Tuesday Poster Session
Category: Biliary/Pancreas
P4392 - Pancreatic Fistulas Involving the Portal Vein and Pleural Space: Two Case Reports on Complex Presentations and Management
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MA
Mohamed Alharami, MD (he/him/his)
Henry Ford Warren
Warren, MI
Presenting Author(s)
Mohamed Alharami, MD1, Ziad Suleiman, MD2, Omar Alwan, MD3, Frhaan Zahrawi, MBBCh4, Hadi Hemaidan, MS5, Omar Khattab, MD6
1Henry Ford Warren, Warren, MI; 2Southwest healthcare medical education consortium, Murrieta, CA; 3Hamilton Medical Center, Dalton, GA; 4Franciscan Health Olympia Fields, Olympia Fields, IL; 5Florida International University, Daytona Beach, FL; 6Kettering Health Netwrok, Kettering, OH
Introduction: A rare yet serious complication of pancreatitis is fistula formation. Pancreatic fistula (PF) develops as the integrity of the pancreatic ductal system gets disrupted by parenchymal inflammation, causing leakage of pancreatic secretions into nearby tissues. The clinical presentation varies depending on the anatomical destination of the fistula, often appearing atypically and making diagnosis and management difficult.
Case Description/
Methods: Case 1: A 59-year-old male patient with chronic idiopathic pancreatitis developed a pancreatic–pleural fistula (PPF), presenting as a massive, recurrent right-sided pleural effusion (Figure 1A). Thoracentesis revealed an elevated pleural fluid lipase level, and the diagnosis was confirmed by imaging and ERCP demonstrating a pancreatic duct leak into the pleural space via a sinus tract extending from the pancreas to the mediastinum. The patient underwent thoracic surgical intervention together with multiple chest tube placements and endoscopic stenting.
Case 2: A 52-year-old male with a history of chronic alcoholic pancreatitis presented with worsening abdominal pain. Imaging revealed extensive portal vein thrombosis, and despite anticoagulant therapy, thrombosis continued to worsen (Figure 1B). Further evaluation revealed a rare pancreatic–portal vein fistula (PPVF). The diagnosis became evident through imaging and intraoperative portal system contrast injection, which opacified a pancreatic pseudocyst, confirming pancreaticoportal communication (Figure 1C). The patient needed multiple endoscopic stent placements, cystogastrostomy, and an extended course of anticoagulant therapy.
Discussion: PPVF and PPF are rare, diagnostically challenging, and therapeutically complex complications of pancreatitis. In both cases, fistula-related symptoms preceded radiologic evidence of the fistula, contributing to delays in diagnosis and definitive treatment. This diagnostic lag, coupled with the severity of associated complications, such as portal vein thrombosis and recurrent pleural effusion, leads to substantial morbidity and mortality risk in PF cases. In patients with a long-standing history of pancreatitis who present atypically, pancreatic fistula should be considered in the differential diagnosis. Early recognition allows a prompt and specific treatment approach, which decreases patient complications and enhances their clinical outcomes.
