Tuesday Poster Session
Category: Biliary/Pancreas
P4393 - Mycotic Cholangitis in Immunocompetent Adult: A Case Report
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

George Sarin Zacharia, MD (he/him/his)
BronxCare Health System
New York, NY
Presenting Author(s)
George Sarin Zacharia, MD1, Mathew V. Lazar, DM2, Franklin Sosa, MD3, Raul Reina, MD1
1BronxCare Health System, New York, NY; 2Lifecare Hospital, Abu Dhabi, Abu Dhabi, United Arab Emirates; 3BronxCare Health System, Bronx, NY
Introduction: Cholangitis is a severe infection often resulting from biliary obstruction, typically due to choledocholithiasis or strictures. Gram-negative enteric bacteria are the most common pathogens. Fungal cholangitis is a rare condition that affects typically individuals who are immunocompromised or those with indwelling biliary stents. We report a rare case of Candida albicans cholangitis in an immunocompetent individual presenting with acute pancreatitis and septic shock.
Case Description/
Methods: A 52-year-old previously healthy male presented with three days of severe epigastric pain, nausea, vomiting, and intolerance to oral intake. He had no past medical history or immunosuppressive risk factors. At presentation, he was hypoxic (SpO₂ 88% on NRB), tachypneic, and in respiratory distress, requiring intubation. Labs showed leukopenia, elevated liver enzymes, and high lipase. CT abdomen revealed Balthazar grade C pancreatitis, CBD dilatation (10 mm), and possible distal obstruction. ERCP demonstrated a distal CBD cut-off with purulent drainage; a 7Fr stent was placed. Blood and bile cultures grew Candida albicans sensitive to fluconazole, echinocandins, and amphotericin B. IV caspofungin was initiated. Over the course of one week, clinical and biochemical improvements occurred, allowing for extubation and cessation of vasopressors. The patient was discharged, and stent removal was performed two weeks later. He remained asymptomatic during 6-month follow-up.
