cancer could reasonably be ruled out. Allowing room to pursue the diagnosis of IgG4-SC. Despite access to advanced endoscopy, diagnosis remained elusive until serum IgG4 results prompted a retrospective pathology review. The absence of autoimmune pancreatitis further obscured the clinical picture. This case demonstrates that even the best procedural strategies may fall short in identifying rare inflammatory conditions. IgG4 testing and directed histologic reevaluation ultimately shifted the clinical trajectory, allowing for steroid therapy and full recovery without surgery.
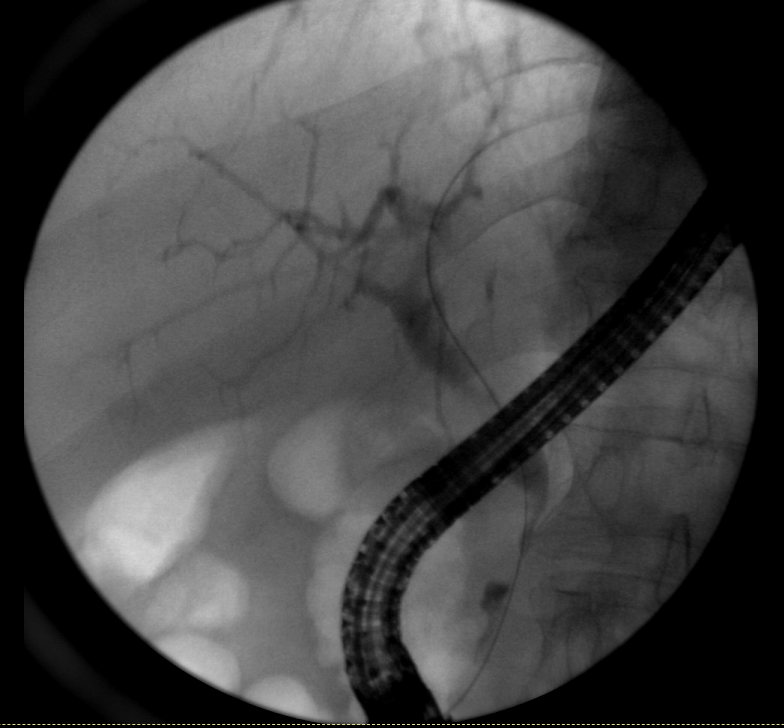
Figure: Figure 1 & 2: Initial ERCP and fluoroscopy demonstrating a dominant distal biliary stricture with upstream intrahepatic biliary dilation. Brushings and biopsies were inconclusive, and no pancreatic involvement was identified. Findings raised suspicion for malignancy but remained indeterminate.
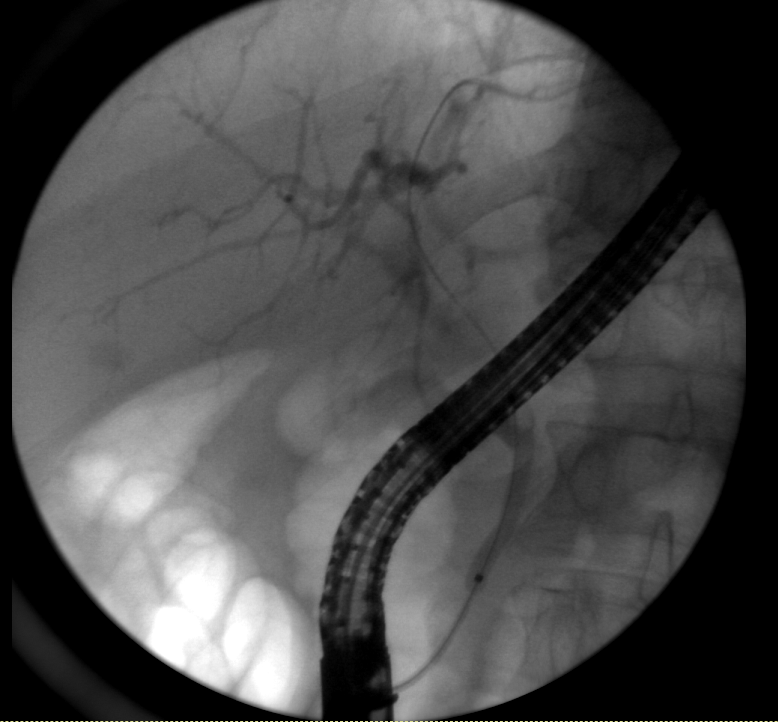
Figure: Figure 1 & 2: Initial ERCP and fluoroscopy demonstrating a dominant distal biliary stricture with upstream intrahepatic biliary dilation. Brushings and biopsies were inconclusive, and no pancreatic involvement was identified. Findings raised suspicion for malignancy but remained indeterminate.