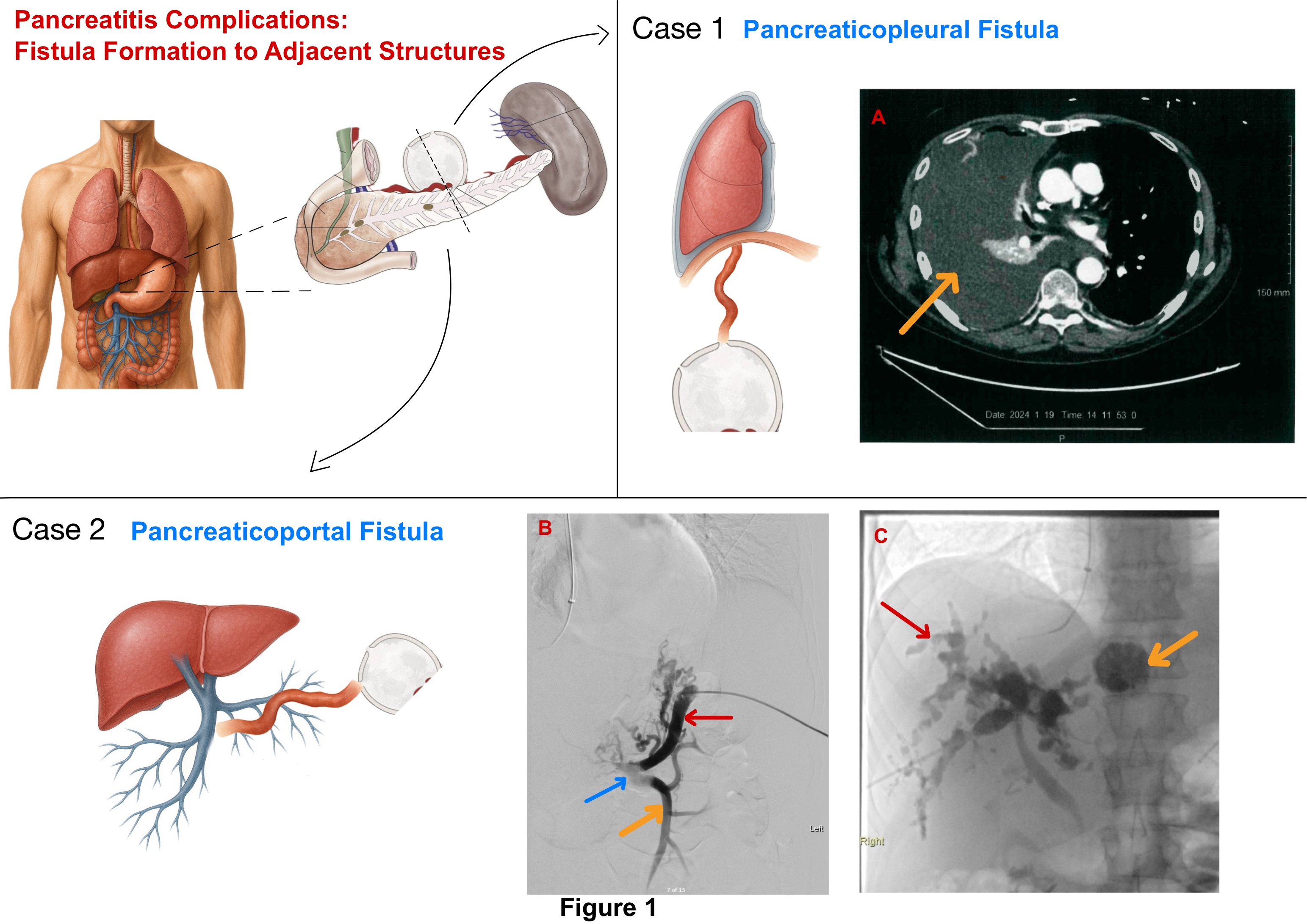
Figure: A. Axial CT scan of the chest showing massive right-sided pleural effusion (orange arrow) secondary to a pancreaticopleural fistula.
B. Venography showing the splenic vein (red arrow), superior mesenteric vein (orange arrow), and massive thrombosis at the portal vein confluence (blue arrow).
C. Venography demonstrating an amorphous portal venous system (red arrow) with contrast leakage into a peripancreatic pseudocyst (orange arrow).
Disclosures:
Mohamed Alharami indicated no relevant financial relationships.
Ziad Suleiman indicated no relevant financial relationships.
Omar Alwan indicated no relevant financial relationships.
Frhaan Zahrawi indicated no relevant financial relationships.
Hadi Hemaidan indicated no relevant financial relationships.
Omar Khattab indicated no relevant financial relationships.