Discussion: Fungal cholangitis is an uncommon but serious infection typically seen in immunosuppressed individuals or those with prolonged antibiotic use, biliary stents, or intensive care unit (ICU) stays. Candida albicans is the most frequently isolated fungal organism. While colonization can occur, actual infection is suggested by clinical deterioration and the presence of candidemia. This case is unique due to the absence of classical risk factors. Notably, the patient was not evaluated for rare immunodeficiency syndromes but lacked suggestive clinical features.
In conclusion, Candidal cholangitis should be considered in critically ill patients with cholangitis, even in the absence of traditional risk factors for candidal infections. Prompt diagnosis, source control, and antifungal therapy are critical. This case highlights the evolving spectrum of biliary infections and underscores the importance of heightened awareness of fungal pathogens in atypical settings.
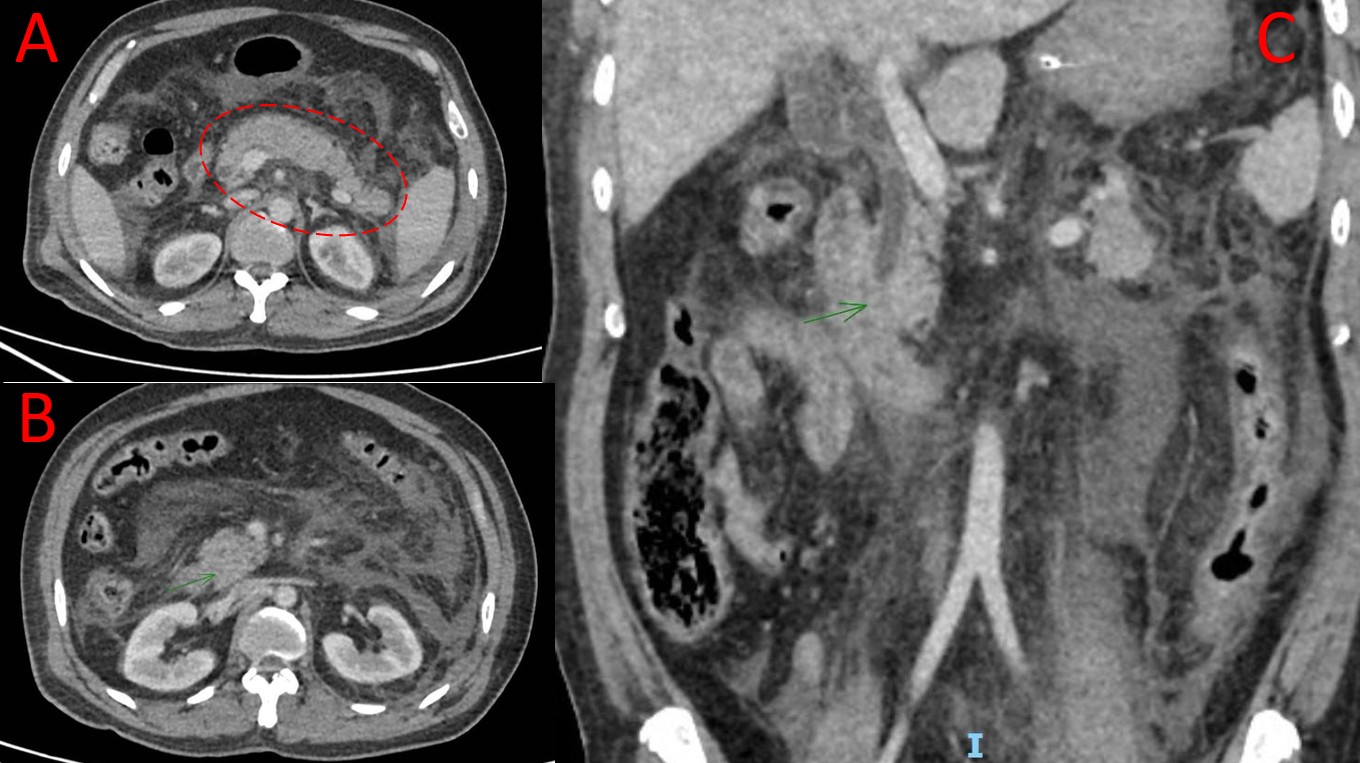
Figure: CECT abdomen. (A) Edematous pancreas with normal post-contrast enhancement and peripancreatic fat stranding; suggestive of acute pancreatitis. (B) Dilated CBD with a maximum caliber measuring about 10 mm at mid-level and intraluminal sludge versus small calculi. (C) Coronal image demonstrating dilated CBD with a distal cut-off.
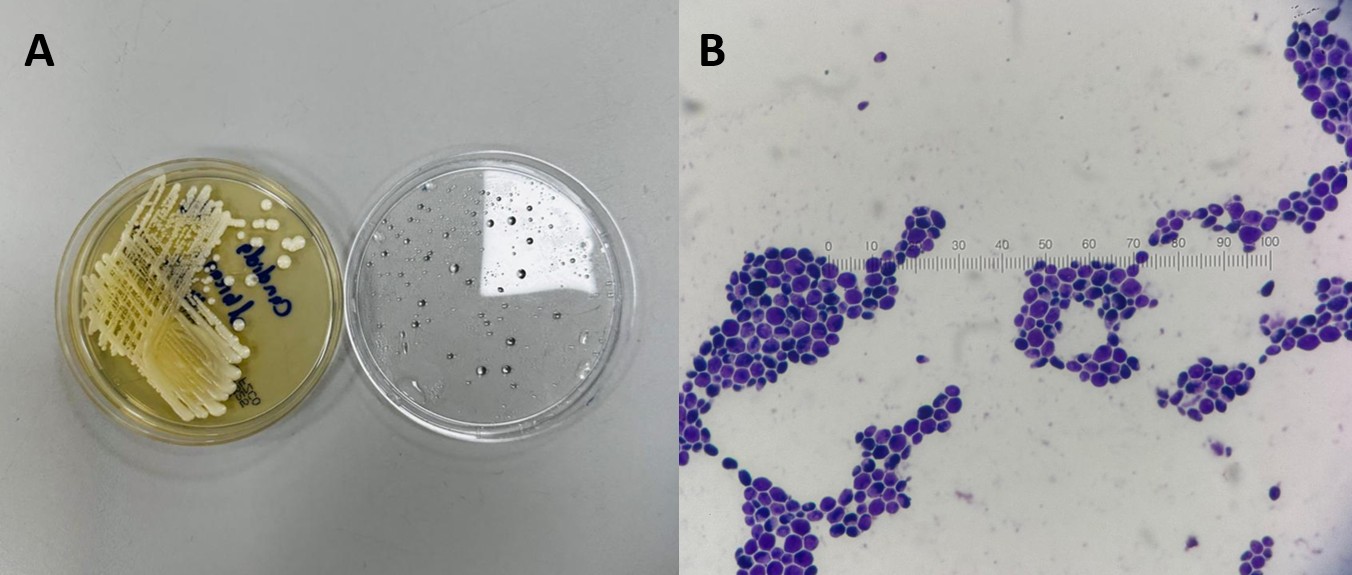
Figure: (A) White pasty colonies on Sabouraud’s dextrose agar after 48 hours of incubation. (B) Oval gram-positive budding yeast cells
Disclosures:
George Sarin Zacharia indicated no relevant financial relationships.
Mathew Lazar indicated no relevant financial relationships.
Franklin Sosa indicated no relevant financial relationships.
Raul Reina indicated no relevant financial relationships.