Disclosures:
Mahmoud Barbarawi indicated no relevant financial relationships.
Jathniel Panneflek indicated no relevant financial relationships.
Majdi Salahie indicated no relevant financial relationships.
Zaid Barbarawi indicated no relevant financial relationships.
Juan Sanchez indicated no relevant financial relationships.
Mahmoud Barbarawi, MD1, Jathniel Panneflek, MD1, Majdi Salahie, MD2, Zaid Barbarawi, MD3, Juan Sanchez, MD, FACG4. P4407 - Advanced Endoscopy Fallibility in Isolated IgG4-Related Cholangitis: A Case Spanning Borders Resolved Completely With Stenting and Steroids, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1DHR Health in affiliation with University of Houston, Tilman J. Fertitta College of Medicine, McAllen, TX; 2DHR Health, McAllen, TX; 3Jordan University of Science and Technology, McAllen, TX; 4DHR Health Gastroenterology, McAllen, TX
Introduction: Immunoglobulin G4-related sclerosing cholangitis (IgG4-SC) is an immune-mediated cholangiopathy that clinically and radiographically mimics cholangiocarcinoma. Isolated extra-pancreatic involvement is rare and difficult to distinguish from malignancy, particularly when initial pathology is inconclusive. Despite widespread reliance on ERCP, EUS, and cholangioscopy, these techniques often fall short when inflammation is focal and plasma cell-mediated.
Case Description/
Methods: A 59-year-old Hispanic man presented with progressive jaundice, 15-pound weight loss, and new-onset type 2 diabetes. He had been diagnosed abroad with presumed pancreatic cancer based on biliary imaging. In the U.S., CT and MRCP identified a dominant distal common bile duct stricture without a mass. Initial ERCP with balloon dilation, brushing, and biopsy was nondiagnostic. Cytology revealed only reactive changes. Subsequent EUS-FNB and SpyGlass-directed biopsy also failed to yield definitive findings. No pancreatic parenchymal or ductal abnormalities were observed.
After two months of evaluation, serum IgG4 results returned >4× the upper limit of normal. Pathology was re-reviewed and revealed storiform fibrosis, obliterative phlebitis, and >10 IgG4-positive plasma cells per high-power field. The diagnosis of isolated IgG4-SC was established. A prednisone taper (starting at 40 mg/day) was initiated. Follow-up ERCP at 4 months demonstrated substantial stricture improvement; at 7 months, cholangiography showed complete ductal resolution without the need for further stenting or immunosuppressive therapy.
Discussion: In dominant biliary strictures, the guiding principle is to consider malignancy until it is definitively excluded. This case required multiple high-yield sampling modalities - ERCP, SpyGlass, and EUS-FNB - before cancer could reasonably be ruled out. Allowing room to pursue the diagnosis of IgG4-SC. Despite access to advanced endoscopy, diagnosis remained elusive until serum IgG4 results prompted a retrospective pathology review. The absence of autoimmune pancreatitis further obscured the clinical picture. This case demonstrates that even the best procedural strategies may fall short in identifying rare inflammatory conditions. IgG4 testing and directed histologic reevaluation ultimately shifted the clinical trajectory, allowing for steroid therapy and full recovery without surgery.
