Tuesday Poster Session
Category: Biliary/Pancreas
P4406 - Atypical Ascites in a Cirrhotic Patient: Diagnostic Utility of Bilirubin Ratio
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- BA
Balakrishnan Arivalagan, MD (he/him/his)
BronxCare Health System
New York, FL
Presenting Author(s)
Balakrishnan Arivalagan, MD1, Fnu Veena, MD1, Sahil Dudhat, MD2, Franklin Sosa, MD1, Priscilla Lajara, MD3, Rayan Faisal Grib Alataa, MD1, Mikhail Sukhoroslov, MD1, Harish Patel, MD3
1BronxCare Health System, New York, NY; 2BRONX CARE HEALTH SYSTEM, Bronx, NY; 3BronxCare Health System, Bronx, NY
Introduction: Ascites, the pathological accumulation of fluid within the peritoneal cavity, is most associated with portal hypertension in cirrhotic patients. Analysis of ascitic fluid including serum-ascites albumin gradient (SAAG), cell count, and visual inspection plays a key role in identifying underlying etiology. Biliary ascites, though rare, should be considered when fluid appearance is atypical, particularly greenish or brownish.
Case Description/
Methods: We present a case of a 64-year-old cirrhotic male (Child-Pugh B), likely secondary to metabolic-associated steatohepatitis (MASH), with a history of TIPS placement for variceal bleeding, coronary artery disease, and obstructive sleep apnea was admitted for altered mentation. Laboratory findings included leukocytosis, mild hyperbilirubinemia, and preserved liver function shown in Table 1. CT imaging revealed moderate ascites, gallstones, and cholecystitis. Paracentesis showed brown fluid with low SAAG, PMN count >250/mm³, and an ascitic bilirubin of 1.9 mg/dL. Cultures were sterile. He received antibiotics and underwent percutaneous cholecystostomy using a 10F catheter, which was later dislodged spontaneously. Given clinical instability and poor surgical candidacy, the tube was not replaced. Eight weeks later, the patient redeveloped ascites. Repeat paracentesis revealed green fluid (as in Figure 1) with a PMN count >250/mm³ and an ascitic bilirubin of 2.8 mg/dL (serum bilirubin 2.7 mg/dL), yielding an ascitic-to-serum bilirubin ratio >1 suggestive of biliary ascites as in Table 2. Imaging did not reveal pneumoperitoneum. Due to worsening clinical status and comorbidities, the patient was transitioned to palliative care per his previously stated wishes.
Discussion: Biliary ascites results from bile leakage into the peritoneal cavity, typically due to bile duct injury, gallbladder perforation, or post-interventional complications. A greenish hue and an ascitic-to-serum bilirubin ratio >1 are diagnostic clues (1,2). This case highlights a delayed presentation of biliary peritonitis potentially related to spontaneous dislodgement of a small-bore cholecystostomy tube. Although conservative management may be acceptable initially, delayed complications can occur and warrant close follow-up.