George Sarin Zacharia, MD1, Mathew V. Lazar, DM2, Franklin Sosa, MD3, Raul Reina, MD1. P4393 - Mycotic Cholangitis in Immunocompetent Adult: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1BronxCare Health System, New York, NY; 2Lifecare Hospital, Abu Dhabi, Abu Dhabi, United Arab Emirates; 3BronxCare Health System, Bronx, NY
Introduction: Cholangitis is a severe infection often resulting from biliary obstruction, typically due to choledocholithiasis or strictures. Gram-negative enteric bacteria are the most common pathogens. Fungal cholangitis is a rare condition that affects typically individuals who are immunocompromised or those with indwelling biliary stents. We report a rare case of Candida albicans cholangitis in an immunocompetent individual presenting with acute pancreatitis and septic shock.
Case Description/
Methods: A 52-year-old previously healthy male presented with three days of severe epigastric pain, nausea, vomiting, and intolerance to oral intake. He had no past medical history or immunosuppressive risk factors. At presentation, he was hypoxic (SpO₂ 88% on NRB), tachypneic, and in respiratory distress, requiring intubation. Labs showed leukopenia, elevated liver enzymes, and high lipase. CT abdomen revealed Balthazar grade C pancreatitis, CBD dilatation (10 mm), and possible distal obstruction. ERCP demonstrated a distal CBD cut-off with purulent drainage; a 7Fr stent was placed. Blood and bile cultures grew Candida albicans sensitive to fluconazole, echinocandins, and amphotericin B. IV caspofungin was initiated. Over the course of one week, clinical and biochemical improvements occurred, allowing for extubation and cessation of vasopressors. The patient was discharged, and stent removal was performed two weeks later. He remained asymptomatic during 6-month follow-up.