Mohamed Alharami, MD1, Ziad Suleiman, MD2, Omar Alwan, MD3, Frhaan Zahrawi, MBBCh4, Hadi Hemaidan, MS5, Omar Khattab, MD6. P4392 - Pancreatic Fistulas Involving the Portal Vein and Pleural Space: Two Case Reports on Complex Presentations and Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Warren, Warren, MI; 2Southwest healthcare medical education consortium, Murrieta, CA; 3Hamilton Medical Center, Dalton, GA; 4Franciscan Health Olympia Fields, Olympia Fields, IL; 5Florida International University, Daytona Beach, FL; 6Kettering Health Netwrok, Kettering, OH
Introduction: A rare yet serious complication of pancreatitis is fistula formation. Pancreatic fistula (PF) develops as the integrity of the pancreatic ductal system gets disrupted by parenchymal inflammation, causing leakage of pancreatic secretions into nearby tissues. The clinical presentation varies depending on the anatomical destination of the fistula, often appearing atypically and making diagnosis and management difficult.
Case Description/
Methods: Case 1: A 59-year-old male patient with chronic idiopathic pancreatitis developed a pancreatic–pleural fistula (PPF), presenting as a massive, recurrent right-sided pleural effusion (Figure 1A). Thoracentesis revealed an elevated pleural fluid lipase level, and the diagnosis was confirmed by imaging and ERCP demonstrating a pancreatic duct leak into the pleural space via a sinus tract extending from the pancreas to the mediastinum. The patient underwent thoracic surgical intervention together with multiple chest tube placements and endoscopic stenting.
Case 2: A 52-year-old male with a history of chronic alcoholic pancreatitis presented with worsening abdominal pain. Imaging revealed extensive portal vein thrombosis, and despite anticoagulant therapy, thrombosis continued to worsen (Figure 1B). Further evaluation revealed a rare pancreatic–portal vein fistula (PPVF). The diagnosis became evident through imaging and intraoperative portal system contrast injection, which opacified a pancreatic pseudocyst, confirming pancreaticoportal communication (Figure 1C). The patient needed multiple endoscopic stent placements, cystogastrostomy, and an extended course of anticoagulant therapy.
Discussion: PPVF and PPF are rare, diagnostically challenging, and therapeutically complex complications of pancreatitis. In both cases, fistula-related symptoms preceded radiologic evidence of the fistula, contributing to delays in diagnosis and definitive treatment. This diagnostic lag, coupled with the severity of associated complications, such as portal vein thrombosis and recurrent pleural effusion, leads to substantial morbidity and mortality risk in PF cases. In patients with a long-standing history of pancreatitis who present atypically, pancreatic fistula should be considered in the differential diagnosis. Early recognition allows a prompt and specific treatment approach, which decreases patient complications and enhances their clinical outcomes.