References
1. Blank J, Anderson E, Mansoor AM. Biliary Ascites. J Gen Intern Med. 2022.
2. Lee CM, Stewart L, Way LW. Post cholecystectomy Abdominal Bile Collections. Arch Surg. 2000;135(5):538–544

Figure: Fig A: Paracentesis drain showing greenish ascitic fluid collection
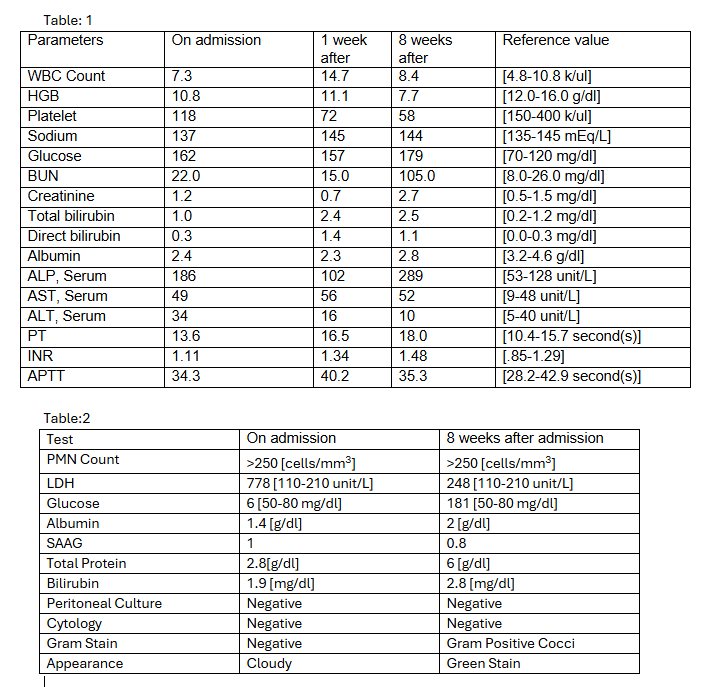
Figure: Table: 1 Laboratory investigations
Table:2 Ascitic Fluid Analysis
PMN Count= Polymorphonuclear leukocytes
LDH= Lactate dehydrogenase
AST=Aspartate transaminase
ALT=Alanine transaminase
ALP=Alkaline phosphatase
BUN=Blood Urea Nitrogen
WBC=White blood count
HGB=Hemoglobin
PT= Prothrombin Time
APTT= Activated Partial Thromboplastin Time
INR=International Normalized Ratio
Disclosures:
Balakrishnan Arivalagan indicated no relevant financial relationships.
Fnu Veena indicated no relevant financial relationships.
Sahil Dudhat indicated no relevant financial relationships.
Franklin Sosa indicated no relevant financial relationships.
Priscilla Lajara indicated no relevant financial relationships.
Rayan Faisal Grib Alataa indicated no relevant financial relationships.
Mikhail Sukhoroslov indicated no relevant financial relationships.
Harish Patel indicated no relevant financial relationships.
Balakrishnan Arivalagan, MD1, Fnu Veena, MD1, Sahil Dudhat, MD2, Franklin Sosa, MD1, Priscilla Lajara, MD3, Rayan Faisal Grib Alataa, MD1, Mikhail Sukhoroslov, MD1, Harish Patel, MD3. P4406 - Atypical Ascites in a Cirrhotic Patient: Diagnostic Utility of Bilirubin Ratio, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1BronxCare Health System, New York, NY; 2BRONX CARE HEALTH SYSTEM, Bronx, NY; 3BronxCare Health System, Bronx, NY
Introduction: Ascites, the pathological accumulation of fluid within the peritoneal cavity, is most associated with portal hypertension in cirrhotic patients. Analysis of ascitic fluid including serum-ascites albumin gradient (SAAG), cell count, and visual inspection plays a key role in identifying underlying etiology. Biliary ascites, though rare, should be considered when fluid appearance is atypical, particularly greenish or brownish.
Case Description/
Methods: We present a case of a 64-year-old cirrhotic male (Child-Pugh B), likely secondary to metabolic-associated steatohepatitis (MASH), with a history of TIPS placement for variceal bleeding, coronary artery disease, and obstructive sleep apnea was admitted for altered mentation. Laboratory findings included leukocytosis, mild hyperbilirubinemia, and preserved liver function shown in Table 1. CT imaging revealed moderate ascites, gallstones, and cholecystitis. Paracentesis showed brown fluid with low SAAG, PMN count >250/mm³, and an ascitic bilirubin of 1.9 mg/dL. Cultures were sterile. He received antibiotics and underwent percutaneous cholecystostomy using a 10F catheter, which was later dislodged spontaneously. Given clinical instability and poor surgical candidacy, the tube was not replaced. Eight weeks later, the patient redeveloped ascites. Repeat paracentesis revealed green fluid (as in Figure 1) with a PMN count >250/mm³ and an ascitic bilirubin of 2.8 mg/dL (serum bilirubin 2.7 mg/dL), yielding an ascitic-to-serum bilirubin ratio >1 suggestive of biliary ascites as in Table 2. Imaging did not reveal pneumoperitoneum. Due to worsening clinical status and comorbidities, the patient was transitioned to palliative care per his previously stated wishes.