Discussion: Fungal cholangitis is an uncommon but serious infection typically seen in immunosuppressed individuals or those with prolonged antibiotic use, biliary stents, or intensive care unit (ICU) stays. Candida albicans is the most frequently isolated fungal organism. While colonization can occur, actual infection is suggested by clinical deterioration and the presence of candidemia. This case is unique due to the absence of classical risk factors. Notably, the patient was not evaluated for rare immunodeficiency syndromes but lacked suggestive clinical features.
In conclusion, Candidal cholangitis should be considered in critically ill patients with cholangitis, even in the absence of traditional risk factors for candidal infections. Prompt diagnosis, source control, and antifungal therapy are critical. This case highlights the evolving spectrum of biliary infections and underscores the importance of heightened awareness of fungal pathogens in atypical settings.
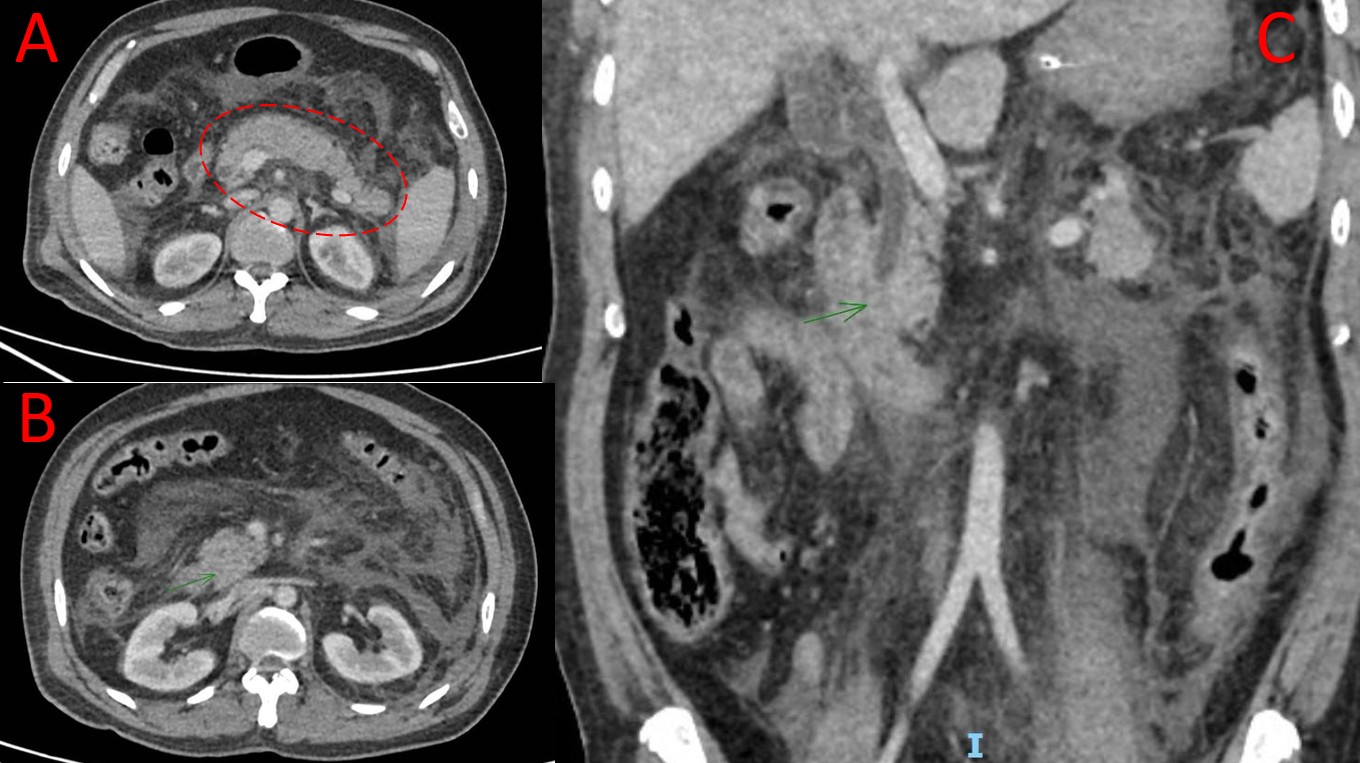
Figure: CECT abdomen. (A) Edematous pancreas with normal post-contrast enhancement and peripancreatic fat stranding; suggestive of acute pancreatitis. (B) Dilated CBD with a maximum caliber measuring about 10 mm at mid-level and intraluminal sludge versus small calculi. (C) Coronal image demonstrating dilated CBD with a distal cut-off.
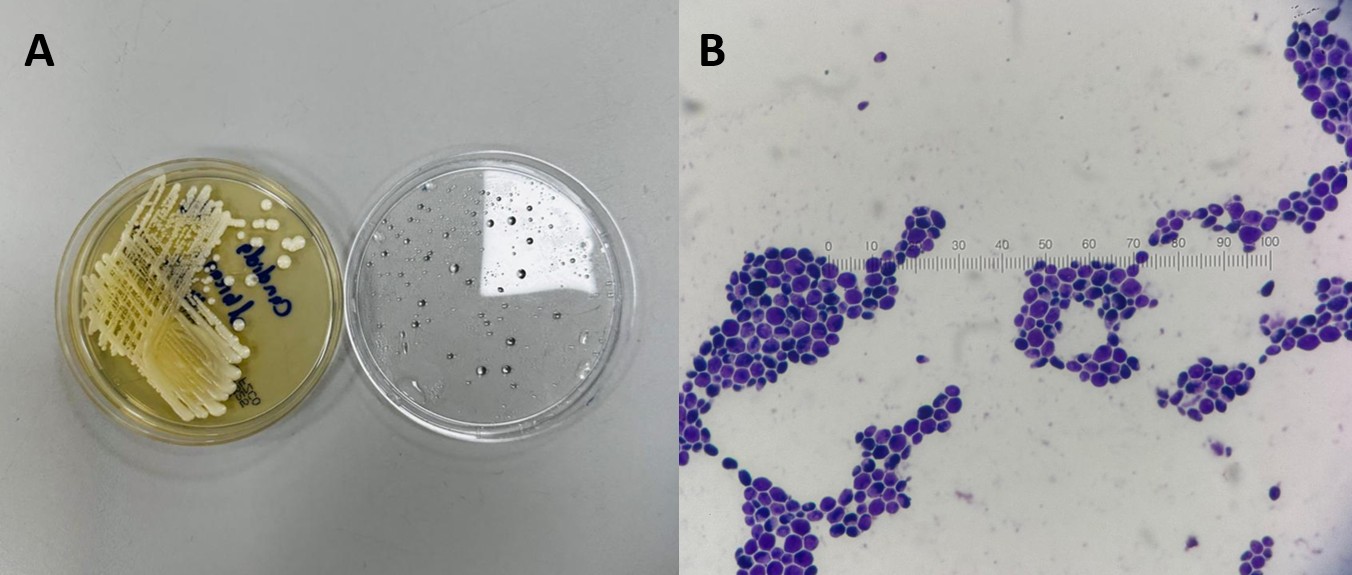
Figure: (A) White pasty colonies on Sabouraud’s dextrose agar after 48 hours of incubation. (B) Oval gram-positive budding yeast cells
Disclosures:
George Sarin Zacharia indicated no relevant financial relationships.
Mathew Lazar indicated no relevant financial relationships.
Franklin Sosa indicated no relevant financial relationships.
Raul Reina indicated no relevant financial relationships.
George Sarin Zacharia, MD1, Mathew V. Lazar, DM2, Franklin Sosa, MD3, Raul Reina, MD1. P4393 - Mycotic Cholangitis in Immunocompetent Adult: A Case Report, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