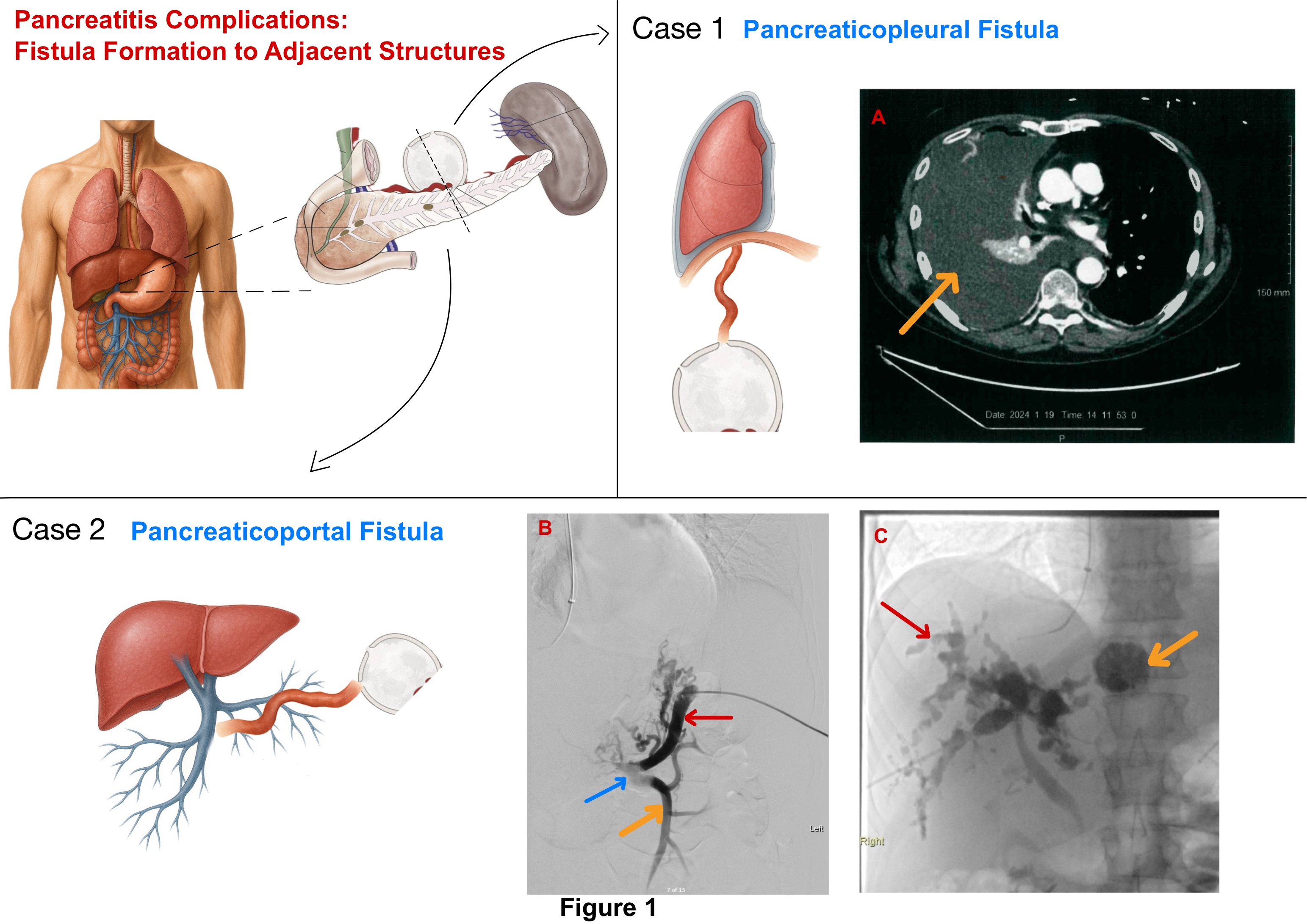
Figure: A. Axial CT scan of the chest showing massive right-sided pleural effusion (orange arrow) secondary to a pancreaticopleural fistula.
B. Venography showing the splenic vein (red arrow), superior mesenteric vein (orange arrow), and massive thrombosis at the portal vein confluence (blue arrow).
C. Venography demonstrating an amorphous portal venous system (red arrow) with contrast leakage into a peripancreatic pseudocyst (orange arrow).
Disclosures:
Mohamed Alharami indicated no relevant financial relationships.
Ziad Suleiman indicated no relevant financial relationships.
Omar Alwan indicated no relevant financial relationships.
Frhaan Zahrawi indicated no relevant financial relationships.
Hadi Hemaidan indicated no relevant financial relationships.
Omar Khattab indicated no relevant financial relationships.
Mohamed Alharami, MD1, Ziad Suleiman, MD2, Omar Alwan, MD3, Frhaan Zahrawi, MBBCh4, Hadi Hemaidan, MS5, Omar Khattab, MD6. P4392 - Pancreatic Fistulas Involving the Portal Vein and Pleural Space: Two Case Reports on Complex Presentations and Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