Discussion: Biliary ascites results from bile leakage into the peritoneal cavity, typically due to bile duct injury, gallbladder perforation, or post-interventional complications. A greenish hue and an ascitic-to-serum bilirubin ratio >1 are diagnostic clues (1,2). This case highlights a delayed presentation of biliary peritonitis potentially related to spontaneous dislodgement of a small-bore cholecystostomy tube. Although conservative management may be acceptable initially, delayed complications can occur and warrant close follow-up.
References
1. Blank J, Anderson E, Mansoor AM. Biliary Ascites. J Gen Intern Med. 2022.
2. Lee CM, Stewart L, Way LW. Post cholecystectomy Abdominal Bile Collections. Arch Surg. 2000;135(5):538–544

Figure: Fig A: Paracentesis drain showing greenish ascitic fluid collection
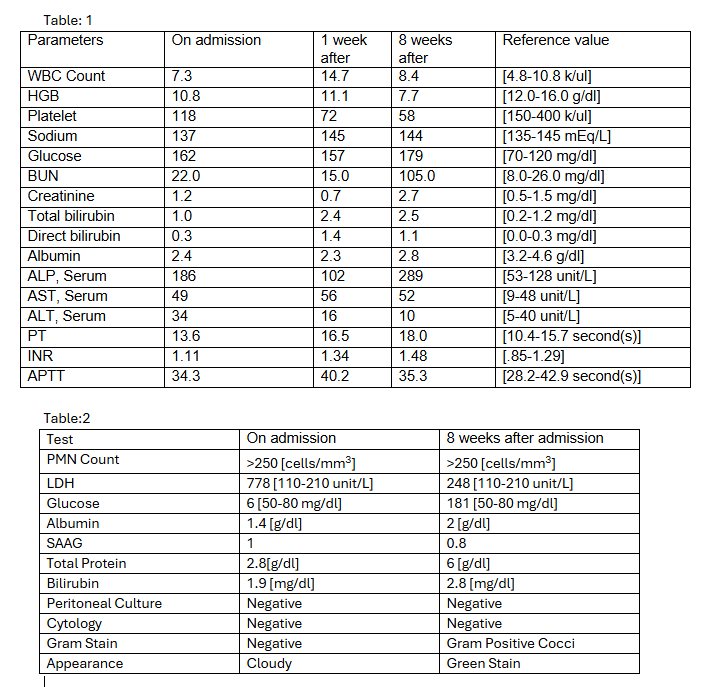
Figure: Table: 1 Laboratory investigations
Table:2 Ascitic Fluid Analysis
PMN Count= Polymorphonuclear leukocytes
LDH= Lactate dehydrogenase
AST=Aspartate transaminase
ALT=Alanine transaminase
ALP=Alkaline phosphatase
BUN=Blood Urea Nitrogen
WBC=White blood count
HGB=Hemoglobin
PT= Prothrombin Time
APTT= Activated Partial Thromboplastin Time
INR=International Normalized Ratio
Disclosures:
Balakrishnan Arivalagan indicated no relevant financial relationships.
Fnu Veena indicated no relevant financial relationships.
Sahil Dudhat indicated no relevant financial relationships.
Franklin Sosa indicated no relevant financial relationships.
Priscilla Lajara indicated no relevant financial relationships.
Rayan Faisal Grib Alataa indicated no relevant financial relationships.
Mikhail Sukhoroslov indicated no relevant financial relationships.
Harish Patel indicated no relevant financial relationships.
Balakrishnan Arivalagan, MD1, Fnu Veena, MD1, Sahil Dudhat, MD2, Franklin Sosa, MD1, Priscilla Lajara, MD3, Rayan Faisal Grib Alataa, MD1, Mikhail Sukhoroslov, MD1, Harish Patel, MD3. P4406 - Atypical Ascites in a Cirrhotic Patient: Diagnostic Utility of Bilirubin Ratio, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