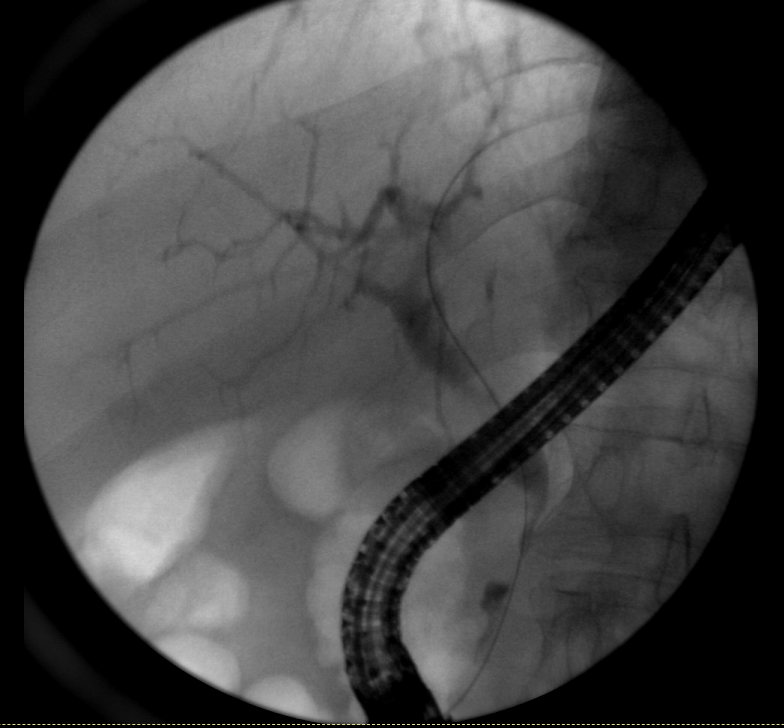
Figure: Figure 1 & 2: Initial ERCP and fluoroscopy demonstrating a dominant distal biliary stricture with upstream intrahepatic biliary dilation. Brushings and biopsies were inconclusive, and no pancreatic involvement was identified. Findings raised suspicion for malignancy but remained indeterminate.
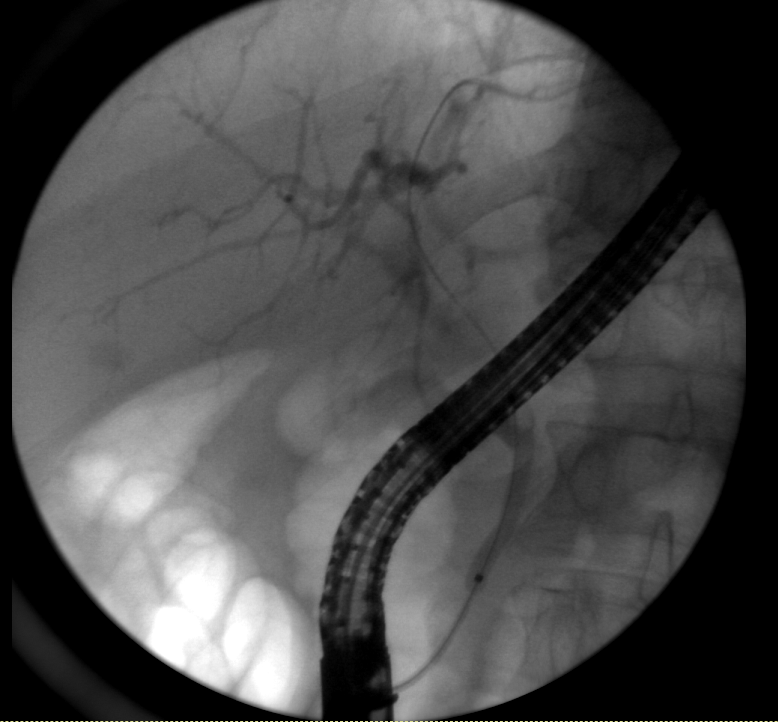
Figure: Figure 1 & 2: Initial ERCP and fluoroscopy demonstrating a dominant distal biliary stricture with upstream intrahepatic biliary dilation. Brushings and biopsies were inconclusive, and no pancreatic involvement was identified. Findings raised suspicion for malignancy but remained indeterminate.
Disclosures:
Mahmoud Barbarawi indicated no relevant financial relationships.
Jathniel Panneflek indicated no relevant financial relationships.
Majdi Salahie indicated no relevant financial relationships.
Zaid Barbarawi indicated no relevant financial relationships.
Juan Sanchez indicated no relevant financial relationships.
Mahmoud Barbarawi, MD1, Jathniel Panneflek, MD1, Majdi Salahie, MD2, Zaid Barbarawi, MD3, Juan Sanchez, MD, FACG4. P4407 - Advanced Endoscopy Fallibility in Isolated IgG4-Related Cholangitis: A Case Spanning Borders Resolved Completely With Stenting and Steroids, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
